Abstract
State-level marijuana liberalization policies have been evolving for the past five decades, and yet the overall scientific evidence of the impact of these policies is widely believed to be inconclusive. In this review we summarize some of the key limitations of the studies evaluating the effects of decriminalization and medical marijuana laws on marijuana use, highlighting their inconsistencies in terms of the heterogeneity of policies, the timing of the evaluations, and the measures of use being considered. We suggest that the heterogeneity in the responsiveness of different populations to particular laws is important for interpreting the mixed findings from the literature, and we highlight the limitations of the existing literature in providing clear insights into the probable effects of marijuana legalization.
Keywords: marijuana liberalization, marijuana products, policy dynamics, policy heterogeneity
INTRODUCTION
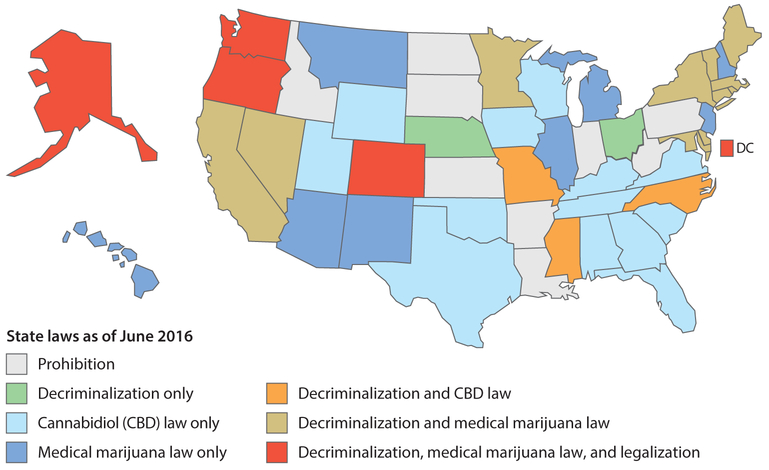
Although the federal law has prohibited the use and distribution of marijuana in the United States since 1937, for the past five decades states have been experimenting with marijuana liberalization polices. State decriminalization policies were first passed in the 1970s, patient medical access laws began to get adopted in the 1990s, and more recently states have been experimenting with legalization of recreational markets. This has resulted in a spectrum of marijuana liberalization policies across the United States that is often not fully recognized or considered when conducting evaluations of recent policy changes. Consider for example the state of marijuana policies in the United States at a single point of time. As shown in Figure 1, as of January 1, 2016, 21 states1 have decriminalized certain marijuana possession offenses (NCSL 2016a), 26 states have legalized medical marijuana use, and another 16 states have adopted cannabidiol (CBD)-only laws (NCSL 2016b) that protect only certain strains of marijuana to be used for medicinal purposes. However, there is tremendous overlap because some states have implemented combinations of each of these policies, as shown by the fact that the five states currently legalizing recreational marijuana use (Alaska, Colorado, Oregon, Washington, and the District of Columbia) all initially decriminalized marijuana and then passed medical marijuana allowances before passing their legalization policies. Thus, the vast majority of US states have moved away from a strict prohibition position toward marijuana well before they started considering outright legalization.
Figure 1.
State marijuana policies as of January 1, 2016. Data from the RAND Marijuana Policy Database (Pacula et al. 2015) and NCSL (2016a,b) with permission. Abbreviation: CBD, cannabidiol.
A number of factors have driven the policy changes observed over the past several decades, including rising state budgetary costs associated with arresting and incarcerating nonviolent drug offenders (Raphael & Stoll 2013, Reuter et al. 2001), growing scientific evidence of the therapeutic benefits of cannabinoids found in the marijuana plant (Hill 2015, Koppel et al. 2014), and strained state budgets that have caused legislatures to look for new sources of tax revenue (Caulkins et al. 2015, Kilmer et al. 2010).
The tremendous policy variation over time and across states would appear to give researchers ample opportunities to quantitatively assess the effect of marijuana liberalization policies on a variety of health and social outcomes. However, the scientific literature has been slow to develop, and what exists in the literature offers generally mixed and largely insignificant findings. This has led many to conclude that the previous liberalization policies must be harmless and that ongoing legalization would similarly generate very little harm to society. Indeed, recent surveys of people’s attitudes about marijuana show a clear shift in favor of legalization (Caulkins et al. 2015).
As we will argue throughout this article, however, at least three reasons suggest that we use caution in drawing conclusions from the mixed empirical evidence or, more importantly, in assuming that a change to legally protected commercial markets would result in outcomes similar to those of the previous experiments. First, the literature has largely treated both decriminalization and medical marijuana policies as if they were simple dichotomous choices, implemented similarly across states. Such a treatment ignores the significant heterogeneity in these policies that can differentially influence harms and benefits and also contributes to what appear to be mixed results from evaluations. Second, the vast majority of policy evaluations conducted thus far examine the effect of the policy in terms of changes in prevalence rates in the general population, which assumes that the proportion of casual and heavy users, who are pooled together in these simple prevalence rates, remains stable even as the policy changes. Finally, research has been slow to consider the extent to which these changes in policies influence the method by which the typical user consumes marijuana. The potential acute harm associated with smoking a joint is different from that associated with consuming an edible or dabbing wax, particularly given that the average potency of the product typically differs and the body’s rate of absorption of THC varies by method (Huestis 2007).
In this article, we review the existing literature on the effects of decriminalization and medical marijuana laws on marijuana use and marijuana use disorders in light of these limitations. Unlike other reviews, our goal is not to summarize all the existing literature on the effects of decriminalization and medicalization. Rather, the purpose of this review is to provide a better understanding of what can be gleaned from the literature when more consideration is given to the complexities of these policies, the populations examined, and the measures of use considered. Doing so allows us to convey the need for more research, in terms of measurement and analysis, before we can truly understand the impacts of marijuana liberalization policies.
WHAT IS MEANT BY HETEROGENEOUS MARIJUANA POLICIES
Defining the Policies
It is important for any discussion of the literature to begin by defining the policies being considered. For the purposes of this review, we define four specific marijuana policies (prohibition, decriminalization, medical marijuana, and legalization) in terms of their legal definitions rather than their implementation in local communities, as the latter is often a function of the level of enforcement, which is difficult to measure in a systematic and analytic way. Prohibition, therefore, can be defined as a law that maintains the criminal status of any action related to marijuana possession, use, cultivation, sale, or distribution. The level of crime may be statutorily defined as either a misdemeanor (incurring relatively lower criminal penalties that may or may not include jail time) or a felony (entailing much more serious charges, tougher sanctions, and certain prison time), and the charge may be a function of the amount of marijuana involved or simply of the nature of the activity (e.g., sale to minors). Regardless, the emphasis is on the criminal status of the related offenses, not the degree to which local law enforcement chooses to enforce it. The US federal government, for example, retains its prohibition on all marijuana activities (possession, use, cultivation, distribution, processing, and sale) as do cities like San Francisco, although San Francisco has adopted a policy of low-priority enforcement (Ross & Walker 2017).
Decriminalization is a policy that was first defined by the 1972 Shaffer Commission (also known as the National Commission on Marihuana and Drug Abuse), and it describes policies that do not define possession for personal use or casual (nonmonetary) distribution as a criminal offense. The Shaffer Commission clearly stated that policies that simply lowered the penalties without removing the criminal status of the offense were not technically decriminalized, because they maintained the substantial social harm of the associated criminal convictions (Natl. Comm. Marihuana Drug Abus. 1972). This distinction between policies that simply lower penalties and those that actually change the legal status of the offense is important, and yet it is not widely understood by many researchers evaluating even the early policies. At least 2 of the 11 widely recognized decriminalized states from the 1970s and 1980s, California and North Carolina, did not remove the criminal status of the offense (Pacula et al. 2003, Reuter & MacCoun 1995). Instead, these states merely reduced the penalties associated with possession and/or use of marijuana, a policy generally known as depenalization (MacCoun & Reuter 2001, Pacula et al. 2005). Yet, individuals in depenalization jurisdictions can still face significant barriers to access work, student loans, and public assistance if caught in possession of marijuana, even if they are only charged with a small fine, because they can still get a criminal charge on their record.
Medical marijuana laws (MMLs) remove state penalties for the use of marijuana for medicinal purposes under specified conditions. Although the federal government continues to retain the 1970 classification of marijuana as a Schedule I substance with high potential for abuse and no accepted medical value (Title II of the Comprehensive Drug Abuse Prevention and Control Act of 1970, P.L. 91–513, October 27, 1970, 84 Stat. 1242, 21 U.S.C. 801, et seq.), states have employed a number of regulatory approaches aimed at increasing access to marijuana for medicinal purposes since the 1970s. Early initiatives through the 1980s aimed to encourage study of the therapeutic value of marijuana, but they had little practical significance due to their heavy reliance on federal cooperation and the failure to establish a legitimate supply channel for patients (Pacula et al. 2002). Initiatives passed since the 1990s have been far more comprehensive, establishing allowances for the use, possession, and supply of high (>3%) Δ9-tetrahydrocannabinol (THC) products for qualifying patients and their caregivers or providers. These modern MMLs have become the most commonly evaluated policies in comparative alcohol and drugs policy analysis (Ritter et al. 2016), but incomplete consideration of widespread variation in how these laws have been designed and implemented has resulted in inconclusive and often contradictory findings (Hunt & Miles 2015; Pacula et al. 2014a, 2015).
