Abstract
Objectives
The purpose of this study was to examine the bactericidal efficacy of hydrogen peroxide (H2O2) on Cutibacterium acnes (C. acnes). We hypothesize that H2O2 reduces the bacterial burden of C. acnes.
Methods
The effect of H2O2 was assessed by testing bactericidal effect, time course analysis, growth inhibition, and minimum bactericidal concentration. To assess the bactericidal effect, bacteria were treated for 30 minutes with 0%, 1%, 3%, 4%, 6%, 8%, or 10% H2O2 in saline or water and compared with 3% topical H2O2 solution. For time course analysis, bacteria were treated with water or saline (controls), 3% H2O2 in water, 3% H2O2 in saline, or 3% topical solution for 5, 10, 15, 20, and 30 minutes. Results were analyzed with a two-way analysis of variance (ANOVA) (p < 0.05).
Results
Minimum inhibitory concentration of H2O2 after 30 minutes is 1% for H2O2 prepared in saline and water. The 3% topical solution was as effective when compared with the 1% H2O2 prepared in saline or water. The controls of both saline and water showed no reduction of bacteria. After five minutes of exposure, all mixtures of H2O2 reduced the percentage of live bacteria, with the topical solution being most effective (p < 0.0001). Maximum growth inhibition was achieved with topical 3% H2O2.
Conclusion
The inexpensive and commercially available topical solution of 3% H2O2 demonstrated superior bactericidal effect as observed in the minimum bactericidal inhibitory concentration, time course, and colony-forming unit (CFU) inhibition assays. These results support the use of topical 3% H2O2 for five minutes before surgical skin preparation prior to shoulder surgery to achieve eradication of C. acnes for the skin.
Cite this article: P. Hernandez, B. Sager, A. Fa, T. Liang, C. Lozano, M. Khazzam. Bactericidal efficacy of hydrogen peroxide on Cutibacterium acnes. Bone Joint Res 2019;8:3–10. DOI: 10.1302/2046-3758.81.BJR-2018-0145.R1.
Keywords: Cutibacterium acnes, Shoulder, Hydrogen peroxide, Infection, Treatment, Shoulder arthroplasty
Article focus
The purpose of this study is to investigate the antibacterial potential of H2O2 for the eradication of C. acnes.
Key messages
Hydrogen peroxide has both bactericidal as well as bacteriostatic properties against C. acnes. The minimum time for hydrogen peroxide to produce its bactericidal effect on C. acnes is five minutes.
Strengths and limitations
This is the first investigation to examine the bacteriocidal properties of hydrogen peroxide for C. acnes.
This is a proof-of-concept pilot study and therefore only utilizes lab isolates of C. acnes; it is unknown if hydrogen peroxide is equally as effective with clinical isolates.
The tissue toxicity of hydrogen peroxide at the minimal inhibitory concentration found in this investigation is unknown.
Introduction
Cutibacterium acnes (C. acnes), formerly named Propionibacterium acnes, is one of the most common causative organisms causing infection following shoulder surgery.1-4 Multiple attempts have been made to provide consistent, reproducible methods of decolonization and/or eradication of this troublesome organism preoperatively in an effort to reduce the risk of surgical site contamination and infection.5-10 Cutibacterium acnes is a slow-growing, facultative anaerobic Gram-positive bacillus commonly residing in the deep dermal layer of the skin within the pilosebaceous glands and hair follicles.4,5,9,11,12 This location not only makes C. acnes difficult to eradicate during surgical skin preparation because of poor penetration, but also puts the patient at risk of contamination of the shoulder joint due to repeated contact with this layer beneath the epidermis.2,4-6,10,11,13,14 It has been hypothesized that C. acnes inoculates the surgical wound once incision is made through the pilosebaceous glands.11,15
Additional attempts have been made to decolonize the skin utilizing antibiotics, either systemically or via topical application, with varying degrees of success.5,8,16-18 This bacteria has been shown to be susceptible to several antibiotics including penicillin G, amoxicillin, cephalothin, ceftriaxone, clindamycin, doxycycline, and rifampin.16,17 The issue that arises following administration of antibiotics is the emergence of resistance, with several recent reports of increasing resistance to clindamycin, doxycycline, tetracycline, minocycline, and erythromycin.17,19-22 Despite this susceptibility, recent studies4,15 have demonstrated prophylactic intravenous antibiotics prior to skin incision to be ineffective and to continue to result in positive C. acnes cultures. Thus far, routine skin preparation and intravenous perioperative antibiotics have not been shown to provide antimicrobial protection against C. acnes.
