Abstract
Background
Cancer is the leading cause of death in the developed world, and yet healthcare practitioners infrequently discuss goals of care (GoC) with hospitalized cancer patients. We sought to identify barriers to GoC discussions from the perspectives of staff oncologists, oncology residents, and oncology nurses.
Methods
This was a single center survey of staff oncologists, oncology residents, and inpatient oncology nurses. Barriers to GoC discussions were assessed on a 7-point Likert scale (1 = extremely unimportant; 7 = extremely important).
Results
Between July 2013 and May 2014, of 185 eligible oncology clinicians, 30 staff oncologists, 10 oncology residents, and 28 oncology nurses returned surveys (response rate of 37%). The most important barriers to GoC discussions were patient and family factors. They included family members’ difficulty accepting poor prognoses (mean score 5.9, 95% CI [5.7, 6.2]), lack of family agreement in the goals of care (mean score 5.8, 95% CI [5.5, 6.1]), difficulty understanding the limitations of life-sustaining treatments (mean score 5.8, 95% CI [5.6, 6.1]), lack of patients’ capacity to make goals of care decisions (mean score 5.7, 95% CI [5.5, 6.0]), and language barriers (mean score 5.7, 95% CI [5.4, 5.9]). Participants viewed system factors and healthcare provider factors as less important barriers.
Conclusions
Oncology practitioners perceive patient and family factors as the most limiting barriers to GoC discussions. Our findings underscore the need for oncology clinicians to be equipped with strong communication skills to help patients and families navigate GoC discussions.
Electronic supplementary material
The online version of this article (10.1186/s12885-019-5333-x) contains supplementary material, which is available to authorized users.
Keywords: Goals of care discussions, End of life, Barriers, Cancer care
Background
Cancer is a leading cause of mortality in the developed world [1]. Most terminally-ill cancer patients prefer to die at home [2]. Despite this, approximately one third still die in hospital, and nearly 10 % die in the intensive care unit (ICU) [3]. An estimated 30 % of patients offered chemotherapy are in the last months of life, and this percentage is increasing each year, as are emergency room (ER) visits, hospitalizations, and admissions to the ICU [4–8]. Physicians often lack awareness of their patients’ wishes to avoid resuscitation in hospital [9]. Unwanted aggressive care at the end of life (EOL) is associated with increased healthcare costs, worse quality of life, and a worse death [10].
Decision-making about goals of care (GoC) has been defined as a communication process that occurs between clinicians and a patient to establish a care plan, and includes decisions about the use or non-use of life-sustaining treatments [11]. Less than a third of patients with advanced cancer have had a GoC discussion with a member of care team [10, 12]. As a result, patients may be subject to unwanted aggressive treatments near the end of life. Cancer patients who die in hospital experience more pain, anxiety, and physical and emotional distress compared to those who die at home with hospice services [13, 14]. Furthermore, when patients die in the ICU or in hospital, family members and caregivers are at higher risk for both post-traumatic stress disorder and prolonged grief disorder [15, 16]. In contrast, patients who have a more accurate understanding of their prognosis are more likely to decline aggressive interventions and resuscitation at the EOL [15]. GoC discussions between patients and physicians are associated with fewer life-sustaining interventions, fewer ICU admissions, better patient outcomes [14], and lower healthcare costs [17].
Hospitalization of a patient with advanced cancer marks an important inflection point in their illness trajectory and presents an important opportunity to clarify GoC. While the importance of support and communication around end-of-life decision-making in advanced cancer has been recognized [18], relatively few studies have identified the relative importance of barriers to GoC discussions in the oncology population. Previous studies have attempted to explore barriers experienced by physicians such as personal discomfort with death and dying [19, 20]. An improved understanding of the barriers to GoC discussions with hospitalized patients who have advanced cancer will inform the design of future strategies aimed at improving both the quantity and quality of GoC discussions in this patient population. The aim of this study was to identify barriers to GoC discussions with hospitalized patients who have advanced cancer, as perceived by oncology clinicians.
Methods
We conducted a cross-sectional survey on all oncology wards of the Juravinski Hospital and Cancer Centre in Hamilton, Ontario, between July 2013 and May 2014. We defined oncology inpatient wards as a unit where staff oncologists, oncology residents, and nurses provided care for admitted patients with cancer. The Hamilton Integrated Research Ethics Board approved the study. Participants gave implicit informed consent through completion of the self-administered questionnaire in response to an invitation to participate voluntarily.
We surveyed oncology clinicians according to the following inclusion criteria: 1) staff oncologists providing care to cancer inpatients, 2) residents enrolled as a subspecialty trainee in the hematology, radiation, and medical oncology programs at McMaster University, and 3) nurses (registered nurses, advanced practice nurses, licensed practical nurses, or registered practical nurses) employed full time, or part time, on the oncology wards.
