Abstract
Objective
Adolescence is a period during which youth may begin experimenting with substances. Youth with overweight or obesity may be at increased risk for substance use, including cigarette smoking. Understanding the associations between smoking and excess weight and the pathways associated with increased likelihood for smoking initiation is of particular importance given the increased risk for negative health outcomes associated with each.
Methods
Using longitudinal panel data from 1,023 middle school youth (baseline age M = 12.5, 52% female), we tested whether smoking initiation was concurrently and prospectively predicted by self-reported body mass index (BMI) and whether self-esteem for physical appearance (SEPA) mediated the effect of BMI on risk of early initiation.
Results
BMI predicted smoking initiation concurrently and prospectively in unadjusted models. In adjusted models, SEPA mediated the effects of BMI on smoking initiation. Bootstrapped mediation results indicated that the positive relationship between BMI and subsequent smoking initiation was significantly mediated by lower SEPA (B =.10, 95% confidence interval [0.01, 0.22]).
Conclusions
Adolescents who have overweight or obesity are more likely to feel negatively about their appearance and bodies, and this negative perception may result in experimentation with cigarettes. Cigarettes may be used by youth with overweight or obesity in an effort to manage weight, to cope with low self-esteem or for other reasons. Future research should explore the motives and psychosocial context of smoking initiation among adolescents with overweight/obesity further (e.g., with whom they first try smoking, perceived benefits of smoking).
Keywords: at risk youth, health behavior, longitudinal research, obesity, tobacco use
Use of addictive substances and overweight/obesity are among priority youth health risks given their contributions to the leading causes of morbidity and mortality nationally (Kann, 2016). Adolescence is a sensitive period in which many adolescents initiate use of tobacco products, alcohol, and other drugs (Center for Behavioral Health Statistics and Quality, 2015), which is concerning because longitudinal research indicates that early-onset smoking is related to higher rates of nicotine dependence in later adulthood (Buchmann et al., 2013; Hu, Davies, & Kandel, 2006) as well as smoking-related morbidity and mortality (Fagerström, 2002; Huxley et al., 2012). In addition, the prevalence of obesity in children and adolescents has risen substantially in recent decades (Ng et al., 2014). Recent research has suggested that youth with overweight and obesity may be at increased risk for smoking (Farhat, Iannotti, & Simons-Morton, 2010; Lange, Thamotharan, Racine, Hirko, & Fields, 2015; Ratcliff, Jenkins, Reiter-Purtill, Noll, & Zeller, 2011; Seo, Jiang, & Kolbe, 2009). Understanding the relationship between excess weight and smoking is of particular importance given their unique and interactive health effects.
The social development model (Catalano, Kosterman, Hawkins, Newcomb, & Abbott, 1996; Hawkins, Lishner, Catalano, & Howard, 1986) may provide a conceptual framework for possible relationships between obesity and smoking initiation. This model suggests that deviant behavior, such as smoking, is a function of (1) the types of opportunities and social influences adolescents are exposed to, (2) the social, cognitive, and behavioral skills they possesses, and (3) the extent to which their behavior is rewarded. Adolescents with overweight and obesity report having a variety of negative social experiences (e.g., teasing, name-calling, and bullying) as a result of stigma, bias, and discrimination associated with their weight (Puhl & King, 2013; Puhl & Latner, 2007). In theory, these types of experiences may result in fewer opportunities for positive social involvement and reduce their self-esteem. Self-esteem in children and adolescents is thought to be multifaceted, with self-esteem for physical appearance (SEPA) believed to be an important domain for determining self-worth (Harter, 1985, 1993, 2012; Wichstraum, 1995). A review of studies on obesity and self-esteem demonstrated that, relative to non-obese youth, youth with obesity reported lower SEPA in all six of the studies examined (Griffiths, Parsons, & Hill, 2010). In one study, youth with overweight or obesity had more than double the risk of having low SEPA and had greater body dissatisfaction relative to those in the normal weight range (Franklin, Denyer, Steinbeck, Caterson, & Hill, 2006). It is possible that youth with overweight and obesity and low SEPA may miss opportunities to develop needed skills and rely on ineffective coping. Among youth with overweight/obesity, lower SEPA also was associated with being bullied (Danielsen et al., 2012; Fox & Farrow, 2009) and having more eating disturbances (e.g., eating to comfort oneself and guilt about eating) (Danielsen et al., 2012). In adolescents, disengagement coping (e.g., getting angry when experiencing a problem or giving up on it) was associated with greater likelihood of early onset of substance use (smoking cigarettes/drinking alcohol/smoking marijuana) (Wills, Sandy, Yaeger, Cleary, & Shinar, 2001). Thus, among those with overweight/obesity, feeling particularly helpless and angry about one’s weight and other stigmatizing experiences could lead to eating or smoking to comfort oneself rather than using more effective strategies.
While, theoretically, overweight and obesity and the lower SEPA that can result may provide fewer opportunities for positive, rewarding, prosocial interactions and influence the skills an adolescent acquires, there have been a limited number of studies examining the association between SEPA and smoking among youth and findings have been inconsistent. When number of days of cigarette use in the past month and SEPA were assessed in a cross-sectional study of 7th and 8th grade students, there was not a significantly association (Lifrak, McKay, Rostain, Alterman, & O’brien, 1997). In a cross-sectional study of youth of age 11–15 years that examined relationships separately by gender, girls with lower SEPA had greater odds of using cigarettes some of the time or regularly, but this was not observed among boys (Minagawa, While, & Charlton, 1993). Another study assessed youth annually for 4 years beginning at age 8 and reported an inverse association between SEPA and having tried smoking when assessed concurrently but not prospectively (Barlow & Woods, 2009). Finally, in a prospective study of 8th grade students, SEPA did not predict likelihood of reporting having smoked 3 weeks later, possibly because of the short time studied (Dolcini & Adler, 1994).
While research has been conducted to understand the relationship between obesity and SEPA, and smoking and SEPA, separately, research to better understand the interrelationships between all three variables is needed. The current study sought to elucidate the risk of excess weight (using self-reported body mass index [BMI] as a continuous measure of adiposity) on the initiation of smoking among adolescents (i.e., adolescents reporting having tried or experimented with cigarette smoking) including possible mechanistic risk associated with low SEPA. We examined both concurrent and prospective relationships; testing concurrent associations includes the subset of youth who had already initiated smoking at baseline, whereas modeling data prospectively permits an unambiguous examination of smoking initiation among those with no prior experimentation (i.e., smoking-naïve). A sample of 6th, 7th, and 8th graders followed longitudinally was used to test the following hypotheses: (1) at all time points, higher BMI would be associated with lower SEPA; (2) concurrently, higher BMI would be associated with greater likelihood of ever having tried smoking; (3) prospectively, higher BMI would predict greater likelihood of future smoking initiation; and (4) lower SEPA would account for the prospective association between BMI and smoking initiation.