Legalization removes criminal and monetary penalties for the possession, use, and supply of marijuana for recreational purposes. Whereas decriminalized countries such as the Netherlands have histories of de facto legalization, and medical marijuana programs are often regarded as thinly veiled recreational legalization (Fischer et al. 2015, Haney & Evins 2016), de jure legalization is a relatively new phenomenon. The November 2012 ballot initiatives passed by voters in Colorado and Washington marked the first time that any jurisdiction worldwide has legally regulated marijuana. Much attention has been given to the recently created retail markets for legal marijuana in these two states, but the commercial model is but one regulatory option for legal production, and a number of alternative strategies are available (Caulkins et al. 2015). Research has not yet assessed the consequences of legalization, but the effects on the prevalence of marijuana use and use disorders will depend largely on the specific state-level regulations adopted as well as the response of the federal government.
Establishing clear definitions for decriminalized, medicalized, and legalized states is not merely a semantic exercise; rather, it highlights the different mechanisms through which policies may influence use, including changes in perceptions of risk or social disapproval, changes in product availability and variety, and changes in production methods or costs that reduce prices. Although it is tempting to use evaluations of decriminalization and medical marijuana policies to shed light on the likely consequences of legalization, the experiences of these states may not fully reflect the changes in price, potency, and product variety that will likely result from increased commercialization and promotion under legalization (Caulkins et al. 2012). Additionally, prior research on decriminalization and MMLs has suffered from serious limitations due to an overreliance on crude indicators that do not account for the complex and varied ways in which states have designed and implemented their policies (Pacula & Sevigny 2014a,b; Pacula et al. 2005). Although the existing literature may be limited in answering how legalization will affect marijuana use and associated outcomes, it offers significant insights into how we should evaluate the effects of marijuana policy changes in a rapidly evolving and multilayered policy environment.
Decriminalization and Definitional Problems
As stated previously, much of the scientific research evaluating the impacts of decriminalization in the United States has ignored the legal definition provided by the Shaffer Commission. In an examination of the original 11 statutes passed shortly after the Shaffer Commission, Pacula and colleagues (2003) discovered that 2 of the 11 widely recognized decriminalized states (California and North Carolina) retained the criminal status of marijuana possession offenses. Moreover, the reduced penalties in 4 of the original 11 states (Minnesota, Mississippi, Nebraska, and North Carolina) only applied to first-time offenders, a distinction not consistent with the spirit of the Shaffer Commission definition. A comparison of state statutory penalties in so-called nondecriminalized states and in decriminalized states reveals that it is not possible to uniquely distinguish the two groups (Pacula et al. 2003, 2005). As early as 2001, there were 7 so-called nondecriminalized states that had removed the criminal status of all marijuana possession offenses and another 13 states that allowed for the reduced penalties and expungement of the criminal offense for first-time offenders (Pacula et al. 2005). Yet, research continued to use the decriminalization variable to identify differences in state marijuana policies that were not truly based on the criminal status or level of penalties.
Given that most US studies have made use of a single dichotomous measure that cannot uniquely differentiate states with lower penalties and reduced criminal status, it is not surprising that they had mixed results. Even early studies examining immediate changes in laws using data from the 1970s and 1980s did not generate consistent findings. Although several studies making use of population survey data found no statistically significant impact of decriminalization on general prevalence rates of marijuana use (Johnston et al. 1981, Maloff 1981, Single 1989), one study looking at emergency room episodes found that cities in states that had decriminalized had higher marijuana-involved episodes than cities in nondecriminalized states (Model 1993). More recent studies that analytically relied on cross-sectional variation in decriminalization status in the late 1980s and 1990s also produced mixed findings. For example, studies examining self-reported use among youth and young adults that only included the single dichotomous measure for marijuana decriminalization found no statistical association with measures of past-year or past-month use (DiNardo & Lemieux 2001, Pacula 1998, Thies & Register 1993). Yet analyses of the adult household population (Saffer & Chaloupka 1999) and studies examining youth but incorporating other measures of legal risk (DeSimone & Farrelly 2003, Pacula et al. 2003) did find evidence of a positive association between decriminalization status and prevalence of use. MacCoun et al. (2009) note that the fact that the state decriminalization indicator remains positive and significant in analyses that also include additional controls for the statutory penalties for these offenses suggests that this measure is picking up something other than a signal related to a reduction in the legal risk. Hypotheses offered include a proxy of broader social acceptance of marijuana use and an advertising effect of the reduced policies.
Even beyond the problem of policy measurement, results from US studies evaluating the impact of marijuana decriminalization need to be interpreted with caution for several reasons. First, in many studies, marijuana possession penalties do not vary substantially over time, which analytically confounds the effects of unobserved state characteristics (e.g., tough-on-crime lawmakers) with differences observed in the level of penalties. Second, because there is no comprehensive data source reporting the actual penalties incurred by offenders, these studies have all relied on proxies, such as maximum or median fines as indicated by statutory laws. These statutory penalties may or may not accurately reflect the true severity of the penalties imposed in a jurisdiction. Last, evidence has shown that citizens have relatively limited knowledge as to the statutory penalties and policies for marijuana possession in their states (MacCoun et al. 2009), which makes it difficult to interpret evidence showing that removal of such penalties has a significant causal effect on marijuana consumption.
Medical Marijuana Laws in a Complex and Dynamic Policy Environment
In 1996, California became the first state to pass what is now commonly recognized as an MML. As of January 2016, 25 additional states have passed similar legislation. Empirical evidence consistently shows a strong correlation between MMLs and the prevalence of marijuana use and marijuana use disorders (Cerdá et al. 2012, Wall et al. 2011), but studies have not consistently supported a causal interpretation (Anderson et al. 2015, Hasin et al. 2015b, Lynne-Landsman et al. 2013, Wen et al. 2015).
One explanation for the inconsistent findings from causal studies is that the specific provisions of state MMLs have varied widely both among states and within any given state over time (Pacula et al. 2014a,b). The use of a single dichotomous indicator for the initial passage of an MML in policy evaluation obscures both types of variation. Because the effects of any policy will depend on the specific statutory provisions and their implementation, studies examining outcome data covering different time frames are in fact evaluating the effects of very different policies. Further confounding comparison of prior estimates is the fact that the federal enforcement position has changed over time, and state MML provisions have adapted alongside changes in the federal stance.
When one takes a historical look at how MMLs have evolved since the passage of California’s law in 1996, it becomes easy to understand how a single dichotomous measure falls short of describing these policies within a state and across states over time. We broadly categorize state policies into three waves, each initiated by an important political change: the ballot era (1996–2000), the early legislative era (2000–2009), and the late legislative era (2009–present).
The ballot era states are the first seven states that enacted policies through ballot initiatives (whether subsequently contested by state courts or not). These early laws aimed to protect the rights of patients who used medical marijuana and their caregivers who assisted in that use. Federal opposition to these policies was explicit, and one month after Proposition 215 passed in California, then-drug czar Barry McCaffrey threatened to arrest any physician who recommended cannabis to a patient (Pertwee 2014). The threat of federal enforcement created an important barrier to establishing clearly defined legal access to medical marijuana. Early MMLs during the ballot era were often vague, defining medical use broadly to include consumption, home cultivation, production, transportation, and acquisition. Most of the laws were ambiguous as to the legality of group growing or storefront dispensaries, resulting in confusion among law enforcement, patients, and caregivers as to what constituted legal participation in the medical marijuana market. Furthermore, the uncertainty of the federal response to these state experiments meant that ballot era policies rarely mandated patients to register with a state authority, making it even more difficult for law enforcement to differentiate legitimate medical users from recreational users. It is thus unsurprising that research examining the effects of the early state ballot laws on marijuana use has found insignificant effects (Gorman & Huber 2007, Khatapoush & Hallfors 2004).
With the passage of S.B. 862 in 2000, Hawaii became the first state to pass an MML through the state legislature rather than by ballot initiative. Learning from the frustrating experiences of patients and law enforcement under the earlier state policies, states that passed laws during this early legislative era (2000–2009) made more explicit allowances regarding the supply chain. Most laws passed during this period included patient registry provisions, allowances for home cultivation, and limits on the amount of marijuana that patients or caregivers could possess and grow. In addition, many states that had initially passed laws through ballot initiatives (e.g., California and Oregon) made further policy changes through their state legislatures during this period in an attempt to clarify issues and address tensions that had emerged.
Although MMLs during this early legislative era established clearer definitions of what constituted legal supply, uncertainty about the federal response to these policies inhibited a formal state regulation of producers. For instance, Colorado’s 2001 law did not explicitly sanction cooperative growing, but the ambiguity of the law allowed for its de facto operation. Through S.B. 420, California amended its initial MML to explicitly allow for cooperative cultivation, but regulatory discretion was left to local governments. New Mexico was the only state in the early legislative era to establish legal provisions for state-licensed dispensaries in its initial legislation in July 2007, but threats of federal prosecution led to indefinite delays in licensing (Baker 2007).