Physician-specific (staff oncologist or oncology resident) and nurse-specific versions of the questionnaire were created to capture items specific to each professional group. The questionnaire used in this study was adapted from a questionnaire used previously to quantify barriers to goals of care discussions, as perceived by clinicians, with seriously ill hospitalized patients on medical teaching units [21]. This original questionnaire was drafted by the authors, presented to a national focus group, revised by front-line clinicians, and then pilot-tested with physicians and nurses on a medical teaching unit (MTU) in Hamilton, Ontario, Canada. To adapt the survey for this study, oncologists provided clinical expertise and feedback on the content and structure of the questionnaire, including the hypothetical patient vignettes. We pilot-tested the initial adapted version with the study investigators and made revisions to improve clarity in a final version.
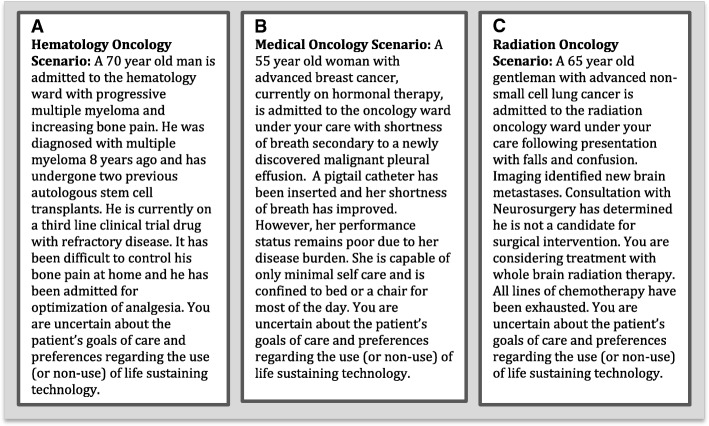
The final questionnaire was then distributed in a paper-based format to oncology clinicians and electronic reminders were given to non-responders [22]. The preamble to the questionnaire presented the definition of goals-of-care discussions to be used for this study: “We define communication and decision-making about goals of care as a conversation in which, ideally, a patient or family member and the healthcare team establish the goals of treatment (e.g., cure, prolongation of life, comfort) and agree upon the types of life sustaining technology that will (or will not) be used to achieve those goals (e.g., CPR, mechanical ventilation, dialysis, intensive care unit admission, feeding tubes, or intravenous hydration)” [11]. Each questionnaire contained a clinical vignette (Fig. 1) that was tailored to each subspecialty of oncology (medical, hematology, radiation). Barriers to GoC discussions were assessed on a 7-point Likert scale (1 = extremely unimportant, 2 = very unimportant, 3 = somewhat unimportant, 4 = neither important nor unimportant, 5 = somewhat important, 6 = very important, 7 = extremely important). Participants were then asked to rate their willingness to participate in different aspects of GoC discussions (initiate discussion, exchange information, act as a decision coach, make a final decision) on the same 7-point Likert scale. Finally, participants were asked to rate how acceptable they found it to have other healthcare professionals initiate and participate in these different aspects of GoC discussions using the same 7-point Likert Scale.
Fig. 1.
Clinical Vignettes. Clinical vignettes for clinicians in: (a) hematology oncology, (b) medical oncology, and (c) radiation oncology
All statistical analyses were performed with the use of SPSS software. We summarized continuous data using means and categorical data using proportions. We report survey responses as means and 95% confidence intervals.
Results
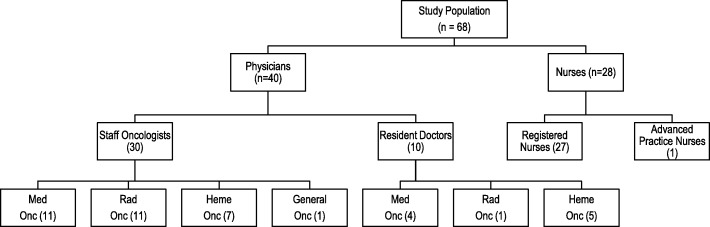
The overall response rate was 68/185 (37%); (30/51 [57%] among staff oncologists, 10/26 [38%] among oncology residents, and 28/108 [26%] among oncology nurses). Figure 2 depicts the professional training of the study respondents, and the demographic characteristics of the study participants are shown in Table 1.
Fig. 2.
Study Population
Table 1.