Method
Participants
Data were taken from a sample of 1,023 students enrolled in a prospective study on drinking initiation and progression (Jackson, Barnett, Colby, & Rogers, 2015; Jackson, Colby, Barnett, & Abar, 2015). At enrollment, the sample was 52% female, 24% non-White (5% Black, 3% Asian, 2% American Indian, 8% mixed race, and 6% other), and 12% Hispanic and comprised roughly equal numbers of 6th, 7th, and 8th graders (33%, 32%, and 35%, respectively). Mean age at enrollment was 12.5 years (range: 10–15, SD = 1.0). The sample was more racially diverse and less socioeconomically disadvantaged than the school populations from which it was drawn but was representative with respect to gender and grade (Jackson, Colby, et al., 2015).
Procedures
All procedures were approved by the university institutional review board. Participants were recruited from six middle schools in the Northeastern United States. Five school cohorts were enrolled on a semiannual basis from 2009 to 2011. Students received information about the study via mail and teachers; those who were interested (initial response rate of 38% of those informed of the study) and for whom written parental consent was obtained (65% of those who returned consent forms) were invited to participate in an after-school session; 88% of these youth were enrolled into the study. During this session, the project was explained to the students by project staff. Assent was obtained from each student, and each completed a 45-min computerized baseline survey. A Certificate of Confidentiality was obtained from the National Institute on Alcohol Abuse and Alcoholism to preserve participant confidentiality.
Participants completed a total of five biannual surveys (T1–T5) across 2 years and a follow-up survey 1 year later (T6); all surveys were Web-based. Participants received $25 for completion of the baseline (T1) survey and $20 for completion of each of the follow-up surveys. Response rates were 90% at T2, 86% at T3, 83% at T4, 81% at T5, and 82% at T6. Compared with characteristics of the full sample at the time of enrollment, nonresponse at any subsequent time point was not associated with age, t(1,021) = −.67, p = .50, but was associated with male gender, χ2(1, N = 1,023) = 7.29, p < .007, non-White race, χ2(1, N = 1,023) = 8.12, p < .004, Hispanic ethnicity, χ2(1, N = 1,023) = 12.74, p < .002, and lower socioeconomic status (SES), χ2(2, N = 898) = 19.33, p < .001.
Measures
Demographic Factors
At enrollment, gender, race, ethnicity (Hispanic/non-Hispanic), and age were obtained via self-report; receipt of lunch subsidy was used as a proxy for SES, obtained via parent-report (90% of sample).
Body Mass Index
At each time point, participants provided self-report of height and weight. According to the Centers for Disease Control and Prevention (CDC), BMI in children and teens must be interpreted relative to other youth of the same sex and age (Centers for Disease Control and Prevention, 2015). The CDC provides an Excel spreadsheet calculator tool for use by schools and other professionals who want to compute BMI for groups of up to 20,000 youth (https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/tool_for_schools.html). This tool, which determines BMI based on the standard formula [(weight in pounds * 703)/height in inches2] and provides percentiles calculated from the CDC growth charts based on age and sex, was used to calculate BMI and BMI percentile.
Self-Esteem for Physical Appearance
The six-item SEPA domain from the Harter’s Self-Perception Profile (Harter, 2012; Wichstraum, 1995). On each item, participants are first asked: “Which kids are most like you?” followed by two possibilities (e.g., “some kids are happy with the way they look” and “some kids are not happy with the way they look”). After selecting an option, they then indicated whether this description was “sort of true for me” (3 for positive physical appearance, and 2 for negative physical appearance) or “really true for me” (4 for positive physical appearance and 1 for negative physical appearance). Means response on the six items were calculated at T2 and T4. Cronbach’s alphas were .88 and .89, respectively.
Smoking Initiation
At each time point, smoking initiation was assessed with the question: “Have you ever tried or experimented with cigarette smoking, even a few puffs/drags?” (1: Yes, 2: No) from the Smoking Uptake Continuum questionnaire (Choi, Gilpin, Farkas, & Pierce, 2001). For T1, the dichotomous variable was left unchanged. For each subsequent study year, a dichotomous variable represented whether smoking initiation had occurred, given that it had not occurred previously (1 = event occurred, 0 = event has not yet occurred). To capture only new initiation at each time point, those who reported initiation at an earlier time point or for whom data were not available were set as missing in the analytic model.
Analytic Strategy
Pearson’s correlations were used to assess relationships between SEPA and BMI (Hypothesis 1). To test, whether BMI predicted concurrent smoking initiation (Hypothesis 2), we performed logistic regression with T1 smoking initiation as the dependent variable, and T1 BMI as the predictor. Gender and all demographic characteristics that were significantly associated with smoking initiation at any time point (see Table I) were included as covariates to avoid confounding sociodemographic factors.
Table I.
Univariate Statistics and Correlations (N = 1,023)
| M or % | SD | Range | SI (T1) | SI (T3) | SI (T5) | SI (T6) | SEPA (T2) | SEPA (T4) | |
|---|---|---|---|---|---|---|---|---|---|
| SI n (%) | 90 (8.8) | 135 (13.6) | 178 (18.7) | 215 (24.0) | |||||
| Female (%)a | 52.2 | 54.4 | 56.3 | 56.7 | 57.2 | −.22*** | −.29*** | ||
| Hispanic (%)a | 12.1 | 16.7 | 15.6 | 13.5 | 12.6 | −.08* | −.08* | ||
| Non-White (%)a | 17.0 | 26.7* | 26.7** | 24.2** | 23.3** | −.11** | −.11** | ||
| Received lunch subsidy (%)a | 33.9 | 71.2*** | 67.9*** | 62.4*** | 57.9*** | −.13** | −.11** | ||
| Age (T1) | 12.5 | 1.0 | [10, 15] | .21*** | .19*** | .21*** | .20*** | −.09** | −.09* |
| BMI (T1)b | 58.0 | 29.6 | [0, 99.6] | .08* | .10** | .11*** | .12*** | −.28*** | −.30*** |
| Male (n = 489) | 59.2 | 29.6 | [0, 99.6] | .04 | .09 | .09 | .08 | −.26*** | −.30*** |
| Female (n = 534) | 56.8 | 29.6 | [0, 99.6] | .11* | .12** | .13* | .17*** | −.26*** | −.32*** |
| BMI (T3)b | 60.2 | 28.9 | [0, 99.6] | .09** | .11*** | .10** | .11** | −.25*** | −.32*** |
| Male (n = 489) | 62.1 | 29.8 | [0, 99.6] | .07 | .12** | .15** | .11* | −.20*** | −.28*** |
| Female (n = 534) | 58.5 | 28.1 | [0, 99.5] | .11* | .10* | .07* | .11* | −.27*** | −.33*** |
| BMI (T5)b | 60.0 | 28.2 | [0, 99.7] | .13*** | .12*** | .13*** | .15*** | −.22*** | −.27*** |
| Male (n = 489) | 60.7 | 29.2 | [0, 99.7] | .12* | .15** | .17*** | .16** | −.10 | −.24*** |
| Female (n = 534) | 59.4 | 27.3 | [0, 99.5] | .13** | .10* | .11* | .15** | −.25*** | −.31*** |
| SEPA (T2)c | 2.9 | 0.9 | [1, 4] | −.14*** | −.16*** | −.16*** | −.17*** | − | .63*** |
| SEPA (T4)c | 2.8 | 0.9 | [1, 4] | −.11** | −.13*** | −.16*** | −.20*** | – | – |
Note. BMI = body mass index percentile based on youth of the same age and sex from self-reported height and weight; SEPA = self-esteem for physical appearance; SI = smoking initiation; T = time point in study.