Protracted legal disputes about the legitimacy of retail outlets under state law combined with tremendous uncertainty about the federal response led to the slow development of medical marijuana markets throughout many states during the early legislative era, which helps explain why many studies evaluating MMLs from this period find insignificant effects on prevalence of marijuana use (Anderson et al. 2012, 2015; Harper et al. 2012; Lynne-Landsman et al. 2013; Pacula et al. 2015). Whereas norms may have been changing in response to these laws, direct access through markets was not necessarily increasing (Smart 2016). Yet, two studies making use of data from only this time period find a significant positive effect of MML enactment on use among specific high-risk populations (Chu 2014, Pacula et al. 2010). Making use of quarterly data from the 2000–2003 Arrestee Drug Abuse Monitoring (ADAM), Pacula et al. (2010) find a positive association between MML and self-reported marijuana use (confirmed through urine samples) among adult male arrestees. Chu (2014) similarly found significant positive effects of MML policies on marijuana possession arrests and marijuana-related treatment admissions, though the results are sensitive to model specification. These studies may indicate that increased medical marijuana supply in an uncertain policy environment primarily affected marijuana consumption among an at-risk population of heavy users. However, the results are also consistent with endogenous responses by police enforcement or treatment facilities and may not reflect actual changes in use.
In 2009, the uncertainty about the federal government’s response was seemingly resolved. Shortly following the inauguration of President Barack Obama, Attorney General Eric Holder issued a statement that federal authorities would cease interfering with medical marijuana dispensaries operating in compliance with state law (Johnston & Lewis 2009). On October 19, 2009, Deputy Attorney General David Ogden formalized this policy of federal nonenforcement with a memorandum stating that federal prosecutors “should not focus federal resources … on individuals who are in clear and unambiguous compliance with existing state laws providing for the medical use of marijuana” (Ogden 2009, pp. 1–2).
The clarification of the federal position dramatically changed the regulatory structure of state medical marijuana supply channels. State MMLs passed during the late legislative era (2009–present) established far more comprehensive and explicit regulations regarding medical marijuana distribution, often requiring elaborate systems that would take years to fully implement. Several early-enacting states (e.g., Oregon and Maine) amended their laws to formally allow and regulate state-licensed dispensaries. State regulatory authorities became more prominently involved in the production and distribution of marijuana by overseeing the dispensing, manufacturing, and labeling of cannabis-derived products.
Following the Ogden Memo, requirements for the registration of patients and caregivers became far more standard in state policies, and the participation of both increased dramatically in state medical marijuana programs (Fairman 2015, Sevigny 2014). States that had delayed the implementation of formal supply channels (e.g., New Mexico) moved quickly to license dispensaries, and other states began to resolve legislative disputes about what constituted legally protected sources of supply. Alongside this expansion of medical marijuana markets during this period, media attention toward the issue of legal marijuana also increased markedly (Schuermeyer et al. 2014, Stringer & Maggard 2016).
Compared to earlier time periods, in the late legislative era marijuana use might respond more significantly to changes in policy as the availability and potency of the drug evolved with the changing structure and size of medical marijuana markets (Sevigny et al. 2014). Indeed, the one study to evaluate the effects of MML passage using only policies enacted in the early and late legislative eras (Wen et al. 2015) found a significant positive effect of MML enactment on the probability of recent marijuana use (14%), daily marijuana use (15%), and marijuana use disorders (10%). More studies focused on these later laws are needed to assess if these findings are robust.
Perhaps because of the federal permission for states to regulate medical marijuana more directly, medical marijuana policies adopted by states for the first time during this postlegislative era (e.g., by New York, Massachusetts, Illinois) contain a variety of features that differ considerably from those of the laws of early adopting states. For example, all MMLs passed after 2009 have established a state-licensed dispensary system and do not allow personal cultivation by patients or their caregivers, except under narrowly defined circumstances. Moreover, since 2010, states have adopted medical marijuana policies that are more consistent with traditional medical care and pharmaceutical regulation (Williams et al. 2016). For example, all require testing and labeling of marijuana cannabinoid profiles in addition to a bona-fide clinical doctor-patient relationship requiring the ongoing management of the condition.
Evidence that MML statutes are continuing to move in a more medicalized direction is evident by the growing number of high CBD-only laws since 2014. CBD is a naturally occurring nonpsychoactive compound in cannabis that has been demonstrated in a variety of clinical studies not only to have therapeutic effects but also to counter the intoxicating effects of THC (Koppel et al. 2014, Russo et al. 2007, Whiting et al. 2015). These new laws allow qualifying patients to use CBD extract, mostly in oil form, with minimal THC content, and its use is generally only allowed for a narrow range of medical conditions. Sixteen states have passed CBD laws since 2014, but these policies have been largely ignored by advocacy groups, and no research is studying their impacts (NCSL 2016b). With some exceptions, there is still limited regulation on potency (THC concentration) and other cannabinoids, medical product testing, and methods of consumption.
Considering Heterogeneous Implementation of Legalization
As of July 2016, five states have policies legalizing the possession of specified quantities of marijuana by adults aged 21 and older for recreational purposes.2 Voters in Colorado and Washington approved legalization initiatives in November 2012, and additional policies were passed in Alaska, Oregon, and the District of Columbia in November 2014. The current regulatory environment is complex and dynamic, as state and local governments are continually adapting legislation to evolve along with the industry (Subritzky et al. 2016). The effects of these policies on marijuana use and use disorders will be determined by how the design and implementation of the legal regulatory framework influence market structure, price and availability, and perceptions of risk and social approval. As research moves forward in evaluating the effects of recreational legalization, consideration needs to be given to differences and similarities in the regulatory frameworks established by each state.
The District of Columbia is the only legalized jurisdiction in the United States that does not allow the sale of marijuana for recreational use. Under DC’s law, adults can legally grow up to six plants (of which no more than three can be mature) in their primary residence and transfer up to 1 ounce of marijuana to another adult aged 21 and older if there is no remuneration. Sale of any amount of marijuana remains a criminal offense, punishable by up to six months in jail and a fine of $1,000 (Marijuana Work. Group 2016). In contrast, policies in Colorado, Washington, Oregon, and Alaska establish commercialized models of marijuana regulation. Retail sales in Colorado and Washington began respectively in January and July 2014, and Oregon began allowing sales for recreational use from medical marijuana dispensaries in October 2015. Alaska began licensing retail and product manufacturers in September 2016 (Hall & Lynskey 2016). Relative to the home cultivation model of the District of Columbia, commercialization is expected to substantially reduce production costs and generate incentives for legal suppliers to promote heavy consumption (Caulkins & Kilmer 2016).
However, the commercial model of legalization also offers increased scope for regulation, and each state has crafted its own collection of regulatory guidelines and legal provisions that could have important implications for the markets that develop within them. For example, whereas all states require separate licenses for cultivators, manufacturers or processors, and retailers, as well as licensing or certification for testing facilities, Washington alone has adopted regulations restricting the number of licenses a single firm can own. Moreover, Washington prohibits license holders from being involved in both production and retail, in an effort to forbid vertical integration and the efficiencies in production and distribution that can come with it. Washington has further limited the number of retail store licenses available to avoid issues related to overproduction; the other states have not. However, all states except Alaska restrict the size of cultivation facilities, and Washington has an additional cap on total statewide production. In addition to this policy heterogeneity at the state level, local municipalities have some discretion in determining the number of establishments permitted, the strictness of zoning requirements, and the time and manner in which businesses are allowed to operate. These differences in the structure of the market should theoretically influence the availability and cost of marijuana in each state, for reasons described in greater detail below.
Other important legal differences exist across states in terms of the allowance for a nonretail market. Washington is the only state that requires all marijuana for recreational use to be purchased through state-licensed retailers; no home cultivation is allowed. The other three states permit home cultivation by adults subject to specified plant limits (as in the District of Columbia). There are also different approaches to taxation. Currently, the three states with operating retail markets (Colorado, Washington, and Oregon) have instituted ad valorem taxes specific to marijuana, ranging from 17% in Oregon to 37% in Washington. In contrast, Alaska’s policy establishes a tax on cultivation, imposing a $50 per ounce tax on marijuana bud (i.e., flowers) and a $15 per ounce tax on other parts of the plant (stems and leaves).
Differences in how state and local governments regulate the commercial market will generate heterogeneous effects on the retail price of marijuana, which will have important consequences for both the extensive and intensive margins of use and abuse (Pacula & Lundberg 2014, Pacula et al. 2014b). Moreover, because marijuana is involved in a variety of forms and potencies, choices about the tax level, base, and point of collection can also influence the products and potencies available to consumers and the prices they face (Caulkins et al. 2015). Currently, retail stores are allowed to offer marijuana flowers, concentrates, and infused products in solid and liquid form. The original legalization measures in Colorado and Washington did not explicitly distinguish between product types when establishing consumer purchase limits. As marijuana concentrates and infused products have captured an increasing share of legal retail sales, regulations have had to expand. Effective October 2016, adult residents in Colorado are limited to purchasing 1 ounce of marijuana flower, 8 g of concentrates, or 80 10-mg servings of THC in infused product form. In Washington and Alaska, consumers can purchase 1 ounce of marijuana flower, 7 g of marijuana concentrates, 16 ounces of infused product in solid form, or 72 ounces in beverage form. Oregon’s regulations are similar, except for a stricter limit of 5 g for marijuana concentrates. Alaska’s rules also limit buyers to 5,600 mg of THC in a single purchase.
Due to concerns regarding accidental ingestion of edibles by children, states have further regulated marijuana-infused products by implementing stricter packaging and labeling requirements and designating potency limits for individual serving sizes. Washington and Colorado designate individual serving sizes of 10 mg of THC and 100 mg total for an individually wrapped package. In Colorado, products that cannot be stamped, such as drinks or granola, must contain no more than a designated individual serving, effectively banning many of the high-potency marijuana-infused beverages currently sold. Oregon and Alaska have more conservative requirements, designating individual serving sizes of 5 mg of THC and 50 mg total for an individually wrapped package. Still, no state has capped the potency of marijuana products. A measure to limit the THC content of all marijuana products sold at retail stores in Colorado to 16% (Initiative 139) was withdrawn by the Healthy Colorado Coalition in 2016 due to the emergence of a well-funded opposition campaign (Armbrister 2016). In Alaska, a proposal to cap marijuana product potency at 76% THC was also voted down. The lack of restrictions on potency enables the marketing of products with very high (and often uncertain) levels of THC.