Two recent studies5,9 evaluated the effectiveness of topically applied benzoyl peroxide perioperatively. These studies demonstrated an almost 50% reduction in positive superficial cultures5,9 and, when combined with topical clindamycin, positive deep cultures decreased from 19.6% to 3.1%.5 Topical benzoyl peroxide has been proven to be an effective treatment, as it is lipophilic and can penetrate the deep dermal layer as well as release free oxygen radicals.23-26 These free radicals result in oxidation of proteins in bacterial cell membranes with subsequent cell death. While this method seems to be effective, it utilizes an antibiotic and can develop resistance to treatment. Furthermore, these treatments require patient compliance with the perioperative topical treatment regimen. Allhorn et al27 describe a novel antioxidant enzyme, radical oxygenase of Propionibacterium acnes (RoxP), which is produced by the bacteria to protect against oxidation and is hypothesized to facilitate its survival on skin. We are unaware of any studies describing the effectiveness of this enzyme when the bacteria have not had time to adapt to exposure to a new strongly oxidative product.
Hydrogen peroxide (H2O2) is cheap, widely available, and can be applied at the time of surgery. Given that H2O2 is not an antibiotic, there is no risk for development of resistant C. acnes strains. In theory, the aerobic environment created in the presence of H2O2 should be detrimental to anaerobic bacteria. It has been well established that polymorphonuclear leucocytes (PMNs) eliminate microorganisms through the generation of reactive oxygen free radicals, and utilize H2O2 to facilitate this respiratory burst mechanism resulting in cell death.28
The purpose of this study is to investigate the antibacterial potential of H2O2 for the eradication of C. acnes. To our knowledge, no study has been performed evaluating the efficacy of H2O2 in reducing the burden of C. acnes. We hypothesize that H2O2 will be an effective bactericidal treatment against C. acnes.
Materials and Methods
Cutibacterium acnes (ATCC 6919) was cultured in tryptic soy broth (TSB; Becton, Dickinson and Company, Franklin Lakes, New Jersey) with 5% defibrinated sheep blood (DSB) and plated on TSB agar with 5% DSB (TSB-DSB agar), at 37°C under anaerobic conditions using Gas-pak (Becton, Dickinson and Company). Both liquid media and agar plates were pre-reduced for 24 hours before C. acnes culture. All pre-inoculums were made from a single colony in 2 ml broth.
Two inoculums of 25 ml each were started with a 1:100 dilution from 24-hour pre-inoculums (107 colony-forming units (CFUs)). The cell number was calculated after a colony count of serial dilutions. Serial dilutions were prepared from 100 ml samples taken at 0, 6, 24, 30, 48, 54, 78, and 97 hours of growth, and cultured in duplicate on TSB-DSB agar. The plates were incubated at 37ºC for five days under anaerobic conditions. After the incubation period, viable colonies were counted and the number of CFUs per millilitre of culture (CFU/ml) was determined. The generation time (gt) was calculated according to Hall et al,29 using the following formula, where and are final and initial CFU per ml, and are final and initial times in hours, and K = log2 = 0.301:
Dilutions of 1%, 3%, 4%, 6%, 8%, and 10% H2O2 were freshly prepared with Milli-Q water or 0.85% sodium chloride (NaCl) (saline) from a 30% H2O2 solution (Fisher Bioreagents, Pittsburgh, Pennsylvania) and compared with a commercial solution of stabilized 3% topical H2O2 in water (topical solution) (Henry Schein Inc., Melville, New York). Pre-inoculums and 1:100 dilution inoculums were grown in TSB-DSB broth. At 50 hours of culture (109 CFUs), bacteria were centrifuged at 4300 × g for ten minutes, resuspended in saline and divided into 15 tubes. Each tube was treated for 30 minutes at room temperature with one of the following conditions: saline only, water only, 1%, 3%, 4%, 6%, 8%, or 10% H2O2 prepared in saline, the same dilutions prepared in water, or 3% topical solution. Tubes were centrifuged at 10 000 × g for five minutes and resuspended in 1 ml of saline. From this, 10 µl of serial dilutions up to 1/100 000 v/v were plated by duplicate on TSB-DSB agar. After incubation under the same conditions as above, colonies were counted and the minimum inhibitory concentration (MIC) was calculated. From the 1/10 v/v dilution of: a) saline; b) water; c) 3% H2O2 prepared in saline; d) 3% H2O2 prepared in water; and e) topical solution, 100 µl were plated as lawn in TSB-DSB agar for up to five days.
Fresh H2O2 dilutions in water and saline were prepared as previously mentioned for dose response. For this experiment, pre-inoculums and 1:50 dilution inoculums were grown in TSB without blood. Bacteria were centrifuged at 4300 × g for ten minutes, washed in saline once, and divided into 19 tubes. Each one was incubated in one of the following conditions: 3% H2O2 prepared in saline; 3% H2O2 prepared in water; or 3% topical solution for 0, 5, 10, or 15 minutes at room temperature. Saline-only and water-only controls were incubated for 15 minutes. Bacteria were centrifuged at 10 000 × g for five minutes, which resulted in final incubation times of 5, 10, 15, and 20 minutes. Cells were resuspended in saline and stained with Live/Dead BacLight bacterial viability kit (Molecular Probes, Invitrogen, Waltham, Massachusetts) following the manufacturer’s instructions. A standard curve for each experiment was created by mixing the percentages of live and dead bacteria in saline. To obtain dead bacteria, tubes were exposed to 95°C for ten minutes. Plates were exposed to 480 nm for excitation with 520 nm (green) and 620 nm (red) emission.