Dichotomized groups coded: 0 = male, 1 = female; 0 = Non-Hispanic, 1 = Hispanic; 0 = White, 1 = non-White; 0 = no lunch subsidy, 1 = reduced-price/free lunch; Pearson’s chi-square used to test differences in smoking initiation; Percentages show proportion of adolescents initiating who endorsed the demographic characteristic referenced in the first column.
Percent overweight/obese at T1, T3, and T5 were 24.0%, 26.3%, and 23.3%, respectively.
Females had lower SEPA scores at T2 (M = 2.71, SD = 0.96) and T4 (M = 2.57, SD = 0.93) than did males (T2 M = 3.11, SD = 0.81; T4 M = 3.11, SD = 0.81)), t(930) = −6.87, p < .001 and t(865) = −8.91, p < .001, respectively.
*p < .05; **p < .01; ***p < .001.
To assess whether BMI predicted subsequent smoking initiation (Hypothesis 3), and whether SEPA mediated the link between BMI and subsequent initiation (Hypothesis 4), we conducted two sets of discrete-time hazard regression models in the context of structural equation models using Mplus Version 8 (Muthen & Muthen, 2007). For these analyses, we restricted the sample to those who did not report smoking initiation at T1 (N = 933 smoking-naïve). For these models, smoking initiation was defined in a discrete-time hazard regression where the log odds of initiation were conditional on the predictors, given that initiation had not occurred at a previous wave (Singer & Willett, 2003).
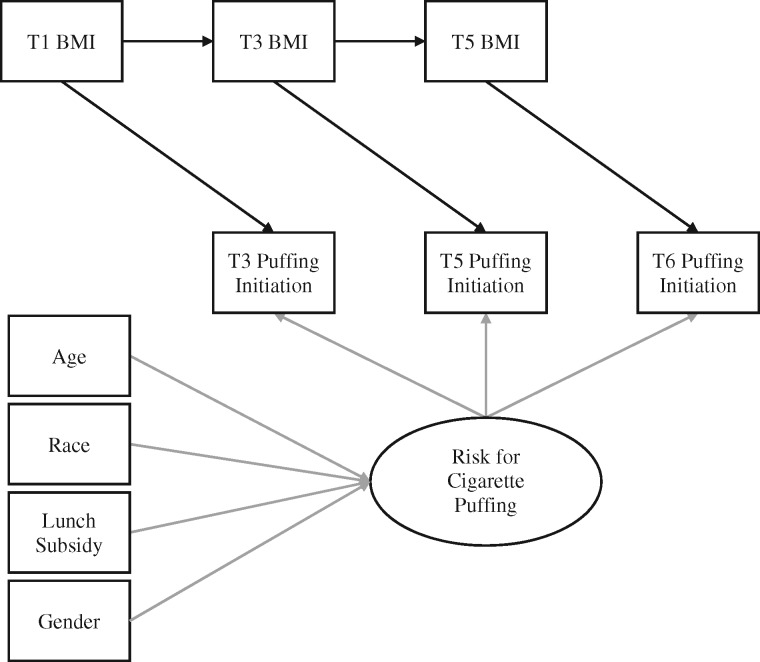
Figure 1 illustrates the model used to test Hypothesis 3. While the latent factor representing discrete-time initiation was regressed on sociodemographic covariates,1 specific indicators of smoking initiation were regressed on standardized predictors assessed at the previous time point (Muthen & Muthen, 2007). To determine whether to model the relationship between BMI and smoking initiation using time-invariant effects (i.e., effect of BMI constrained to be equal across measurement periods) or independently estimated effects (i.e., effects of T1, T3, and T5 BMI freely estimated), we investigated changes in model fit based on significance of a Wald test comparing the two models. A nonsignificant Wald test indicates that a constrained model fits the data significantly better than the model in which effects were freely estimated, suggesting that time-invariant effects should be modeled.
Figure 1.
Model of discrete-time survival with lagged BMI as predictor.
Note. Among smoking-naïve, we predict cigarette smoking initiation at three yearly follow-ups (T3, T5, and T6). In discrete-time survival modeling, the hazard of initiation is estimated and predicted, assuming initiation did not occur previously. Therefore, lagged BMI is assessed at the time point before risk of initiation. The prediction of the latent variable lets us control for time-invariant effects. BMI = body mass index percentile based on youth of the same age and sex from self-reported height and weight.
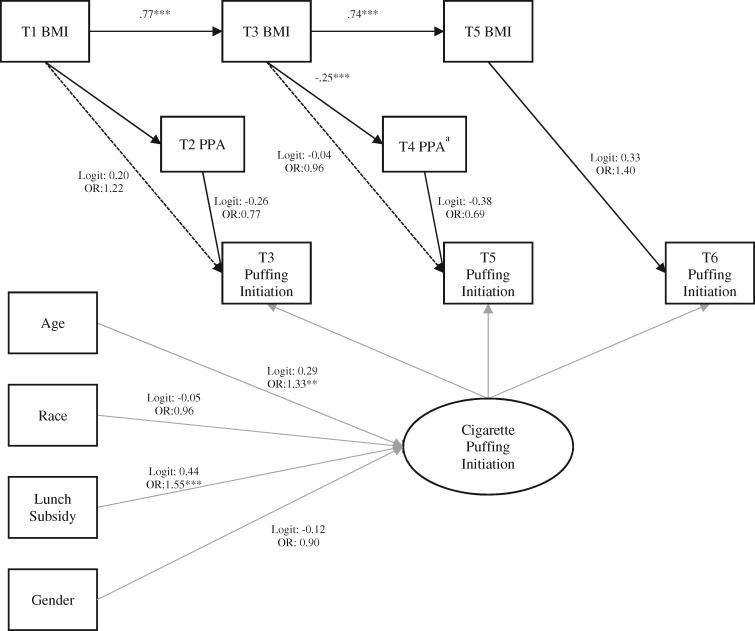
To test Hypothesis 4 (mediation), the model included both BMI and SEPA as predictors, with T1 BMI and T2 SEPA predicting T3 smoking initiation, with T3 BMI and T4 SEPA predicting T5 smoking initiation, and with T5 BMI predicting T6 smoking initiation (see Figure 2). Time-varying effects of BMI and SEPA were modeled to satisfy the requirement of directionality (temporality) for testing mediation, as a time-invariant test would have modeled the effect of T3 BMI on T4 SEPA for people who had already onset before T3, leading to a violation of temporal order. We evaluated whether significant mediation occurred by estimating the bias-corrected bootstrapped joint significance of the two pathways (BMI → SEPA; SEPA → smoking initiation) with 5,000 samples (Preacher & Hayes, 2008). The results from these analyses may be interpreted as the product of standardized estimates for the relationship between BMI and SEPA (a-path; linear) and between SEPA and smoking initiation (b-path; logit).