Increased marketing has been an important concern under the commercial model, because advertising can be used to promote harmful use and has been shown to influence adolescent marijuana use and intention to use (D’Amico et al. 2015). Colorado’s regulations prohibit Internet pop-up advertisements and advertisements that target children. Washington allows retailers to have only two signs (not to exceed 1,600 square inches) at their place of business, but the signs cannot contain marijuana-themed imagery nor can marijuana-related imagery be featured in window displays. Alaska and Oregon continue to revise rules for marijuana marketing. The strictness of state regulations for advertising and the way they are enforced can partly mediate the extent to which legalization influences perceptions and consumption behaviors among legal consumers as well as adolescents. However, these potential benefits of advertising restrictions must be balanced against potential efficiency costs resulting from information asymmetries between suppliers and consumers.
As was the case with decriminalization and MMLs, legalization is not a binary policy variable. The home cultivation model of the District of Columbia will have very different implications for supply than the commercialized models of Colorado, Washington, Oregon, and Alaska. Within commercialized states, heterogeneity in how production and price are regulated will lead to different consequences for consumption by legal adult users and spillovers to adolescent markets. Restrictions placed on advertising could limit youth exposure to messaging that could encourage experimentation, but only if the regulations are enforced. The way in which product availability and potency are regulated will have important effects on the total quantity of marijuana consumed by users and their level of intoxication, which will in turn influence the prevalence of marijuana use disorders. Legalized states have chosen different ways of regulating, and this policy heterogeneity will need to be considered in future work when assessing the effects of legalization on use.
WHAT IS MEANT BY HETEROGENEOUS POPULATIONS
The previous section focused on the heterogeneity of the policies being implemented. However, the effects of these diverse policies may well vary depending on the population group studied. Heterogeneous effects across population subgroups may be driven by differences in budget constraints (Markowitz & Taurus 2009), price elasticities (Pacula & Lundberg 2014), preferences for risk (Fox & Tannenbaum 2011), or search costs (Galenianos et al. 2012, Pacula et al. 2010), to name a few. Mixed findings in the current literature with respect to the impact of prior liberalization policies may thus reflect legitimate differences in the populations being studied.
Past research has generally attempted to accommodate this potential heterogeneity by stratifying analyses by age (e.g., adolescents, young adults, older adults) and, to a lesser extent, frequency of use (number of times used in the past month/year or near-daily use). The potential effects on youth consumption have been of particular concern in the literature, because evidence suggests that use of marijuana during early adolescence predicts increased risk of dependence, lower educational attainment, and cognitive impairment (Hall 2009, 2015). Limiting the analysis to adolescents, research shows that MML enactment has largely insignificant or even negative effects on youth marijuana use measures (Anderson et al. 2015, Choo et al. 2014, Gorman & Huber 2007, Harper et al. 2012, Hasin et al. 2015b, Lynne-Landsman et al. 2013), with only Wen et al. (2015) finding a significant increase in the probability of past-year initiation among youths aged 12–20. The results of the few studies that have focused on changes in marijuana consumption among adults have been more mixed, with some showing no effect of MML passage on measures of use (Gorman & Huber 2007, Harper et al. 2012) and others finding significant positive effects (Chu 2014, Wen et al. 2015).
Yet, as noted above, the use of a dichotomous MML variable misses important variations in the specific implementation of supply channels, which may be particularly important in determining the extent to which medical marijuana is diverted to adolescent markets (Boyd et al. 2015, Nussbaum et al. 2015, Salomonsen-Sautel et al. 2012). When studies focus on the effects of dispensary legalization, there is some evidence of a significant increase in youth consumption (Pacula et al. 2015, Wen et al. 2015), though other studies find no effect (Hasin et al. 2015b). Even within the same study, estimated effects switch sign depending on whether consumption is measured by past-month use, frequency of use, or dependence (Pacula et al. 2015, Wen et al. 2015). Similar inconsistencies exist in studies of the effects of specific dimensions of MML policy on measures of marijuana use in the general population (Anderson & Rees 2014, Choi 2014, Pacula et al. 2015). Thus, age alone is clearly not an adequate way of capturing population heterogeneity.
Perhaps a more relevant dimension of population heterogeneity pertains to differentiating casual or light users from high-risk consumers, often identified in this literature as arrestees (Chu 2014, Pacula et al. 2010), polysubstance users (Wen et al. 2015, Williams & Mahmoudi 2004), or those admitted to treatment (Pacula et al. 2015). Only a few studies have focused on high-risk users, but those that have tend to find more consistent evidence that marijuana liberalization significantly increases use (Chu 2014; Model 1993; Pacula et al. 2010, 2015; Wen et al. 2015). The response of high-risk users to marijuana policy changes will likely differ from that of casual users or nonusers due to differences in price sensitivity (Pacula & Lundberg 2014, Sumnall et al. 2004), knowledge of the policy environment (MacCoun et al. 2009), engagement with drug markets (Pacula et al. 2010), and perceived social or physical harms from use (Haardörfer et al. 2016, Kilmer et al. 2007). By examining how marijuana liberalization policy affects the prevalence of marijuana use, many past evaluations have conflated changes in the consumption of casual users with changes in the consumption of regular or heavy users. Because casual users represent a larger proportion of the total number of users, such analyses will discount the behaviors of heavy users, who account for a larger proportion of the total quantity of marijuana consumed (Burns et al. 2013, Davenport & Caulkins 2016).
The overreliance on using prevalence measures as the outcome of interest in past work is largely a consequence of limited data availability, but as legal markets for marijuana develop, there is an urgent need to assess the alternative measures of use that are more relevant for understanding potential harms. Nationally representative data show that the number of daily or near-daily (DND) users has increased approximately sevenfold since 1992 (Burns et al. 2013), and the prevalence of marijuana use disorders has almost doubled since 2001 (Hasin et al. 2015a). Simultaneous use of marijuana with other substances (e.g., tobacco and alcohol) is common and has been shown to be associated with increased risk of adverse consequences (Subbaraman & Kerr 2015, Terry-McElrath et al. 2014). Currently, we have little evidence to indicate how marijuana liberalization policies will affect these outcomes (Wen et al. 2015). Moving forward, it will be important to develop more comprehensive data collection and sampling designs to assess how marijuana liberalization policies affect populations at risk for problematic use as well as the use of particularly dangerous products or methods of consumption.
WHAT IS MEANT BY HETEROGENEOUS PRODUCTS
Past research has generally focused on how liberalization affects the prevalence of marijuana use and has paid less attention to how liberalization affects the type of marijuana used or the way in which it is consumed. But marijuana is not a uniform product. The cannabis plant itself can develop in a number of different ways, depending on the genetic variety, temperature, culture condition, and lighting it receives. The potency of the consumable product, typically measured by concentration or level of THC, will vary by strain, cultivation technique, and method of processing. There are also a variety of ways to consume marijuana, with the most common methods including smoking, vaporization, and ingestion of edible products (Schauer et al. 2016).
Both potency and methods of consumption have evolved over time. Decriminalization occurred during a time when marijuana was largely smoked, which facilitated comparisons of marijuana use rates between decriminalized and nondecriminalized states. Medical marijuana brought with it new products (e.g., oils and edibles), new methods for consuming it (e.g., dabbing, vaping), and new techniques for controlling potency (Pacula et al. 2016, Rendon 2013). Legalization only extends these new products to even more users. It is difficult to predict the extent to which legalization will increase product innovation, as growth in the industry will promote the development of new methods for extracting and synthesizing the hundreds of chemicals in the cannabis plant, of which relatively little is known (Caulkins et al. 2015).
Systematic data collection on methods of use and potency is limited, but available evidence indicates that marijuana users in states with medical or recreational legalization consume a different product mix than users in other states. Individuals living in MML states, particularly in states with greater access to dispensaries, have significantly higher likelihood of vaporizing or ingesting marijuana products compared to individuals in states without MMLs (Borodovsky et al. 2016). Evidence also suggests that states that legally permit medical marijuana dispensaries experience significant increases in average marijuana potency (Sevigny et al. 2014). Within states with legalized dispensaries, adults who use marijuana for medicinal purposes are significantly more likely to vaporize it or consume edibles than individuals who use it for recreational purposes (Pacula et al. 2016).
It is complicated to assess the impact of policy on use if the product being consumed or the method of consumption changes in line with the policy. Outcomes such as level of intoxication or dependency may well vary according to the type and method of marijuana consumption, and simply comparing use in legalized states to use in nonlegalized states will not reflect these differences. Changes in product variety will not threaten the identification of changes on the extensive margin of use (meaning any use or prevalence), because existing survey measures can provide information on the number of people who transition from nonusers to users and those who continue using rather than quitting. However, most of the adverse physical and behavioral consequences associated with marijuana use come from heavy users (Gordon et al. 2013, Hall 2015, Volkow et al. 2014). Proper evaluation of the public health consequences of legalization relies on the ability of research to estimate the effects of marijuana policy changes on the intensive margin of use.