Statistical analysis
A two-way analysis of variance (ANOVA) with Tukey’s test for multiple comparisons of time course data was performed with GraphPad Prism version 7 (GraphPad Software, La Jolla, California). Differences were considered significant when the p-value was less than 0.05. A one-way ANOVA with Dunnett’s post hoc test was performed to compare timepoints on each 3% H2O2 solution. A power analysis of time course data was performed with SigmaPlot 13.0 (Systat Software, Inc., San Jose, California) (Table I).
Table I.
Results of a power analysis of the five-minute data from the time course experiment
| Power for analysis of variance (ANOVA) | |
|---|---|
| Data source: 5 mins 3% H2O2 in saline vs 3% topical H2O2 | |
| Power | 1 |
| Difference in means | 65.73 |
| Standard deviation | 13.52 |
| Groups, n | 3 |
| Group size, n | 5 |
| Alpha | 0.05 |
| Data source: 5 mins 3% H2O2 in water vs 3% topical H2O2 | |
| Power | 1 |
| Difference in means | 74.13 |
| Standard deviation | 13.52 |
| Groups, n | 3 |
| Group size, n | 5 |
| Alpha | 0.05 |
Results
Reconstituted C. acnes was first plated in TSB-DSB agar in anaerobic conditions to produce single colonies. Controls included bacteria grown in aerobic conditions and non-cultured plates in both anaerobic and aerobic conditions. No colonies were observed in any of the controls. All colonies of C. acnes in plates shared the same characteristics: circular, convex, smooth, white, and opaque. We then characterized the growth of this C. acnes purified strain from ATCC for up to 97 hours of culture (Fig. 1). Our calculations for generation time (gt) were 4.39 hours, similar to the 5.1 hours previously described by Hall et al,29 who studied intraocular clinical isolates of subjects with chronic postoperative endophthalmitis.
Fig. 1.
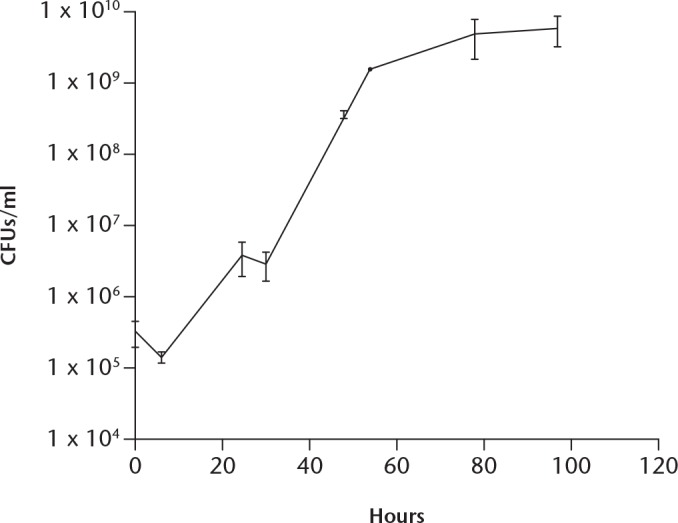
Growth curve of purified strain of C. acnes. Bacteria were grown in tryptic soy broth–defibrinated sheep blood (TSB-DSB) at 37ºC under anaerobic conditions. Samples were taken at 0, 6, 24, 30, 48, 54, 78, and 97 hours of growth and culture aliquots were plated on TSB-DSB agar. The calculated generation time (gt) is 4.39 hours. Data are presented as the mean (standard deviation) of two measurements. CFUs, colony-forming units.
For the consecutive experiments, we calculated that 50 hours of culture were necessary to obtain 109 CFUs.