Figure 2.
Discrete-time survival model with SEPA mediating the effect of BMI on subsequent smoking initiation.
Note. BMI = body mass index percentile based on youth of the same age and sex from self-reported height and weight; SEPA: self-esteem for physical appearance. Model focused on mediation by T2 and T3 SEPA, of the effect of earlier BMI on subsequent initiation. Bootstrapped joint significance tests examined whether the product of the a-path (here: T1 BMI on T2 SEPA, and T3 BMI on T4 SEPA) and the b-path (here: T2 SEPA and T3 initiation, and T4 SEPA and T4 initiation) was significant. *p < .05, **p < .01, ***p < .001.
aSignificant mediator.
In outcome analyses, missing data were handled through Full Information Maximum Likelihood (FIML) under assumption of missing at random, conditional on covariates included in the model, with robust standard errors. One participant was excluded from outcome analyses, because of having missing data for all endogenous variables (resulting N = 932). In cross-sectional analyses, parent reported receipt of lunch subsidy was missing for 125 participants and was also handled through FIML. Using this procedure, we retain the entire person (dataset row). Only the person’s observed y-scores contribute to model estimation and resulting parameter estimates.
Results
Descriptive Statistics and Correlations
Table I shows the descriptive statistics and correlations between BMI, SEPA, and smoking initiation. As predicted, BMI was significantly negatively associated with SEPA at all time points (r = −.22 to −.32, p < .001). Additionally, at all time points, smoking initiation was positively associated with BMI (r = .08 to .15, p < .05) and negatively associated with SEPA (r = −.11 to −.20, p < .01).
Concurrent Associations With T1 Smoking Initiation
Table II shows that T1 BMI’s unadjusted effect on T1 smoking initiation was significant, indicating that for each SD increase in percentile BMI, the odds of having initiated cigarette smoking increased by 34% (p = .02). Adjusting for shared variance with relevant sociodemographic variables (i.e., gender, age, race, and subsidized lunch), the concurrent association between BMI and smoking initiation was no longer significant.
Table II.
Prediction of Concurrent Smoking Initiation Status at Baseline (N = 1,023)
| Smoking initiation (T1) |
|||
|---|---|---|---|
| OR | 95% CI | p | |
| Unadjusted: | |||
| BMI (T1) | 1.34 | [1.05, 1.71] | .02 |
| Adjusted: | |||
| BMI (T1) | 1.24 | [0.97, 1.59] | .09 |
| Non-White (%) | 0.75 | [0.43, 1.31] | .32 |
| Received lunch subsidy (%) | 2.25 | [1.70, 2.98] | <.001 |
| Age (T1) | 2.26 | [1.75, 2.92] | <.001 |
| Gender | 0.96 | [0.60, 1.54] | .88 |
Note. BMI = body mass index percentile based on youth of the same age and sex from self-reported height and weight; CI = confidence interval; OR = odds ratio; T = time point in study.
Prospective Associations With Smoking Initiation
Wald tests of variance over time showed that the models assuming a time-invariant effect of BMI on odds of smoking initiation had better fit to the data compared with those where BMI effects were estimated independently, Wald χ2(3) = 2.86, p = .41. Results from models that assumed a time-invariant effect of lagged BMI showed that BMI significantly predicted subsequent smoking initiation, even when controlling for gender, age, race, and subsidized lunch (see Table III, top panel).
Table III.
Prediction of Prospective Smoking Initiation Among Smoking-Naïve (n = 932)
| Smoking initiation |
|||
|---|---|---|---|
| HR | 95% CI | p | |
| BMI predicting subsequent smoking initiation | |||
| BMI (lagged) | 1.23 | [1.01, 1.49] | .04 |
| Non-White (%) | 0.92 | [0.57, 1.50] | .75 |
| Received lunch subsidy (%) | 1.56 | [1.26, 1.94] | <.001 |
| Age (T1) | 1.36 | [1.11, 1.66] | .003 |
| Gender | 0.79 | [0.54, 1.14] | .20 |
| Mediational model: BMI and SEPA predicting smoking initiation | |||
| BMI (lagged) | 1.17 | [0.96, 1.43] | .12 |
| SEPA (lagged) | 0.75 | [0.59, 0.94] | .014 |
| Non-White (%) | 0.96 | [0.59, 1.55] | .86 |
| Received lunch subsidy (%) | 1.55 | [1.25, 1.92] | <.001 |
| Age (T1) | 1.34 | [1.09, 1.64] | .005 |
| Gender | 0.88 | [0.60, 1.29] | .51 |
Note. BMI = body mass index percentile based on youth of the same age and sex from self-reported height and weight; CI = confidence interval; HR = hazard ratio; SEPA: self-esteem for physical appearance; T = time point in study.
In the mediation model testing Hypothesis 4, when controlling for SEPA, BMI no longer significantly predicted smoking initiation (see Table III, bottom panel), suggesting SEPA may contribute to this relationship. Results from joint significance tests indicated that the mediation of the effect of BMI on smoking initiation by SEPA was significant at T5 (B =.07, 95% confidence interval [CI] [0.01, 0.21]), but not at T3 (B =.03, 95% CI [−0.02, 0.15]).
Discussion
This study aimed to investigate concurrent and prospective relationships between excess weight, SEPA, and initiation of smoking. We found evidence for prospective associations between BMI, low SEPA, and subsequent smoking initiation. This is the first study, to our knowledge, that has examined SEPA as a possible pathway of increased risk for smoking among adolescents with higher levels of adiposity. The results suggested that having lower self-esteem related to one’s physical appearance was associated with a greater likelihood of initiating cigarette smoking in subsequent years and indicated that SEPA may help explain the relationship between higher BMI and increased likelihood of smoking initiation, particularly at the later time point. Thus, youth with overweight and obesity may develop low SEPA and become involved with smoking subsequently.