Data on quantity of marijuana used are surprisingly limited, and researchers have yet to construct a standardized measure for the unit of marijuana consumption (as exists with alcohol). Prior research has examined changes on the intensive margin through self-reported data on frequency of use, measured by days of use in the past month or past year. The implicit assumption has been that more days of use accurately proxies for higher intensity of use (Temple et al. 2011). Yet, marijuana consumption among DND users can vary from smoking a single low-THC joint each day to using high-THC products multiple times per day via multiple delivery methods (Hughes et al. 2014, Zeisser et al. 2012). Given the variety of delivery devices, strains, and cannabinoid concentrations that become available as the legal industry expands, measuring changes in days of use will fail to capture a number of individuals who transition from occasional to heavy users.
Heterogeneity of marijuana products presents further problems for understanding how medical and recreational legalization affect marijuana use disorders. Previous research examining patterns of use and the development of dependence may not generalize to a legal environment in which there is greater social acceptance, fewer perceived risks and harms, and a wider variety of product types and potencies (Asbridge et al. 2014). Although the definition of marijuana use disorder is evolving (Compton & Baler 2016, Hasin et al. 2013), there has been little clinical assessment of whether the use of different marijuana products carries different risks of dependence or harms. Some evidence suggests that vaporizing hash oil or dabbing is more positively associated with tolerance and withdrawal among adults compared to smoking marijuana (Loflin & Earleywine 2014), but there may be differential effects for adolescents. As marijuana product diversity expands, there is a need for a more comprehensive understanding and analysis of consumption to accurately evaluate changes in use prevalence, intensity of use, and risk for marijuana use disorder.
AN ALTERNATIVE PERSPECTIVE FOR EVALUATING THE EFFECTS OF MEDICAL MARIJUANA LAWS AND LEGALIZATION
In light of the substantial variation underlying the policies being evaluated, the populations considered, and the products consumed, it is not surprising that the scientific literature evaluating the impact of these policies is inconclusive. The decisions made by researchers to focus on specific time periods, states, populations, and/or outcome measures have often been driven by what data were available and not by a careful consideration of the mechanisms by which these policies are expected to influence marijuana use or use disorders among various populations. As this article has established, these decisions can influence the likelihood of finding—or not finding—specific effects because of the heterogeneity of these policies and of the markets that are emerging in light of them.
The program evaluation literature has widely recognized the time it takes between the passing of new policies and their full implementation as a problematic issue (Hunt & Miles 2015, King & Behrman 2009). A common empirical strategy for accommodating delays in implementation is the inclusion of lagged policy variables, and this approach has been explored in a few articles from the medical marijuana literature (Anderson et al. 2013, Bachhuber et al. 2014, Chu 2014). However, assuming a constant allowance for lagged effects obscures the fact that these delays are not random but are correlated with the specific provisions established by state law, the broader federal policy environment, and the setting in which the policy change occurs.
The relationship between state policy heterogeneity and variation in how long it takes for markets to emerge is something that is just beginning to receive the attention it deserves in the literature (Collett et al. 2013, Smart 2016). As explained by Smart (2016), patient registration rates do a better job than simple dichotomous policy variables at capturing the extent to which medical marijuana markets are operating throughout a state. Smart notes that despite the adoption of early policies by many states, the relative size of the associated markets, as measured by registered patients, remained small in most states until federal enforcement policy was clarified in 2009, at which time markets in all states grew substantially faster. In an analysis that explicitly accounts for changes in the size of medical marijuana markets, Smart (2016) finds statistically more robust and consistent evidence of the impacts of these markets on various measures of consumption across users from all age groups.
The consideration of the relative size of these markets across states highlights the necessity to consider the issue of dynamics. Whereas some aspects of medical marijuana and legalization policies can have immediate impacts (e.g., on the criminalization of marijuana use or the ability to grow it at home), other effects of these policies take time to occur or disseminate. In the case of markets, for example, it takes time for regulations to develop regarding how many businesses are allowed, who is allowed to operate a business, and where those businesses are allowed to operate. It takes even longer once those rules are passed for businesses to obtain permits and begin distribution. Thus, it should not be surprising that after the passing of marijuana legalization measures in Colorado and Washington in November 2012, it took at least 18–20 months for retail stores to open. Data on the consequences of the opening of these stores beyond sales and tax revenues are just beginning to become available, which is why rigorous scientific evaluations of the impact of these policies have been slow to develop.
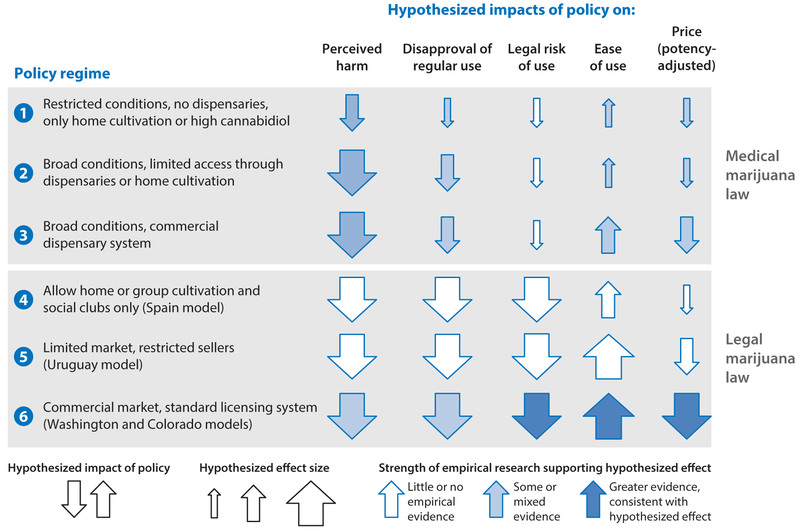
What that means is that researchers working in this space need to pay far greater attention to the specific mechanisms that different types of policies are likely to influence and to consider them within the proper timeframe when assessing impacts on specific populations. We show in Figure 2 some of the primary mechanisms discussed in the literature through which these changes in policies might impact use (i.e., perceived harm, disapproval of regular use, legal risk of use, ease of access and price) as well as the hypothesized effects of various types of policies on each. For simplicity, we consider each mechanism separately, though it is important to note that these are likely not independently determined (e.g., changes in legal risk may influence perceived harms, or changes in ease of access may influence disapproval). A small, medium, or large arrow (pointing up or down) in each cell indicates the relative magnitude and direction of the hypothesized effect. Shading represents the availability of empirical evidence to support the theoretical prediction, with white indicating an absence of existing studies and darker shades representing greater and more consistent support for the hypothesized effect. We provide three simplified versions of a medical marijuana policy and a legal recreational market to illustrate a wider range of policies that would to varying degrees influence the general size of the associated markets (in terms of both users and sellers).
Figure 2.
Mechanisms through which marijuana policies might affect marijuana use and use disorders. This simple illustration shows that even within a single policy area (e.g., medical marijuana), the different variations of the policy can differentially influence each of the mechanisms related to use. For example, we hypothesize that medical marijuana policies will ceteris paribus have a larger impact on people’s perceptions about the drug (perceived harm and disapproval of regular use) than they will have on the legal risk and ease of access to marijuana regardless of policy, assuming that only medical users are provided access and legal protections. Relatedly, because these markets serve a relatively smaller group of users, the overall impacts on price are presumed to be small, although they might increase with the third type of MML, which could allow for competitive forces among suppliers to start influencing price (Anderson et al. 2013, Humphreys 2016, Pacula et al. 2010) and potency (Sevigny et al. 2014) in these markets. The existing evidence generally suggests that the passage of any type of MML significantly lowers perceived harms among adults (Choi 2014, Khatapoush & Hallfors 2004) but not among adolescents (Choi 2014, Keyes et al. 2016). However, the expansion of commercial medical marijuana markets and increased exposure to medical marijuana after 2009 have been associated with significant reductions in adolescent perceptions of harm or disapproval associated with marijuana use (Miech et al. 2015, Schuermeyer et al. 2014, Sobesky & Gorgens 2016, Thurstone et al. 2011).
Of course, under a policy of legalization, the hypothesized effects on some of the mechanisms (perceptions and legal risk) are larger and more immediate. Preliminary evidence from Colorado and Washington shows that commercial legalization has significantly reduced perceived harms and disapproval of marijuana use (Kosterman et al. 2016, Sobesky & Gorgens 2016), and marijuana-related arrests have plummeted (Gettman 2015a,b). Access and prices, however, will likely still be differentially influenced by the regulations that shape the market structure and the level of competition in the market (Caulkins et al. 2015, Smart 2016). The overall impact on consumption, then, would depend on (a) the relative importance of perceptions and legal risk vis-à-vis access and price for the specific population being evaluated, and (b) whether one is evaluating an immediate (short-run) response to the policy or a long-run effect that is inclusive of market mechanisms.
Another important consideration for interpreting findings when evaluating legalization effects is the baseline policy in place prior to legalization. Because most careful evaluations are done based on marginal changes over time, the baseline policy in the states that subsequently legalize will determine the extent to which a particular mechanism is impacted by the change in formal policy. States like Washington and Colorado, for example, which moved to legalization from a medical marijuana policy that already provided broad access and loose regulation of dispensaries, will likely experience far less of an impact on perceptions and access than states starting from a more restrictive medical marijuana policy or no law at all. Generalization of findings from these two state experiences, therefore, would not necessarily apply to states that may be considering a move to legalization without first allowing medical marijuana markets.