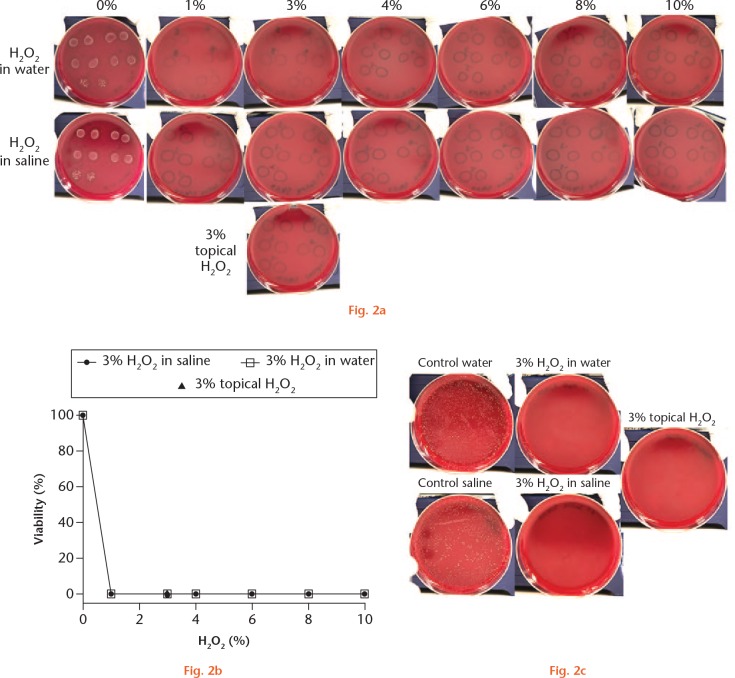
Bacteria were treated for 30 minutes with different percentages of H2O2 and compared with a commercial topical solution of stabilized 3% H2O2. Since the topical H2O2 is stabilized in water, we compared a fresh diluted H2O2 solution in both saline and water. Plates were incubated for five days in anaerobic conditions to allow the development of colonies. Results show that all the concentrations tested for H2O2 have effective bactericidal properties (Fig. 2). Negative controls of saline only and water only showed normal bacterial growth (Fig. 2a). The graph in Figure 2b shows that 1% H2O2 is the minimum bactericidal concentration (MBC) for C. acnes. The topical solution of H2O2 is as effective as 1% of a freshly prepared solution.
Minimum bactericidal concentration (MBC) was performed with a dose response of H2O2 prepared in saline and in water and compared with a 3% topical solution of H2O2. Bacteria were treated for 30 minutes on each solution (0% to 10%) and serial dilutions were seeded on tryptic soy broth–defibrinated sheep blood (TSB-DSB) agar. Colonies were counted after five days of incubation. All treatments are effective in their bactericidal activity. a) Representative image of three independent experiments. b) Graph of percentage of viability of C. acnes versus percentage of H2O2 grown in TSB showed a MBC of 1% for H2O2 prepared in saline and in water. Topical solution is equally effective. d) C. acnes treated for 30 minutes with 3% H2O2 prepared in saline, in water, or 3% topical solution were grown on TSB-DSB agar as lawn to further assess for bacterial growth inhibition. None of the treatments produced growth of colonies, while controls saline and water only show normal bacterial growth.
To corroborate the bactericidal effect of the 3% H2O2 solutions, treated C. acnes were seeded as lawn to observe growth inhibition (Fig. 2c). Results show that all H2O2 dilutions tested inhibit C. acnes growth. These results indicate that H2O2 has both a bactericidal and a bacteriostatic effect on this bacterium.
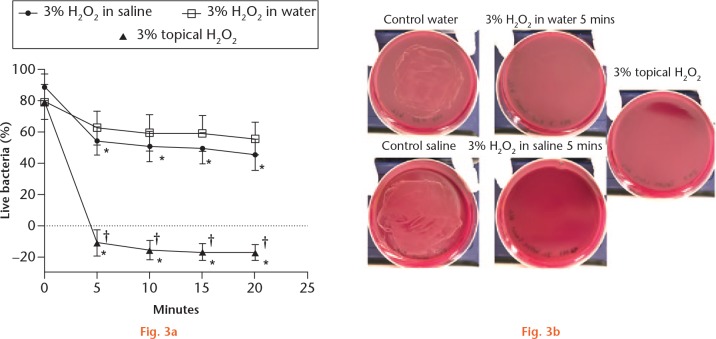
The minimum time required by H2O2 to produce its bactericidal effect on C. acnes was tested (Table II). The 3% H2O2 solutions as described previously were incubated for 5, 10, 15, and 20 minutes, and viability was assayed with Live/Dead BacLight bacterial viability assay (Fig. 3a). The results showed that, starting from five minutes, the 3% topical solution significantly decreases the viability of C. acnes compared with the water-only control (p < 0.0001), and it was superior in its bactericidal effect compared with 3% H2O2 prepared either in saline or water during all times analyzed (p < 0.0001). Bacteria treated for five minutes with each of the tested solutions were grown as lawn to further test growth inhibition (Fig. 3b). Only negative controls showed normal growth of C. acnes as lawn. None of the treatment solutions displayed any appearance of colonies.
Table II.