Youth with overweight or obesity who feel particularly bad about their appearance (e.g., wish their body, weight, or physical appearance were different; perceive themselves as not good looking) may be the ones especially vulnerable to experimentation with cigarettes. Low SEPA may contribute to increased likelihood of trying cigarettes via a number of risk pathways in this population. First, adolescents who have overweight or obesity and low SEPA may try cigarettes as a means of weight control. Consistent with this, adolescent females who describe themselves as overweight and who report trying to lose weight are more likely to initiate smoking (Boles & Johnson, 2001; Cawley, Markowitz, & Tauras, 2004; French, Perry, Leon, & Fulkerson, 1994). Likewise, adolescents who endorsed motivation to smoke for weight control purposes had an increased risk of initiating smoking in the subsequent year (Harakeh, Engels, Monshouwer, & Hanssen, 2010). Among adolescents with overweight/obesity who have low SEPA, initiation of smoking may occur because of a desire to lose weight and a belief that smoking may help them do so.
Another possibility is that increased use of tobacco and other substances may be used as a way to cope with negative emotions created by experiences of rejection or depression (Leary, Schreindorfer, & Haupt, 1995). There is considerable evidence that youth perceive their peers with overweight and obesity with negative attitudes (e.g., perceived as ugly, stupid, and lazy) and that these attitudes develop as early as preschool and can lead to rejection (Puhl & Latner, 2007). In addition, bullying based on weight is more prevalent in youth than bullying based on race/ethnicity, sexual orientation, and religion (Puhl et al., 2016), and risk of smoking initiation is higher among adolescents who have been a victim of bullying (Weiss, Mouttapa, Cen, Johnson, & Unger, 2011). While SEPA was not assessed, among younger children (age: 9–10 years) with obesity who reported decreases in global self-esteem (e.g., being less happy with themselves and liking themselves less), higher rates of loneliness were reported, and there was increased likelihood of smoking (Strauss, 2000).
Equally possible, overweight/obesity and concomitant low self-esteem among adolescents may lead to associating with peers who smoke. Indeed, peer influence is a key factor contributing to adolescent smoking (Kobus, 2003), and adolescents with obesity may see smoking as a way to fit in or increase acceptance among certain peer groups. This is supported by findings suggesting increased pressure from peers to try cigarettes among youth with obesity (Huang, Lanza, Wright-Volel, & Anglin, 2013). During adolescence, the norms and values of one’s peer group and peer bonding are influential determinants of behavior (Catalano et al., 1996; Hawkins et al., 1986). If smoking is rewarded by creating a basis for friendship and enhancing one’s social network, these may be potent sources of reinforcement, particularly if few alternative sources of reinforcement exist (Akers, Krohn, Lanza-Kaduce, & Radosevich, 1979). Indeed, social network analyses have shown that adolescents’ friendship networks are associated with both obesity (Zhang, de la Haye, Ji, & An, 2018) and smoking (Roberts, Nargiso, Gaitonde, Stanton, & Colby, 2015), with adolescents who smoke having higher percentages of peers who smoke in their network and greater frequency of contact with smokers.
Strengths and Limitations
This study had numerous strengths including using a large sample and longitudinal data collection with the ability to rule out bidirectional associations and capture initiation of use during a critical period of adolescence. Nonetheless, the rates of smoking initiation in this sample were low, with less than a quarter of the sample reporting initiation by the T6 assessment. Therefore, it is possible that there was not adequate statistical power to detect associations, particularly at T1 when only a small percentage of the sample had experimented with smoking. This may be in part because of the younger age of the sample; findings may differ for youth who begin experimenting with cigarette smoking at an older age.
Our sample was drawn from a set of schools in a single geographic region, and there was a low rate of participation, which may limit generalizability. Because we had low rates of return of the parental consent forms, enrollment rate was lower than anticipated; we expect this is likely because of the intensive study design, the depersonalized contact through mailed/distributed flyers, and the focus on the sensitive topic of underage drinking. While studies with implicit/passive parental consent tend to yield higher rates of participation, when active parental consent is required in youth substance use or obesity research, participation tends to be lower with rates from 26% to 55% reported (Pokorny, Jason, Schoeny, Townsend, & Curie, 2001; Rojas, Sherrit, Harris, & Knight, 2008; Mellor, Rapoport, & Maliniak, 2008). As concluded by Frissell et al. (2004) parental nonresponse to traditional active consent procedures may reflect failure of parents to attend to the request (e.g., because of inconvenience) as opposed to explicit refusal. Because active consent requires more effort on the part of parents (Liu, Cox, Washburn, Croff, & Crethar, 2017), it is possible that this impacted the characteristics of those who enrolled. While our sample was more racially diverse and less socioeconomically disadvantaged than the school populations from which it was drawn, these demographic variables were included as covariates to account for the influence of these variables in the models.2 The fact that rates of any cigarette use (at least a puff or two) in our sample appear comparable to those of the state of Rhode Island, which is low relative to the United States at large (data not shown), further reduces concerns regarding potential sampling bias. Nonetheless, although findings are innovative and important for understanding SEPA as a potential risk pathway for smoking among adolescents with higher levels of adiposity, it is important to bear in mind that the present sample precludes generalizability of our findings to adolescents at large.
While the models used estimated parameters based on available data to retain all participants in model estimations and reduce the influence of missing data, differential dropout related to demographic characteristics may have influenced findings. Although results of the Monitoring the Future study (Johnston, O’Malley, Bachman, Schulenberg, & Miech, 2016) suggest comparable rates of cigarette smoking among 8th graders based on race/ethnicity and gender, lower SES was associated with increased smoking. Greater rates of SES-related dropout in the current study led to greater need for data estimation for these adolescents. In addition, because of the Web-based nature of the surveys, adolescent weight was self-reported rather than measured. Although a review found robust associations between the two methods among adolescents (r = .84 to .98, Sherry, Jefferds, & Grummer-Strawn, 2007), females underestimated their weight more than males, as did adolescents who were overweight relative to and those who were not. The potential for differential bias in self-report is a limitation of the current study. Finally, while SEPA and BMI were significantly associated at all time points, physical attributes other than adiposity (e.g., hair, complexion, and height) likely also contributed to negative perceptions regarding physical appearance.
Though we would have liked to investigate whether gender moderated the mediation effect, the low base rates of smoking initiation in the current sample left us unable to perform a reliable test of moderated mediation.3 It is important to note that the current study assessed whether higher BMI and lower SEPA made an individual more likely to initiate smoking, not to become a daily smoker. While a recent meta-analysis suggested that more than two-thirds of individuals who initially experiment with smoking will progress to daily smoking, at least temporarily (Birge, Duffy, Miler, & Hajek, 2018), few adolescents in our sample progressed to regular smoking within the time frame of our study, precluding our ability to test risk trajectory further. Similarly, as smoking motives were not assessed in the current study, it was not possible to assess putative mechanistic relationships between low self-esteem and initiation of smoking such as weight or affect management or peer-group norms. Future research should explore the motives and psychosocial context of smoking initiation among adolescents with overweight/obesity further (e.g., with whom they first try smoking and perceived benefits of smoking). Understanding the protective factors that may buffer against low self-esteem among youth with overweight/obesity and may reduce the likelihood of initiating smoking is an important future direction.