Thus far we have discussed heterogeneous policies, populations, and products as limitations that complicate the evaluation of how marijuana liberalization policies affect marijuana use and marijuana use disorders. However, Figure 2 suggests that this rich variation also offers unique opportunities for future research. By carefully considering the specific aspects of legalization statutes in the context of existing state policies, researchers have increased the scope for determining the mechanisms that are most important for influencing marijuana use among different populations. As more comprehensive data on marijuana prices and products become available, future work can examine not only whether liberalization affects marijuana use, but also whether it affects who uses marijuana, what products are used, and how these products are consumed. The literature has shown that not all marijuana liberalization policies are created equal, but by exploiting this variation we will be able to better evaluate which policy designs will maximize the potential benefits of legalization while minimizing potential harms.
CONCLUSION
The variety of marijuana liberalization policies across the US states is often ignored or inadequately considered when assessing the impacts of further policy reform. Despite the widespread state experimentation with alternative marijuana policies since the 1970s, our knowledge of the impact of these liberalization policies on the consumption of marijuana, and its benefits and harms, is far less developed than one would expect. There are a number of reasons for this, including, particularly, lack of attention to the heterogeneity of existing policies, the specificity of the populations examined, and modes of consumption.
Although findings tend to be mixed when we look at the literature as a whole, some consistent themes seem to emerge when we consider the literature with an eye toward differences between policies and populations. For example, studies that are attentive to the development of medical marijuana markets (e.g., through measures of the presence of active dispensaries or the size of the market) seem to consistently show a positive correlation of liberalization policies with use among high-risk users (arrestees, people in need of treatment, and polysubstance users). Similarly, many studies have shown a positive association with adult use of marijuana, whereas most have found no association with youth prevalence or frequency of use in general school populations. The extent to which these findings can be drawn on to make inferences about the potential impact of legalization on these same populations is not clear. Just as it took time for researchers to pay more careful attention to the differential effects of policy elements over time (Hasin et al. 2015b, Pacula et al. 2015, Smart 2016, Wen et al. 2015), as well as possible heterogeneous responses by different types of users (Pacula et al. 2015, Wen et al. 2015), it will take time for research to emerge that fully reconsiders these associations in light of the full policy dynamics (i.e., changes in a policy within a single state over time and duration of exposure of a population to a given policy type). As more studies account for and consider these heterogeneous effects and dynamics, we may get better clarity regarding the margins on which particular types of policies do or do not influence behavior, and for whom.
Because legal markets will continue to evolve before these questions are fully answered, the real work that lies ahead relies on obtaining more accurate information on the amount and type of products that various people are consuming. Imagine trying to communicate to the public health field the health benefits or harms of alcohol consumption without being able to indicate specific levels or amounts that translate into impairment in well-understood dose-response relationships. Or imagine trying to assess the harmful effects of smoking without being able to differentiate an experimental or occasional smoker from someone who smokes a pack a day. Yet, that is exactly where the science is today in terms of our measurement of marijuana consumption. Precise data on things such as a standardized dose, regular versus experimental use, heavy use, episodic impairment, or even simultaneous use of marijuana and alcohol are not yet captured in most of the data tracking systems used to evaluate the impact of these policies, and they are desperately needed. If marijuana is anything like alcohol, little harm will come from casual, occasional use by mature adults, and indeed such use might generate considerable benefits. Moreover, it is also possible that marijuana, like alcohol, generates positive benefits for one population (mature adults) while also causing negative harms for another population (youth and young adults). Scientific research needs to be mindful of this heterogeneity.
SUMMARY POINTS.
State policies legalizing marijuana are part of the evolution of state liberalization policies that has taken place since the 1970s.
Existing studies evaluating the impacts of prior state experimentation have generated inconclusive findings, and only recently has research attempted to understand the reasons for these mixed results.
One should be cautious when interpreting the evidence from all studies pooled together, because studies are not equivalent in their attention to policy heterogeneity, policy dynamics, and population heterogeneity.
The literature has largely treated both decriminalization and medical marijuana policies as if they were simple dichotomous choices, when in fact there can be substantial variation in the implementation of these policies that influences how adults or youth respond.
Relatively few studies evaluating the impact of MMLs give adequate consideration to the fact that some aspects of liberalizations policies are realized immediately (e.g., ability to grow one’s own), whereas other aspects may take time to evolve (e.g., opening of a market) or change in response to future state and federal policies.
Studies that focus on how marijuana liberalization policies influence past-month or past-year prevalence conflate changes in consumption among light and casual users with changes in consumption among regular and heavy users.
Although relatively few in number, studies that focus on high-risk users (arrestees, poly-substance users, heavy users) tend to find more consistent evidence that medical marijuana policies increase use, suggesting that this segment of the population is particularly sensitive to policy changes.
FUTURE ISSUES.
As legal markets for marijuana develop, there is an urgent need to assess the consequences of liberalization on alternative measures of use that are relevant for understanding potential harms; this requires developing better measures of standardized dose, heavy use, episodic impairment, and simultaneous use.
Research needs to pay more attention to the influence of these policies on the types of products consumed, the amount of THC being consumed in different products, and product development.
Future work also needs to give stronger consideration of the baseline from which new state policies are being evaluated. For example, legalization is likely to generate smaller population changes in medical marijuana states that already have active dispensaries than in states with no prior medical marijuana stores.
Researchers need to pay far greater attention to the specific mechanisms different types of policies are likely to influence and to consider them within the proper timeframe when assessing impacts on specific populations because not all users will respond in the same ways.
ACKNOWLEDGMENTS
This article was supported by a grant from the National Institute on Drug Abuse to the RAND Corporation (R01DA032693). The article benefited from research assistance provided by Anne Boustead, Ervant Maksabedian, and Gabriel Weinberger. We should also give credit to several of our DPRC colleagues whom we have been fortunate enough to conduct research with and who have influenced our thinking on this literature, including Jonathan Caulkins, Beau Kilmer, Mark Kleiman, Mireille Jacobson, Priscillia Hunt, David Powell, Paul Heaton, Eric Sevigny, Peter Reuter, and Rob MacCoun. All errors in the article are our own.
DISCLOSURE STATEMENT
The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
Footnotes
For simplicity, this article refers to the District of Columbia (DC) as a state.
Uruguay also legalized recreational marijuana in 2013, and Canada’s prime minister is working on a formal proposal expected to be delivered to the Canadian Parliament in April 2017. We are focusing on the US experience here because no formal stores are open in either Uruguay or Canada at this time.
LITERATURE CITED
- Anderson DM, Hansen B, Rees DI. 2012. Medical marijuana laws and teen marijuana use. Disc. Pap. 6592, IZA, Bonn, Ger. [Google Scholar]
- Anderson DM, Hansen B, Rees DI. 2013. Medical marijuana laws, traffic fatalities, and alcohol consumption. J. Law Econ 56:333–69 [Google Scholar]
- Anderson DM, Hansen B, Rees DI. 2015. Medical marijuana laws and teen marijuana use. Am. Law Econ. Rev 17(2):495–528 [Google Scholar]
- Anderson DM, Rees DI. 2014. The role of dispensaries: The devil is in the details. J. Policy Anal. Manag 33(1):235–40 [PubMed] [Google Scholar]
- Armbrister M 2016. Colorado pot potency ballot initiative is withdrawn. Denver Bus. J, July 8 [Google Scholar]
- Asbridge M, Duff C, Marsh DC, Erickson PG. 2014. Problems with the identification of “problematic” cannabis use: examining the issues of frequency, quantity, and drug use environment. Eur. Addict. Res 20:254–67 [DOI] [PubMed] [Google Scholar]
- Bachhuber MA, Saloner B, Cunningham CO, Barry CL. 2014. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999–2010. JAMA Intern. Med 174(10):1668–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker D 2007. N.M.:Won’t oversee marijuana production. Assoc. Press, August 16 [Google Scholar]