Results of the two-way analysis of variance (ANOVA) with Tukey’s test for multiple comparisons was performed on the time course data
| Test groups | Mean difference | 95% CI | Adjusted p-value |
|---|---|---|---|
| Time: 0 mins | |||
| 3% H2O2 in saline vs 3% H2O2 water | 9.418 | –23.07 to 41.9 | 0.7663 |
| 3% H2O2 in saline vs 3% topical H2O2 | 9.418 | –23.07 to 41.9 | 0.7663 |
| 3% H2O2 in water vs 3% topical H2O2 | 0 | –32.48 to 32.48 | > 0.9999 |
| Time: 5 mins | |||
| 3% H2O2 in saline vs 3% H2O2 in water | -8.396 | –40.88 to 24.09 | 0.8091 |
| 3% H2O2 in saline vs 3% topical H2O2 | 65.73 | 33.25 to 98.22 | < 0.0001* |
| 3% H2O2 in water vs 3% topical H2O2 | 74.13 | 41.64 to 106.6 | < 0.0001* |
| Time: 10 mins | |||
| 3% H2O2 in saline vs 3% H2O2 in water | -8.674 | –41.16 to 23.81 | 0.7977 |
| 3% H2O2 in saline vs 3% topical H2O2 | 66.75 | 34.26 to 99.23 | < 0.0001* |
| 3% H2O2 in water vs 3% topical H2O2 | 75.42 | 42.94 to 107.9 | < 0.0001* |
| Time: 15 mins | |||
| 3% H2O2 in saline vs 3% H2O2 in water | -9.61 | –42.09 to 22.87 | 0.758 |
| 3% H2O2 in saline vs 3% topical H2O2 | 66.83 | 34.35 to 99.32 | < 0.0001* |
| 3% H2O2 in water vs 3% topical H2O2 | 76.44 | 43.96 to 108.9 | < 0.0001* |
| Time: 20 mins | |||
| 3% H2O2 in saline vs 3% H2O2 in water | -10.39 | –42.87 to 22.1 | 0.7236 |
| 3% H2O2 in saline vs 3% topical H2O2 | 63.22 | 30.73 to 95.7 | < 0.0001* |
| 3% H2O2 in water vs 3% topical H2O2 | 73.61 | 41.12 to 106.1 | < 0.0001* |
Statistically significant
CI, confidence interval
Time course of H2O2 effect. a) Bacteria grown in tryptic soy broth (TSB) showed that a 3% topical solution is superior to the other solutions in its bactericidal effect, starting from five minutes of incubation. 3% H2O2 prepared in saline is not significantly different from 3% H2O2 prepared in water in any of the timepoints. *p < 0.0001 compared with control saline or water; †p < 0.0001 compared with 3% H2O2 prepared in saline or in water. b) Bacteria grown in tryptic soy broth–defibrinated sheep blood (TSB-DSB) agar and treated with each solution of H2O2 for five minutes was grown as lawn to further assess for growth inhibition. All treatment solutions inhibited bacterial growth except the controls with water or saline.
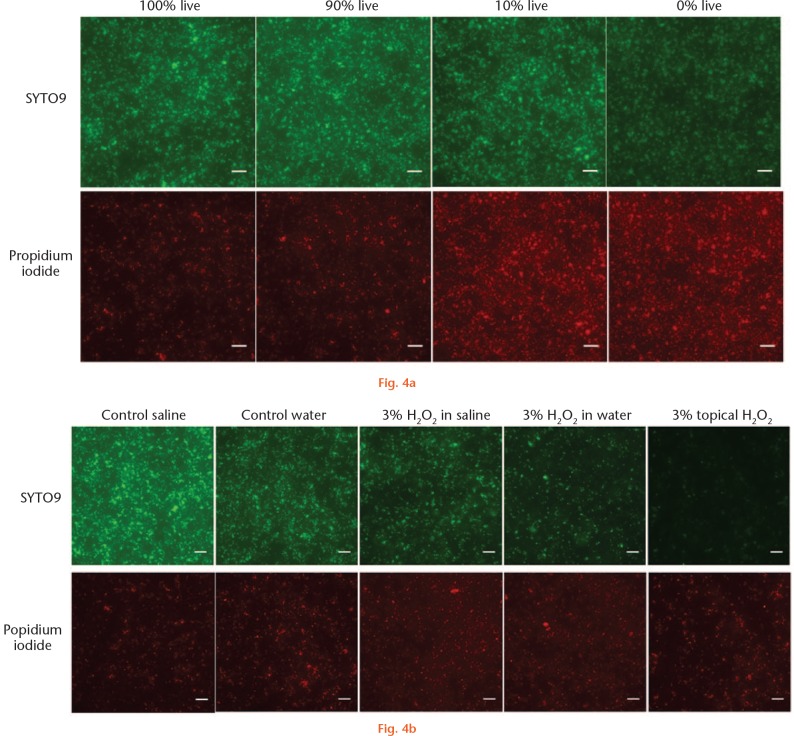
Bacteria stained with Live/Dead BacLight kit were viewed with a Nikon Eclipse Ti fluorescence microscope (Nikon Corp., Tokyo, Japan) to assess the staining profile and investigate the negative values of cell viability obtained for 3% topical solution. The standard curve for live/dead bacteria showed a gradual decrease in green staining (live cells), together with an increase in red staining (dead cells) (Fig. 4a). This was visible for both 3% H2O2 in saline and in water. However, topical solutions showed a decrease of fluorescence staining for both green and red (Fig. 4b). The findings for the topical H2O2 fluorescence staining indicate that this treatment results in not just cell death, but also complete cell destruction.