Conclusions and Clinical Implications
The findings of the current study indicate that adolescents with overweight/obesity may be at increased risk for experimentation with cigarettes, even after controlling for important sociodemographic factors. It suggests that youth with excess weight are more likely to have low self-esteem regarding their appearance and bodies, and this negative perception may result in experimentation with cigarettes. Adolescents with overweight/obesity who begin smoking have disproportionate risk for negative health consequences because of the individual and interactive risks associated with both excess weight and smoking. Accordingly, understanding how the societal messages are received by youth with overweight/obesity (e.g., from the media, obesity prevention campaigns, physicians, parents, teachers, and peers) may be crucial to understanding the development of low self-esteem in this population and the cascade of future risks that may result. Recently, the American Psychological Association released Clinical Practice Guideline for Multicomponent Behavioral Treatment of Obesity and Overweight in Children and Adolescent (American Psychological Association, 2018). The guideline notes it is important to consider how weight-related messages may impact an adolescent’s self-esteem and a family’s willingness to engage in treatment. Parents and health-care providers have been identified as significant sources of weight-related stigma (Puhl & King, 2013; Puhl & Latner, 2007).
Based on the current findings, we suggest several possible implications. First, health-care providers are encouraged to discuss weight status with patients and parents and to recommend interventions for youth with overweight or obesity to reduce associated health consequences in a way that is not stigmatizing or judgmental (e.g., using neutral words in conversation and documentation) to avoid causing reductions in SEPA. Family-based interventions that include active participation of parents and children for increasing healthy eating and physical activity are recommended in the guideline. These types of interventions may have the additional benefit of increasing the opportunity for bonding within the family and offering alternative sources of rewards to the adolescent, which is recommended as a way to prevent use of tobacco and other substances according to the social development model (Catalano et al., 1996; Hawkins et al., 1986) and, therefore, could help reduce the likelihoood of smoking initiation or progression. Although the guideline does not discuss smoking risk, based on current findings, when working with youth with overweight or obesity, special emphasis should be placed on identifying youth who may be at-risk for smoking. We suggest use of screening measures that assess cognitive susceptibility to smoking (Jackson, 1998; Pierce, Choi, Gilpin, Farkas, & Merritt, 1996; Unger, Johnson, Stoddard, Nezami, & Chou, 1997), smoking initiation, and internalization of weight bias (Ciupitu-Plath, Wiegand, & Babitsch, 2018).
Along with screening, there are opportunities for primary and secondary prevention efforts. For example, providers can help to denormalize the use of tobacco and nicotine or discuss alternate ways to obtain the perceived benefits from smoking (e.g., weight control, social facilitation, and affect regulation) with their patients. When working with youth who have already experimented with cigarettes, “prevescalation” (prevent escalation) strategies that involve reinforcing positive self-perceptions and aspirations that are incompatible with smoking or promoting the use of self-affirmations may help reduce the risk of continuation of smoking (Villanti, Niaura, Abrams, & Mermelstein, 2018). Testing the efficacy of these strategies among youth with overweight or obesity and low SEPA is an important future direction.
Footnotes
We investigated possible nested effects of school cohort in concurrent and prospective analyses. School cohort (defined as five-level categorical predictors with the first school cohort as reference group) did not significantly influence model results, Wald χ2(4, N = 1,023) = 8.975, p = .062; Wald χ2(4, N = 889) = 5.775, p = .217. In our prior work, we have tested for clustering by school cohort and failed to find any clustering effects; we have also failed to find any effects for school cohort (dummy coded) in the prediction of smoking outcomes (as in Lechner et al., 2018; Marceau, Abar, & Jackson, 2015). As such, we chose to report a more parsimonious model that did not account for the nested structure of the data.
To examine whether our processes varied across race and SES, we conducted ancillary analyses in which we calculated a correlation matrix of model constructs and compared correlations across groups defined by these factors. The magnitude and direction of correlations among BMI and SEPA were similar among White and non-White youth and among youth with no lunch subsidy and reduced-price/free lunch. The direction of correlations among BMI and SEPA with smoking initiation was also similar, albeit of much lower magnitude, given low rates of smoking initiation and fewer participants with these characteristics.
We note, however, that the magnitude and direction of correlations among BMI, SEPA, and smoking were similar for boys and girls (Table 1).
Funding
This work was supported by grants from the National Institute on Drug Abuse (grant numbers T32DA016184 and L30DA042415); the National Institute on Alcohol Abuse and Alcoholism (grant numbers R01AA016838, K02AA13938, and T32AA007459).
Conflicts of interest: None declared.