- Borodovsky JT, Crosier BS, Lee DC, Sargent JD, Budney AJ. 2016. Smoking, vaping, eating: Is legalization impacting the way people use cannabis? Int. J. Drug Policy 36:141–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd CJ, Veliz PT, McCabe SE. 2015. Adolescents’ use of medical marijuana: a secondary analysis of Monitoring the Future data. J. Adolesc. Health 57(2):241–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns RM, Caulkins JP, Everingham SS, Kilmer B. 2013. Statistics on cannabis users skew perceptions of cannabis use. Front. Psychiatry 4(138):1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caulkins JP, Hawken A, Kilmer B, Kleiman M. 2012. Marijuana Legalization: What Everyone Needs to Know. New York: Oxford Univ. Press [Google Scholar]
- Caulkins JP, Kilmer B. 2016. Considering marijuana legalization carefully: insights for other jurisdictions from analysis for Vermont. Addiction 111(12):2082–89 [DOI] [PubMed] [Google Scholar]
- Caulkins JP, Kilmer B, Kleiman MAR, MacCoun RJ, Midgette G, et al. 2015. Considering Marijuana Legalization: Insights for Vermont and Other Jurisdictions. Santa Monica, CA: RAND Corp. [Google Scholar]
- Cerdà M, Wall M, Keyes KM, Galea S, Hasin DS. 2012. Medical marijuana laws in 50 states: investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug Alcohol Depend. 120:22–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi A 2014. The impact of medical marijuana laws on marijuana use and other risky health behaviors. Presented at ASHE Conf., 5th, Los Angeles [Google Scholar]
- Choo EK, Benz M, Zaller N, Warren O, Rising KL, McConnell KJ. 2014. The impact of state medical marijuana legislation on adolescent marijuana use. J. Adolesc. Health 55(2):160–66 [DOI] [PubMed] [Google Scholar]
- Chu YWL. 2014. The effects of medical marijuana laws on illegal marijuana use. J. Health Econ. 38:43–61 [DOI] [PubMed] [Google Scholar]
- Collett SC, Gariffo T, Hernandez-Morgan M. 2013. Evaluation of the Medical Marijuana Program in Washington, D.C. Los Angeles: UCLA [Google Scholar]
- Compton WM, Baler R. 2016. The epidemiology ofDSM-5 cannabis use disorders among U.S. adults: science to inform clinicians working in a shifting social landscape. Am. J. Psychiatry 173(6):551–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Miles JNV, Tucker JS. 2015. Gateway to curiosity: medical marijuana ads and intention and use during middle school. Psychol. Addict. Behav 29(3):613–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davenport SS, Caulkins JP. 2016. Evolution of the United States: marijuana market in the decade of liberalization before full legalization. J. Drug Issues 46(4):411–27 [Google Scholar]
- DeSimone J, Farrelly MC. 2003. Price and enforcement effects on cocaine and marijuana demand. Econ. Inquiry 41:98–115 [Google Scholar]
- Dinardo J, Lemieux T. 2001. Alcohol, marijuana, and American youth: the unintended consequences of government regulation. J. Health Econ 20(6):991–1010 [DOI] [PubMed] [Google Scholar]
- Fairman BJ. 2015. Trends in registered medical marijuana participation rates across 13 US states and District of Columbia. Drug Alcohol Depend. 159:72–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer B, Kuganesan S, Room R. 2015. Medical marijuana programs: implications for cannabis control policy—observations from Canada. Int. J. Drug Policy 26(1):15–19 [DOI] [PubMed] [Google Scholar]
- Fox CR, Tannenbaum D. 2011. The elusive search for stable risk preferences. Front. Psychol 2:298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galenianos M, Pacula RL, Persico N. 2012. A search-theoretic model of the retail market for illicit drugs. Rev. Econ. Studies 79:1239–69 [Google Scholar]
- Gettman J 2015a. Marijuana Arrests in Colorado After the Passage of Amendment 64. New York: Drug Policy Alliance [Google Scholar]
- Gettman J 2015b. Status Report: Marijuana Legalization in Washington After 1 Year of Retail Sales and 2.5 Years of Legal Possession. New York: Drug Policy Alliance [Google Scholar]
- Gordon AJ, Conley JW, Gordon JM. 2013. Medical consequences of marijuana use: a review of the current literature. Curr. Psychiatry Rep 15(12):419. [DOI] [PubMed] [Google Scholar]
- Gorman DM, Huber J. 2007. Do medical cannabis laws encourage cannabis use? Int. J. Drug Policy 18(3):160–67 [DOI] [PubMed] [Google Scholar]
- Haardörfer R, Berg CJ, Lewis M, Payne J, Pillai D, et al. 2016. Polytobacco, marijuana, and alcohol use patterns in college students: a latent class analysis. Addict. Behav 59:58–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W 2009. The adverse health effects of cannabis use: What are they, and what are their implications for policy? Int. J. Drug Policy 20(6):458–66 [DOI] [PubMed] [Google Scholar]
- Hall W 2015. What has research over the past two decades revealed about the adverse effects of cannabis use? Addiction 110(1):19–35 [DOI] [PubMed] [Google Scholar]
- Hall W, Lynskey M. 2016. Evaluating the public health impacts of legalizing recreational cannabis use in the United States. Addiction 111(10):1764–73 [DOI] [PubMed] [Google Scholar]
- Haney M, Evins AE. 2016. Does cannabis cause, exacerbate, or ameliorate psychiatric disorders? An oversimplified debate discussed. Neuropsychopharmacology 41(2):393–401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper S, Strumpf EC, Kaufman JS. 2012. Do medical marijuana laws increase marijuana use? Replication study and extension. Ann. Epidemiol 22(3):207–12 [DOI] [PubMed] [Google Scholar]
- Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, et al. 2013. DSM-5 criteria for substance use disorders: recommendations and rationale. Am. J. Psychiatry 170:834–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, et al. 2015a. Prevalence of marijuana use disorders in the United States between 2001–2002 and 2012–2013. JAMA Psychiatry 72(12):1235–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Wall M, Keyes KM, Cerdà M, Schulenberg J, et al. 2015bMedical marijuana laws and adolescent marijuana use in the USA from 1991–2014: results from annual, repeated cross-sectional surveys. Lancet Psychiatry 2(7):601–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill KP. 2015. Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. JAMA 313(24):2474–83 [DOI] [PubMed] [Google Scholar]
- Huestis MA. 2007. Human cannabinoid pharmacokinetics. Chem. Biodivers 4(8):1770–804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Fingar JR, Budney AJ, Naud S, Helzer JE. 2014. Marijuana use and intoxication among daily users: an intensive longitudinal study. Addict. Behav 39(10):1464–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys K 2016. So, something interesting happens to weed after it’s legal. The Washington Post Wonkblog, May 4. https://www.washingtonpost.com/news/wonk/wp/2016/05/04/the-priceof-legal-pot-is-collapsing/
- Hunt PE, Miles J. 2015. The impact of legalizing and regulating weed: issues with study design and emerging findings in the USA. Curr. Topics Behav. Neurosci 10.1007/7854_2015_423 [DOI] [PubMed] [Google Scholar]
- Johnston D, Lewis NA. 2009. Ending raids of dispensers of marijuana for patients. New York: Times, March 18, p. A20 [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG. 1981. Marijuana decriminalization: the impact on youth 1975–1980 Monitoring the Future Occas. Pap. 13, Inst. Soc. Res., Univ. Mich., Ann Arbor [Google Scholar]
- Keyes KM, Wall M, Cerdà M, Schulenberg J, O’Malley PM, et al. 2016. How does state marijuana policy affect US youth? Medical marijuana laws, marijuana use and perceived harmfulness: 1991–2014. Addiction 111:2187–95. 10.1111/add.13523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khatapoush S, Hallfors D. 2004. “Sending the wrong message”: Did medical marijuana legalization in California change attitudes about and use of marijuana? J. Drug Issues 34:741–70 [Google Scholar]
- Kilmer B, Caulkins JP, Pacula RL, MacCoun RJ, Reuter P. 2010. Altered State? Assessing How Marijuana Legalization in California Could Influence Marijuana Consumption and Public Budgets. Santa Monica, CA: RAND Corp. [Google Scholar]
- Kilmer JR, Hunt SB, Lee CM, Neighbors C. 2007. Marijuana use, risk perception, and consequences: Is perceived risk congruent with reality? Addict. Behav 32:3026–33 [DOI] [PubMed] [Google Scholar]
- King E, Behrman J. 2009. Timing and duration of exposure in evaluations of social programs. World Bank Econ. Rev 22:539–66 [Google Scholar]
- Koppel BS, Brust JC, Fife T, Bronstein J, Youssof S, et al. 2014. Systematic review: efficacy and safety of medical marijuana in selected neurologic disorders. Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology 82(17):1556–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosterman R, Bailey JA, Guttmannova K, Jones TM, Eisenberg N, et al. 2016. Marijuana legalization and parents’ attitudes, use, and parenting in Washington State. J. Adolesc. Health 59(4):450–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loflin M, Earleywine M. 2014. A new method of cannabis ingestion: the dangers of dabs? Addict. Behav 39(10):1430–33 [DOI] [PubMed] [Google Scholar]
- Lynne-Landsman SD, Livingston MD, Wagenaar AC. 2013. Effects of state medical marijuana laws on adolescent marijuana use. Am. J. Public Health 103(8):1500–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCoun R, Pacula RL, Chriqui JF, Harris K, Reuter P. 2009. Do citizens know whether their state has decriminalized marijuana? Assessing the perceptual component of deterrence theory. Rev. Law Econ. 5:347–71 [Google Scholar]
- MacCoun R, Reuter P. 2001. Evaluating alternative cannabis regimes. Br. J. Psychiatry 178:123–28 [DOI] [PubMed] [Google Scholar]
- Maloff D 1981. A review of the effects of the decriminalization of marijuana. Contemp. Drug Probl. 10:307–22 [Google Scholar]
- Marijuana Work. Group. 2016. Initiative 71: Marijuana Working Group Status Report. Washington, DC: Gov. D.C. [Google Scholar]
- Markowitz S, Tauras J. 2009. Substance use among adolescent students with consideration of budget constraints. Rev. Econ. Househ 7:423–46 [Google Scholar]