Bacterial viability after five minutes of treatment. Viability was tested with Live/Dead BacLight kit after five minutes of incubation with H2O2. a) Standard curve used for each experiment was obtained by mixing live bacteria with dead bacteria obtained by incubation at 95°C for ten minutes in saline. Green staining gradually decreased (from 100% to 0% live bacteria) while red increased (from 0% to 100% dead bacteria). b) Both 3% H2O2 solution prepared in saline and in water show a similar staining pattern, while 3% topical solution showed a decreased staining for both green and red dyes.
Discussion
The results of this study serve to validate the bactericidal and bacteriostatic properties of H2O2 against a specific bacterium, C. acnes. After treatment with H2O2, the colonies with C. acnes showed complete elimination of bacteria within five minutes. The oxidative reaction produced caused extensive damage and even destroyed the bacterial cells. After the treatments with H2O2, attempts to regrow the C. acnes produced negative results for at up to a week, a timepoint significantly longer than controls. The minimum inhibitory concentration of H2O2 for C. acnes is 1% solution prepared with either saline or water. More importantly, our results demonstrated that the commercially available topical solution is as effective as the 1% freshly prepared solution, indicating that it is as powerful as the lowest concentration of H2O2 solution. Additionally, our results found that the topical solution had a superior bactericidal effect compared with 3% H2O2 prepared in either saline or water, and found that the minimum time for bactericidal effect on C. acnes was five minutes.
Previous literature has shown that H2O2 has both bactericidal and bacteriostatic effect in vitro on other bacterium.28,30 To our knowledge, this is the first study to examine the efficacy of H2O2 as it pertains to C. acnes. The results of this study are powerful in that the H2O2 topical solution is low cost, with an average price of $1.30 (USD) for a 473.18 ml (16 ounce) bottle, and can be easily applied to the surgical field at any time during the surgical procedure. The ease of application provides a means of delivery to the deep dermal layer where sebaceous glands reside.
This study was undertaken in order to find a more efficacious form of skin preparation prior to shoulder surgery to reduce the bacterial burden of C. acnes and decrease the risk of deep contamination and potential infection. Studies have shown that culture-positive C. acnes patients may remain positive in nearly a third following treatment with chlorhexidine, and may be even double this at the end of a surgical procedure.6 The current ‘standard of care’ skin preparations are questionably effective in eliminating C. acnes colonization, therefore alternative skin preparations must be considered in order to reduce the incidence of postoperative infection by this troublesome bacterium. Although, to date, no study has been performed that looks explicitly at the effects of H2O2 on C. acnes colonization in vivo, there have been studies examining the cultures of shoulders after treatment with benzoyl peroxide, a similarly structured analogue. In this study, Sabetta et al9 showed that pre-treatment with benzoyl peroxide produced similarly low positive culture rates for C. acnes as a control swab, indicating the ability of the substance to penetrate the sebaceous glands and eliminate the bacterium.
A recent study by Namdari et al8 performed as a randomized controlled trial to evaluate the effectiveness of a preoperative course of oral doxycycline for seven days prior to shoulder arthroscopy to determine whether this treatment would reduce C. acnes colonization in males. The authors reported no difference in positive culture rates between the ‘no antibiotics’ and the doxycycline groups. The most alarming finding was 59.5% positive cultures in the no treatment group and 43.2% in the doxycycline group (p = 0.245). The results indicate minimal impact on C. acnes and the authors recommended against this type of prophylactic use, as there is potential risk for the emergence of resistance. These results also support the findings reported by Matsen et al15 and Falconer et al4 that indicate that current intravenous administered antibiotics given prior to skin incision do not eliminate C. acnes. Both of these studies found a 30% culture-positive rate despite perioperative antibiotics, thus supporting the need for additional/other interventions to eradicate this bacteria successfully at the time of surgery.
While this study certainly produces meaningful information, it has some limitations. This study is an in vitro analysis of the effects of H2O2 on C. acnes. Although the results show efficacy in the laboratory, the clinical utility has still not been investigated. In the laboratory, the H2O2 comes into direct contact with the bacterial membranes, allowing for aggressive destruction of cells, as demonstrated by the negative curve for the topical H2O2 solution in Figure 3a. In vitro, the bacteria tend to live in the pilosebaceous glands in the subcutaneous dermal layer of the skin, a location that is not readily accessible to most skin preparations.4,13 Another limitation is that we used only one bacterial reference strain, and while it is not common clinically to speciate bacterial strains of this organism, we do not know if clinical isolates of C. acnes would demonstrate the same susceptibility to H2O2. The efficacy of H2O2 is a topic for future investigation.
The use/application of H2O2 at the time of surgery will need to be at multiple locations to be able to get in contact with the bacteria and be effective. Although this is not an issue during open surgical procedures, H2O2 may not be as effective during arthroscopic shoulder surgery because its penetration into the deep dermal layer through topical application is unknown. While benzoyl peroxide has been shown to penetrate the pilosebaceous glands of the skin, no such study has been performed for H2O2.14 It is clear that it is not possible to eradicate C. acnes completely, and the focus and goal should be to decrease the bacterial burden in order to prevent contamination of the surgical field and not allow this troublesome bacteria to establish a biofilm deep within the shoulder.