References
- American Psychological Association, Guideline Development Panel for Obesity Treatment. (2018). Clinical practice guideline for multicomponent behavioral treatment of obesity and overweight in children and adolescents: Current state of the evidence and research needs. Retrived from http://www.apa.org/about/offices/directorates/guidelines/obesity-clinical-practice-guideline.pdf [Google Scholar]
- Akers R. L., Krohn M. D., Lanza-Kaduce L., Radosevich M. (1979). Social learning and deviant behavior: a specific test of a general theory. American Sociological Review, 44, 636–655. [PubMed] [Google Scholar]
- Barlow A., Woods S. E. (2009). Relationships between self‐esteem and smoking experimentation in childhood. Early Child Development and Care, 179, 529–537. [Google Scholar]
- Birge M., Duffy S., Miler J. A., Hajek P. (2018). What proportion of people who try one cigarette become daily smokers? A meta analysis of representative surveys. Nicotine and Tobacco Research, 20, 1427–1433. doi: 10.1093/ntr/ntx243. [DOI] [PubMed] [Google Scholar]
- Boles S. M., Johnson P. B. (2001). Gender, weight concerns, and adolescent smoking. Journal of Addictive Diseases, 20, 5–14. [DOI] [PubMed] [Google Scholar]
- Buchmann A. F., Blomeyer D., Jennen‐Steinmetz C., Schmidt M. H., Esser G., Banaschewski T., Laucht M. (2013). Early smoking onset may promise initial pleasurable sensations and later addiction. Addiction Biology, 18, 947–954. [DOI] [PubMed] [Google Scholar]
- Catalano R. F., Kosterman R., Hawkins J. D., Newcomb M. D., Abbott R. D. (1996). Modeling the etiology of adolescent substance use: A test of the social development model. Journal of Drug Issues, 26, 429–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawley J., Markowitz S., Tauras J. (2004). Lighting up and slimming down: the effects of body weight and cigarette prices on adolescent smoking initiation. Journal of Health Economics, 23, 293–311. doi: 10.1016/j.jhealeco.2003.12.003 [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2015). Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health. HHS Publication No. SMA 15-4927. Retrieved from http://www.samhsa.gov/data/ [Google Scholar]
- Centers for Disease Control and Prevention. (2015). About child & teen BMI. Retrieved from www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html [Google Scholar]
- Choi W. S., Gilpin E. A., Farkas A. J., Pierce J. P. (2001). Determining the probability of future smoking among adolescents. Addiction, 96, 313–323. [DOI] [PubMed] [Google Scholar]
- Ciupitu-Plath C., Wiegand S., Babitsch B. (2018). The weight bias internalization scale for youth: validation of a specific tool for assessing internalized weight bias among treatment-seeking german adolescents with overweight. Journal of Pediatric Psychology, 43, 40–51. [DOI] [PubMed] [Google Scholar]
- Danielsen Y. S., Stormark K. M., Nordhus I. H., Mæhle M., Sand L., Ekornås B., Pallesen S. (2012). Factors associated with low self-esteem in children with overweight. Obesity Facts, 5, 722–733. [DOI] [PubMed] [Google Scholar]
- Dolcini M. M., Adler N. E. (1994). Perceived competencies, peer group affiliation, and risk behavior among early adolescents. Health Psychology, 13, 496–506. [DOI] [PubMed] [Google Scholar]
- Fagerström K. (2002). The epidemiology of smoking. Drugs, 62, 1–9. [DOI] [PubMed] [Google Scholar]
- Farhat T., Iannotti R. J., Simons-Morton B. G. (2010). Overweight, obesity, youth, and health-risk behaviors. American Journal of Preventive Medicine, 38, 258–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox C. L., Farrow C. V. (2009). Global and physical self-esteem and body dissatisfaction as mediators of the relationship between weight status and being a victim of bullying. Journal of Adolescence, 32, 1287–1301. [DOI] [PubMed] [Google Scholar]
- Franklin J., Denyer G., Steinbeck K. S., Caterson I. D., Hill A. J. (2006). Obesity and risk of low self-esteem: a statewide survey of Australian children. Pediatrics, 118, 2481–2487. [DOI] [PubMed] [Google Scholar]
- French S. A., Perry C. L., Leon G. R., Fulkerson J. A. (1994). Weight concerns, dieting behavior, and smoking initiation among adolescents: a prospective study. American Journal of Public Health, 84, 1818–1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frissell K. C., McCarthy D. M., D’Amico E. J., Metrik J., Ellingstad T. P., Brown S. A. (2004). Impact of consent procedures on reported levels of adolescent alcohol use. Psychology of Addictive Behaviors, 18, 307–315. [DOI] [PubMed] [Google Scholar]
- Griffiths L. J., Parsons T. J., Hill A. J. (2010). Self‐esteem and quality of life in obese children and adolescents: A systematic review. Pediatric Obesity, 5, 282–304. [DOI] [PubMed] [Google Scholar]
- Harakeh Z., Engels R. C., Monshouwer K., Hanssen P. F. (2010). Adolescent’s weight concerns and the onset of smoking. Substance Use and Misuse, 45, 1847–1860. [DOI] [PubMed] [Google Scholar]
- Harter S. (1985). Manual for the self-perception profile for children:Revision of the perceived competence scale for children. Denver, CO: University of Denver. [Google Scholar]
- Harter S. (1993). Causes and consequences of low self-esteem in children and adolescents self-esteem (pp. 87–116): Springer. [Google Scholar]
- Harter S. (2012). Self-perception profile for adolescents: Manual and questionnaires. Denver, CO: University of Denver. [Google Scholar]
- Hawkins J. D., Lishner D. M., Catalano R. F. Jr, Howard M. O. (1986). Childhood predictors of adolescent substance abuse: toward an empirically grounded theory. Journal of Children in Contemporary Society, 18, 11–48. [Google Scholar]
- Hu M.-C., Davies M., Kandel D. B. (2006). Epidemiology and correlates of daily smoking and nicotine dependence among young adults in the United States. American Journal of Public Health, 96, 299–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang D. Y., Lanza H. I., Wright-Volel K., Anglin M. D. (2013). Developmental trajectories of childhood obesity and risk behaviors in adolescence. Journal of Adolescence, 36, 139–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huxley R. R., Yatsuya H., Lutsey P. L., Woodward M., Alonso A., Folsom A. R. (2012). Impact of age at smoking initiation, dosage, and time since quitting on cardiovascular disease in African Americans and whites: The atherosclerosis risk in communities study. American Journal of Epidemiology, 175, 816–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson C. (1998). Cognitive susceptibility to smoking and initiation of smoking during childhood: A longitudinal study. Preventive Medicine, 27, 129–134. [DOI] [PubMed] [Google Scholar]
- Jackson K. M., Barnett N. P., Colby S. M., Rogers M. (2015). The prospective association between sipping alcohol by the sixth grade and later substance use. Journal of Studies on Alcohol and Drugs, 76, 212–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson K. M., Colby S. M., Barnett N. P., Abar C. C. (2015). Prevalence and correlates of sipping alcohol in a prospective middle school sample. Psychology of Addictive Behaviors, 29, 766–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston L. D., O’Malley P. M., Bachman J. G., Schulenberg J. E., Miech R. (2016). Monitoring the Future national survey results on drug use, 1975-2015: Volume II, college students and adults ages 19-55. Ann Arbor, MI: Institute for Social Research, The University of Michigan [Google Scholar]