- Miech RA, Johnston L, O’Malley PM, Bachman JG, Schulenberg J, Patrick ME. 2015. Trends in use of marijuana and attitudes toward marijuana among youth before and after decriminalization: the case of California 2007–2013. Int. J. Drug Policy 26:336–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Model K 1993. The effect of marijuana decriminalization on hospital emergency room episodes: 1975–1978. J. Am. Stat. Assoc 88(423):737–47 [Google Scholar]
- Natl. Comm. Marihuana Drug Abus. 1972. Marihuana: a signal of misunderstanding First Rep. Natl. Comm. Marihuana Drug Abus, US Gov. Print. Off., Washington, DC [Google Scholar]
- NCSL (Natl. Conf. State Legis.). 2016a. Marijuana overview, Aug. 2. http://www.ncsl.org/research/civil-and-criminal-justice/marijuana-overview.aspx
- NCSL (Natl. Conf. State Legis.). 2016b. State medical marijuana laws, Jul. 20. http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx
- Nussbaum AM, Thurstone C, McGarry L, Walker B, Sabel AL. 2015. Use and diversion of medical marijuana among adults admitted to inpatient psychiatry. Am. J. Drug Alcohol Abus. 41(2):166–72 [DOI] [PubMed] [Google Scholar]
- Ogden DW.2009. Investigations and Prosecutions in States Authorizing the Medical Use of Marijuana: Memorandum for Selected United States Attorneys. Washington, DC: US Dep. Justice, Off. Deputy Atty. [Google Scholar]
- Pacula RL. 1998. Does increasing the beer tax reduce marijuana consumption? J. Health Econ 17(5):557–86 [DOI] [PubMed] [Google Scholar]
- Pacula RL, Boustead A, Hunt P. 2014aWords can be deceiving: a review of variation among legally effective medical marijuana laws in the United States. J. Drug Policy Anal 7(1):1–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, Chriqui JF, King J. 2003. Decriminalization in the United States: What does it mean? Work. Pap. 9690, NBER, Cambridge, MA [Google Scholar]
- Pacula RL, Chriqui JF, Reichmann DA, Terry-McElrath YM. 2002. State medical marijuana laws: understanding the laws and their limitations. J. Public Health Policy 23(4):413–39 [PubMed] [Google Scholar]
- Pacula RL, Heaton P, Powell D, Sevigny EL. 2015. Assessing the effects of medical marijuana laws on marijuana use: The devil is in the details. J. Policy Anal. Manag 34(1):7–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, Jacobson M, Maksabedian EJ. 2016. In the weeds: a baseline view of cannabis use among legalizing states and their neighbors. Addiction 111:973–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, Kilmer B, Grossman M, Chaloupka FJ. 2010. Risks and prices: the role of user sanctions in marijuana markets. B. E. J. Econ. Anal. Policy 10(1):1–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, Kilmer B, Wagenaar AC, Chaloupka FJ, Caulkins JP. 2014bDeveloping public health regulations for marijuana: lessons from alcohol and tobacco. Am. J. Public Health 104(6):1021–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, Lundberg R. 2014. Why changes in price matter when thinking about marijuana policy: a review of the literature on the elasticity of demand. Public Health Rev. 35(2):1–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, MacCoun R, Reuter P, Chriqui J, Kilmer B, et al. 2005. What does it mean to decriminalize marijuana? A cross-national empirical examination In Substance Abuse: Individual Behaviour, Social Interactions, Markets and Politics, Vol. 16, ed. Grossman M, Lindgren B, pp. 347–70. Amsterdam: Elsevier; [PubMed] [Google Scholar]
- Pacula RL, Powell D, Heaton P, Sevigny E. 2015. Assessing the effects of medical marijuana laws on marijuana: The devil is in the details. J. Public Policy Anal. Manag 34:7–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, Sevigny EL. 2014aMarijuana liberalization policies: why we can’t learn much from policy still in motion. J. Policy Anal. Manag 33(1):212–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, Sevigny EL. 2014b. Natural experiments in a complex and dynamic environment: the need for measured assessment of the evidence. J. Policy Anal. Manag 33(1):232–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pertwee R 2014. Handbook of Cannabis. Oxford, UK: Oxford Univ. Press [Google Scholar]
- Raphael S, Stoll MA. 2013. Why Are So Many Americans in Prison? New York: Russell Sage Found. [Google Scholar]
- Rendon J 2013. Super-Charged: How Outlaws, Hippies, and Scientists Reinvented Marijuana. Portland, OR: Timber Press [Google Scholar]
- Reuter P, Hirschfield P, Davies C. 2001. Assessing the Crackdown on Marijuana in Maryland. Baltimore, MD: Abell Found. [Google Scholar]
- Reuter P, MacCoun RJ. 1995. Assessing the legalization debate In Policies and Strategies to Combat Drugs in Europe, ed. Estievenart G, pp. 39–49. Amsterdam: Kluwer [Google Scholar]
- Ritter A, Livingston M, Chalmers J, Berends L, Reuter P. 2016. Comparative policy analysis for alcohol and drugs: current state of the field. Int. J. Drug Policy 31:39–50 [DOI] [PubMed] [Google Scholar]
- Ross A, Walker A. 2017. The impact of low-priority laws on criminal activity: evidence from California. Contemp. Econ. Policy In press 10.1111/coep.12179 [DOI] [Google Scholar]
- Russo EB, Guy GW, Robson PJ. 2007. Cannabis, pain, and sleep: lessons from therapeutic clinical trials of Sativex, a cannabis-based medicine. Chem. Biodivers 4(8):1729–43 [DOI] [PubMed] [Google Scholar]
- Saffer H, Chaloupka FJ. 1999. The demand for illicit drugs. Econ. Inq 37(3):401–11 [Google Scholar]
- Salomonsen-Sautel S, Sakai JT, Thurstone C, Corley R, Hopfer C. 2012. Medical marijuana use among adolescents in substance abuse treatment. J. Am. Acad. Child Adolesc. Psychiatry 51(7):694–702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schauer GL, King BA, Bunnell RE, Promoff G, McAfee TA. 2016. Toking, vaping, and eating for health or fun: marijuana use patterns in adults, U.S., 2014. Am. J. Prev. Med 50(1):1–8 [DOI] [PubMed] [Google Scholar]
- Schuermeyer J, Salomonsen-Sautel S, Price RK, Balan S, Thurstone C, et al. 2014. Temporal trends in marijuana attitudes, availability and use in Colorado compared to non-medical marijuana states: 2003–2011. Drug Alcohol Depend. 140:145–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevigny EL. 2014. Medical marijuana by the numbers Presented at Annu. Conf. Int. Soc. Study Drug Policy, 8th, Rome [Google Scholar]
- Sevigny EL, Pacula RL, Heaton P. 2014. The effects of medical marijuana laws on potency. Int. J. Drug Policy 25:308–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Single E 1989. The impact of marijuana decriminalization: an update. J. Public Health Policy 10:456–66 [PubMed] [Google Scholar]
- Smart R 2016. Essays on the effects of medical marijuana laws PhD Thesis, Univ. Calif., Los Angeles [Google Scholar]
- Sobesky M, Gorgens K. 2016. Cannabis and adolescents: exploring the substance misuse treatment provider experience in a climate of legalization. Int. J. Drug Policy 33:66–74 [DOI] [PubMed] [Google Scholar]
- Stringer RJ, Maggard SR. 2016. Reefer madness to marijuana legalization: media exposure and American attitudes toward marijuana (1975–2012). J. Drug Issues 46(4):428–45 [Google Scholar]
- Subbaraman MS, Kerr WC. 2015. Simultaneous versus concurrent use of alcohol and cannabis in the National Alcohol Survey. Alcohol. Clin. Exp. Res 39(5):872–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subritzky T, Pettigrew S, Lenton S. 2016. Issues in the implementation and evolution of the commercial recreational cannabis market in Colorado. Int. J. Drug Policy 27:1–12 [DOI] [PubMed] [Google Scholar]
- Sumnall HR, Tyler E, Wagstaff GF, Cole JC. 2004. A behavioural economic analysis of alcohol, amphetamine, cocaine and ecstasy purchases by polysubstance misusers. Drug Alcohol Depend. 76(1):93–99 [DOI] [PubMed] [Google Scholar]
- Temple EC, Brown RF, Hine DW. 2011. The “grass ceiling”: Limitations in the literature hinder our understanding of cannabis use and its consequences. Addiction 106:238–44 [DOI] [PubMed] [Google Scholar]
- Terry-McElrath YM, O’Malley PM, Johnston LD. 2014. Alcohol and marijuana use patterns associated with unsafe driving among U.S. high school seniors: high use frequency, concurrent use, and simultaneous use. J. Stud. Alcohol Drugs 75(3):378–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thies CF, Register CA. 1993. Decriminalization of marijuana and the demand for alcohol, marijuana and cocaine. Soc. Sci. J 30(4):385–99 [Google Scholar]
- Thurstone C, Lieberman SA, Schmiege SJ. 2011. Medical marijuana diversion and associated problems in adolescent substance treatment. Drug Alcohol Depend. 118(2–3):489–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Baler RD, Compton WM, Weiss SRB. 2014. Adverse health effects of marijuana use. N. Engl. J. Med 370:2219–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall MM, Poh E, Cerdà M, Keyes KM, Galea S, Hasin DS. 2011. Adolescent marijuana use from 2002 to 2008: higher in states with medical marijuana laws, cause still unclear. Ann. Epidemiol 21(9):714–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen H, Hockenberry JM, Cummings JR. 2015. The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. J. Health Econ. 42:64–80 [DOI] [PubMed] [Google Scholar]
- Whiting PF, Wolff RF, Deshpande S, Di Nisio M, Duffy S, et al. 2015. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA 313(24):2456–73 [DOI] [PubMed] [Google Scholar]
- Williams AR, Olfson M, Kim JH, Martins SS, Kleber HD. 2016. Older, less regulated medical marijuana programs have much greater enrollment rates than newer “medicalized” programs. Health Aff. 35(3):480–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams J, Mahmoudi P. 2004. Economic relationship between alcohol and cannabis revisited. Econ. Rec 80(248):36–48 [Google Scholar]
- Zeisser C, Thompson K, Stockwell T, Duff C, Chow C, et al. 2012. A “standard joint”? The role of quantity in predicting cannabis-related problems. Addict. Res. Theory 20(1):82–92 [Google Scholar]