In conclusion, hydrogen peroxide is a very potent antimicrobial against the bacterium Cutibacterium acnes. It is both bacteriostatic and rapidly bactericidal, even at low concentrations. The minimum bactericidal concentration of H2O2 for C. acnes is a 1% solution prepared in either saline or water. The commercially available topical 3% solution is equally as effective as the laboratory-prepared concentration. Within five minutes of exposure to H2O2, there is complete eradication of C. acnes in vitro. Further studies are needed to establish the depth of penetration through the epidermis to the deep dermal layers. With our current findings, the use of a topical solution of H2O2 as part of skin preparation prior to surgery may be a helpful tool to prevent C. acnes contamination during shoulder surgery. Additionally, application to the deep dermal layer once a skin incision has been made, and a final application to the deep dermal layer prior to skin closure, may be helpful in the eradication of this troublesome bacterium. Future studies are required in order to validate these recommendations clinically.
Footnotes
Author contributions: P. Hernandez: Designed the study, Collected and analyzed the data, Actively involved in the laboratory experiment, Wrote the manuscript.
B. Sager: Designed the study, Analyzed the data, Wrote the manuscript.
A. Fa: Collected the data, Actively involved in the laboratory experiment.
T. Liang: Collected the data, Actively involved in the laboratory experiment.
C. Lozano: Designed the study, Analyzed the data, Wrote the manuscript.
M. Khazzam: Developed the hypothesis, Designed the study, Analyzed the data, Wrote the manuscript.
Conflict of interest statement: None declared
Follow us @BoneJointRes
Funding statement
None declared
References
- 1. Scholz CF, Kilian M. The natural history of cutaneous propionibacteria, and reclassification of selected species within the genus Propionibacterium to the proposed novel genera Acidipropionibacterium gen. nov., Cutibacterium gen. nov. and Pseudopropionibacterium gen. nov. Int J Syst Evol Microbiol 2016;66:4422-4432. [DOI] [PubMed] [Google Scholar]
- 2. Mook WR, Klement MR, Green CL, Hazen KC, Garrigues GE. The incidence of propionibacterium acnes in open shoulder surgery: a controlled diagnostic study. J Bone Joint Surg [Am] 2015;97-A:957-963. [DOI] [PubMed] [Google Scholar]
- 3. Hudek R, Sommer F, Abdelkawi AF, et al. Propionibacterium acnes in shoulder surgery: is loss of hair protective for infection? J Shoulder Elbow Surg 2016;25:973-980. [DOI] [PubMed] [Google Scholar]
- 4. Falconer TM, Baba M, Kruse LM, et al. Contamination of the surgical field with propionibacterium acnes in primary shoulder arthroplasty. J Bone Joint Surg [Am] 2016;98-A:1722-1728. [DOI] [PubMed] [Google Scholar]
- 5. Dizay HH, Lau DG, Nottage WM. Benzoyl peroxide and clindamycin topical skin preparation decreases Propionibacterium acnes colonization in shoulder arthroscopy. J Shoulder Elbow Surg 2017;26:1190-1195. [DOI] [PubMed] [Google Scholar]
- 6. Lee MJ, Pottinger PS, Butler-Wu S, et al. Propionibacterium persists in the skin despite standard surgical preparation. J Bone Joint Surg [Am] 2014;96-A:1447-1450. [DOI] [PubMed] [Google Scholar]
- 7. Murray MR, Saltzman MD, Gryzlo SM, et al. Efficacy of preoperative home use of 2% chlorhexidine gluconate cloth before shoulder surgery. J Shoulder Elbow Surg 2011;20:928-933. [DOI] [PubMed] [Google Scholar]
- 8. Namdari S, Nicholson T, Parvizi J, Ramsey M. Preoperative doxycycline does not decolonize Propionibacterium acnes from the skin of the shoulder: a randomized controlled trial. J Shoulder Elbow Surg 2017;26:1495-1499. [DOI] [PubMed] [Google Scholar]
- 9. Sabetta JR, Rana VP, Vadasdi KB, et al. Efficacy of topical benzoyl peroxide on the reduction of Propionibacterium acnes during shoulder surgery. J Shoulder Elbow Surg 2015;24:995-1004. [DOI] [PubMed] [Google Scholar]
- 10. Saltzman MD, Nuber GW, Gryzlo SM, Marecek GS, Koh JL. Efficacy of surgical preparation solutions in shoulder surgery. J Bone Joint Surg [Am] 2009;91-A:1949-1953. [DOI] [PubMed] [Google Scholar]