- Kann L. (2016). Youth risk behavior surveillance—United States, 2015. MMWR Surveillance Summaries, 65. [DOI] [PubMed] [Google Scholar]
- Kobus K. (2003). Peers and adolescent smoking. Addiction, 98, 37–55. [DOI] [PubMed] [Google Scholar]
- Lange K., Thamotharan S., Racine M., Hirko C., Fields S. (2015). The relationship between weight and smoking in a national sample of adolescents: role of gender. Journal of Health Psychology, 20, 1558–1567. [DOI] [PubMed] [Google Scholar]
- Leary M. R., Schreindorfer L. S., Haupt A. L. (1995). The role of low self-esteem in emotional and behavioral problems: why is low self-esteem dysfunctional?. Journal of Social and Clinical Psychology, 14, 297–314. [Google Scholar]
- Lechner W. V., Murphy C. M., Colby S. M., Janssen T., Rogers M. L., Jackson K. M. (2018). Cognitive risk factors of electronic and combustible cigarette use in adolescents. Addictive Behaviors, 82, 182–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lifrak P. D., McKay J. R., Rostain A., Alterman A. I., O’brien C. P. (1997). Relationship of perceived competencies, perceived social support, and gender to substance use in young adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 933–940. [DOI] [PubMed] [Google Scholar]
- Liu C., Cox R. B. Jr, Washburn I. J., Croff J. M., Crethar H. C. (2017). The effects of requiring parental consent for research on adolescents’ risk behaviors: A meta-analysis. Journal of Adolescent Health, 61, 45–52. [DOI] [PubMed] [Google Scholar]
- Marceau K., Abar C. C., Jackson K. M. (2015). Parental knowledge is a contextual amplifier of associations of pubertal maturation and substance use. Journal of Youth and Adolescence, 44, 1720–1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellor J. M., Rapoport R. B., Maliniak D. (2008). The impact of child obesity on active parental consent in school-based survey research on healthy eating and physical activity. Evaluation Review, 32, 298–312. [DOI] [PubMed] [Google Scholar]
- Minagawa K., While D., Charlton A. (1993). Smoking and self-perception in secondary school students. Tobacco Control, 2, 215. [Google Scholar]
- Muthen L. K., Muthen B. O. (2007). Mplus: statistical analysis with latent variables In MPlus User’s Guide (4th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Ng M., Fleming T., Robinson M., Thomson B., Graetz N., Margono C., Mullany E. C., Biryukov S., Abbafati C., Abera S. F., Abraham J. P., Abu-Rmeileh N. M., Achoki T., AlBuhairan F. S., Alemu Z. A., Alfonso R., Ali M. K., Ali R., Guzman N. A., Ammar W., Anwari P., Banerjee A., Barquera S., Basu S., Bennett D. A., Bhutta Z., Blore J., Cabral N., Nonato I. C., Chang J. C., Chowdhury R., Courville K. J., Criqui M. H., Cundiff D. K., Dabhadkar K. C., Dandona L., Davis A., Dayama A., Dharmaratne S. D., Ding E. L., Durrani A. M., Esteghamati A., Farzadfar F., Fay D. F., Feigin V. L., Moschandreas J., Naghavi M., Naheed A., Nand D., Narayan K. M., Nelson E. L., Neuhouser M. L., Nisar M. I., Ohkubo T., Oti S. O., Pedroza A., Prabhakaran D., Roy N., Sampson U., Seo H., Sepanlou S. G., Shibuya K., Shiri R., Shiue I., Singh G. M., Singh J. A., Skirbekk V., Stapelberg N. J., Sturua L., Weiderpass E., Werdecker A., Wright J. L., Yang Y. C., Yatsuya H., Yoon J., Yoon S. J., Zhao Y., Zhou M., Zhu S., Lopez A. D., Murray C. J., Gakidou E. (2014). Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. The Lancet, 384, 766–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce J. P., Choi W. S., Gilpin E. A., Farkas A. J., Merritt R. K. (1996). Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychology, 15, 355–361. [DOI] [PubMed] [Google Scholar]
- Pokorny S. B., Jason L. A., Schoeny M. E., Townsend S. M., Curie C. J. (2001). Do participation rates change when active consent procedures replace passive consent. Evaluation Review, 25, 567–580. [DOI] [PubMed] [Google Scholar]
- Preacher K. J., Hayes A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. [DOI] [PubMed] [Google Scholar]
- Puhl R. M., King K. M. (2013). Weight discrimination and bullying. Best Practice and Research Clinical Endocrinology and Metabolism, 27, 117–127. [DOI] [PubMed] [Google Scholar]
- Puhl R. M., Latner J., O’brien K., Luedicke J., Forhan M., Danielsdottir S. (2016). Cross‐national perspectives about weight‐based bullying in youth: Nature, extent and remedies. Pediatric Obesity, 11, 241–250. [DOI] [PubMed] [Google Scholar]
- Puhl R. M., Latner J. D. (2007). Stigma, obesity, and the health of the nation’s children. Psychological Bulletin, 133, 557.. [DOI] [PubMed] [Google Scholar]
- Ratcliff M. B., Jenkins T. M., Reiter-Purtill J., Noll J. G., Zeller M. H. (2011). Risk-taking behaviors of adolescents with extreme obesity: Normative or not? Pediatrics, 127, 827–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts M. E., Nargiso J. E., Gaitonde L. B., Stanton C. A., Colby S. M. (2015). Adolescent social networks: general and smoking-specific characteristics associated with smoking. Journal of Studies on Alcohol and Drugs, 76, 247–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rojas N. L., Sherrit L., Harris S., Knight J. R. (2008). The role of parental consent in adolescent substance use research. Journal of Adolescent Health, 42, 192–197. [DOI] [PubMed] [Google Scholar]
- Seo D. C., Jiang N., Kolbe L. J. (2009). Association of smoking with body weight in US high school students, 1999-2005. American Journal of Health Behavior, 33, 202–212. [DOI] [PubMed] [Google Scholar]
- Sherry B., Jefferds M. E., Grummer-Strawn L. M. (2007). Accuracy of adolescent self-report of height and weight in assessing overweight status: a literature review. American Journal of Health Behavior, 161, 1154–1161. [DOI] [PubMed] [Google Scholar]
- Singer J. D., Willett J. B. (2003). Applied longitudinal data analysis: Modeling change and event occurrence. Oxford University Press. [Google Scholar]
- Strauss R. S. (2000). Childhood obesity and self-esteem. Pediatrics, 105, e15.. [DOI] [PubMed] [Google Scholar]
- Unger J. B., Johnson C. A., Stoddard J. L., Nezami E., Chou C. P. (1997). Identification of adolescents at risk for smoking initiation: validation of a measure of susceptibility. Addictive Behaviors, 22, 81–91. [DOI] [PubMed] [Google Scholar]
- Villanti A. C., Niaura R. S., Abrams D. B., Mermelstein R. (2018). Preventing smoking progression in young adults: The concept of prevescalation. Prevention Science, in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss J. W., Mouttapa M., Cen S., Johnson C. A., Unger J. (2011). Longitudinal effects of hostility, depression, and bullying on adolescent smoking initiation. Journal of Adolescent Health, 48, 591–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wichstraum L. (1995). Harter’s Self-Perception Profile for Adolescents: reliability, validity, and evaluation of the question format. Journal of Personality Assessment, 65, 100–116. [DOI] [PubMed] [Google Scholar]
- Wills T. A., Sandy J. M., Yaeger A. M., Cleary S. D., Shinar O. (2001). Coping dimensions, life stress, and adolescent substance use: a latent growth analysis. J Abnorm Psychol, 110, 309.. [DOI] [PubMed] [Google Scholar]
- Zhang S. K., de la Haye K., Ji M., An R. (2018). Applications of social network analysis to obesity: a systematic review. Obesity Reviews, 19, 976–988. [DOI] [PubMed] [Google Scholar]