- 11. Matsen FA, III, Butler-Wu S, Carofino BC, et al. Origin of propionibacterium in surgical wounds and evidence-based approach for culturing propionibacterium from surgical sites. J Bone Joint Surg [Am] 2013;95-A:e18111-e1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Booker SJ, Boyd M, Gallacher S, et al. The colonisation of the glenohumeral joint by Propionibacterium acnes is not associated with frozen shoulder but is more likely to occur after an injection into the joint. Bone Joint J 2017;99-B:1067-1072. [DOI] [PubMed] [Google Scholar]
- 13. Phadnis J, Gordon D, Krishnan J, Bain GI. Frequent isolation of Propionibacterium acnes from the shoulder dermis despite skin preparation and prophylactic antibiotics. J Shoulder Elbow Surg 2016;25:304-310. [DOI] [PubMed] [Google Scholar]
- 14. Seubert S, Seubert A, Ippen H. Penetration of benzoyl peroxide in the skin. Hautarzt 1984;35:455-458. (Article in German) [PubMed] [Google Scholar]
- 15. Matsen FA, III, Russ SM, Bertelsen A, Butler-Wu S, Pottinger PS. Propionibacterium can be isolated from deep cultures obtained at primary arthroplasty despite intravenous antimicrobial prophylaxis. J Shoulder Elbow Surg 2015;24:844-847. [DOI] [PubMed] [Google Scholar]
- 16. Crane JK, Hohman DW, Nodzo SR, Duquin TR. Antimicrobial susceptibility of Propionibacterium acnes isolates from shoulder surgery. Antimicrob Agents Chemother 2013;57:3424-3426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Khassebaf J, Hellmark B, Davidsson S, et al. Antibiotic susceptibility of Propionibacterium acnes isolated from orthopaedic implant-associated infections. Anaerobe 2015;32:57-62. [DOI] [PubMed] [Google Scholar]
- 18. Rao AJ, Chalmers PN, Cvetanovich GL, et al. Preoperative doxycycline does not reduce propionibacterium acnes in shoulder arthroplasty. J Bone Joint Surg [Am] 2018;100-A:958-964. [DOI] [PubMed] [Google Scholar]
- 19. Leyden JJ, Preston N, Osborn C, Gottschalk RW. In-vivo effectiveness of adapalene 0.1%/benzoyl peroxide 2.5% gel on antibiotic-sensitive and resistant Propionibacterium acnes. J Clin Aesthetic Dermotol 2011;4:22-26. [PMC free article] [PubMed] [Google Scholar]
- 20. Furustrand Tafin U Aubin GG Eich G Trampuz A Corvec S. Occurrence and new mutations involved in rifampicin-resistant Propionibacterium acnes strains isolated from biofilm or device-related infections. Anaerobe 2015;34:116-119. [DOI] [PubMed] [Google Scholar]
- 21. Sardana K, Gupta T, Garg VK, Ghunawat S. Antibiotic resistance to Propionobacterium acnes: worldwide scenario, diagnosis and management. Expert Rev Anti Infect Ther 2015;13:883-896. [DOI] [PubMed] [Google Scholar]
- 22. Takoudju EM, Guillouzouic A, Kambarev S, Pecorari F, Corvec S. In vitro emergence of fluoroquinolone resistance in Cutibacterium (formerly Propionibacterium) acnes and molecular characterization of mutations in the gyrA gene. Anaerobe 2017;47:194-200. [DOI] [PubMed] [Google Scholar]
- 23. Fulton JE, Jr, Farzad-Bakshandeh A, Bradley S. Studies on the mechanism of action of topical benzyl peroxide and vitamin A acid in acne vulgaris. J Cutan Pathol 1974;1:191-200. [DOI] [PubMed] [Google Scholar]
- 24. Haider A, Shaw JC. Treatment of acne vulgaris. JAMA 2004;292:726-735. [DOI] [PubMed] [Google Scholar]
- 25. Leyden JJ. Effect of topical benzoyl peroxide/clindamycin versus topical clindamycin and vehicle in the reduction of Propionibacterium acnes. Cutis 2002;69:475-480. [PubMed] [Google Scholar]
- 26. Leyden JJ, Del Rosso JQ, Webster GF. Clinical considerations in the treatment of acne vulgaris and other inflammatory skin disorders: focus on antibiotic resistance. Cutis 2007;79(Suppl):9-25. [PubMed] [Google Scholar]
- 27. Allhorn M, Arve S, Brüggemann H, Lood R. A novel enzyme with antioxidant capacity produced by the ubiquitous skin colonizer Propionibacterium acnes. Sci Rep 2016;6:36412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hyslop PA, Hinshaw DB, Scraufstatter IU, et al. Hydrogen peroxide as a potent bacteriostatic antibiotic: implications for host defense. Free Radic Biol Med 1995;19:31-37. [DOI] [PubMed] [Google Scholar]
- 29. Hall GS, Pratt-Rippin K, Meisler DM, et al. Growth curve for Propionibacterium acnes. Curr Eye Res 1994;13:465-466. [DOI] [PubMed] [Google Scholar]
- 30. Baldry MG. The bactericidal, fungicidal and sporicidal properties of hydrogen peroxide and peracetic acid. J Appl Bacteriol 1983;54:417-423. [DOI] [PubMed] [Google Scholar]