Characteristics of Respondents
| Nurses (n = 28) | |
|---|---|
| Age (mean) | 40.2 |
| Male | 2 (7%) |
| Female | 26 (93%) |
| Years of practice (mean) | 12.0 |
| Staff Physicians (n = 30) | |
| Age (mean) | 42 |
| Male | 21 (70%) |
| Female | 9 (30%) |
| Years of practice (mean) | 12.5 |
| Resident Physicians (n = 10) | |
| Age (mean) | 31.4 |
| Male | 8 (80%) |
| Female | 2 (20%) |
| Weeks of inpatient subspecialty oncology completed (mean) | 5.9 |
Barriers to goals of care discussions as perceived by oncology clinicians
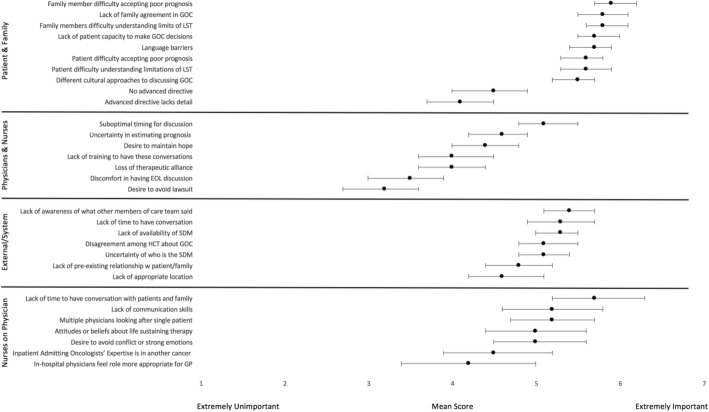
Participants perceived patient and family member factors as the most important barriers to GoC discussions. These included: family members’ difficulty accepting a poor prognosis, lack of family agreement in the goals of care, difficulty understanding the limitations of life-sustaining treatments, lack of patients’ capacity to make goals of care decisions, and language barriers. Study participants viewed system factors and healthcare provider factors as less important barriers. Among external and system factors, lack of time was perceived as one of the more important barriers. Figure 3 illustrates the perceived barriers rated in this study, and all mean scores are tabulated in Additional file 1.
Fig. 3.
Perceived Barriers to Goals of Care Discussions. Combined mean scores from physicians and nurses on a Likert scale, rating the perceived barriers related to patient and family, the role of physicians and nurses from their own perspective, system and external factors, and the role of physicians from nurses’ perspective. The error bars denote 95% confidence intervals
Perceptions of inter-professional roles in communication and decision making about goals of care
Physicians and nurses together expressed a willingness to engage in GoC discussions, including initiating discussions with patients and family, exchanging important information such as diagnosis and prognosis, acting as a decision coach, and making a final decision together with the patient (Additional file 2).
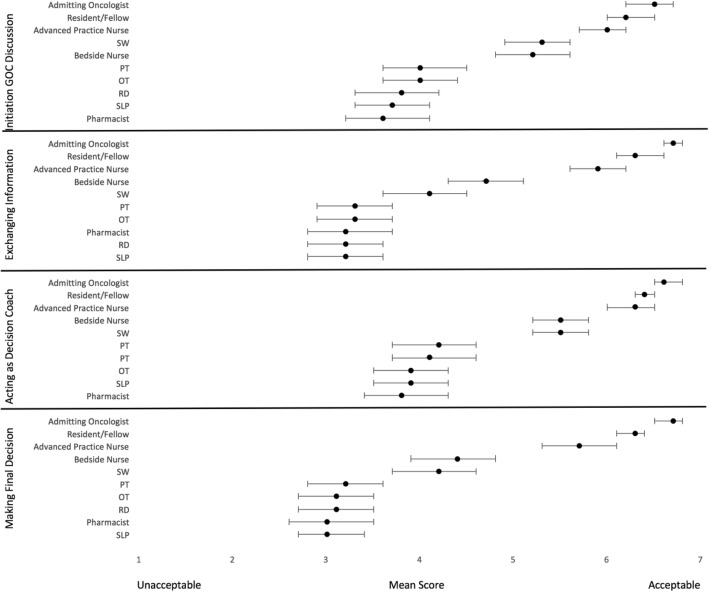
Participants were agreeable to involving allied health professionals in certain aspects of GoC discussions. For initiating a discussion or acting as a decision coach, participants felt that it would be appropriate for many different members of the inter-professional team to be involved, including the admitting oncologist, resident, advanced practice nurse, social worker, or bedside nurse. In contrast, for exchanging pertinent information such as diagnosis or prognosis, or making a final decision together with the patient, study participants felt that the most acceptable individual was the admitting oncologist, followed by the resident, and then advanced practice nurse. Participants felt it was less acceptable for other allied health professionals such as physiotherapists, occupational therapists, registered dieticians, speech language pathologists or pharmacists to engage in these other aspects of GoC discussions (Fig. 4, Additional file 3).
Fig. 4.
Acceptability of Inter-Professional Healthcare Team Members to Engage in Goals of Care Discussions. Combined mean score from physicians and nurses on a Likert scale rating the acceptability of inter-professional healthcare team members in initiating GOC discussion, exchanging information, acting as decision coach, making final decision. The error bars denote 95% confidence intervals
Discussion
In this survey of staff oncologists, oncology residents, and nurses caring for patients with cancer at an academic cancer centre, we found that oncology clinicians perceived patient and family factors as the most important barriers to GoC discussions, and that system and healthcare provider factors were viewed as less important. Study participants also expressed a willingness to engage in many aspects of GoC discussions, such as initiating discussions, exchanging critical information such as prognosis, and making a final decision. Study participants found it acceptable for many different professional groups, including social workers and nurses, to initiate GoC discussions and act as a decision coach.
Cancer patients are more likely to receive care consistent with their preferences when they have had a GoC discussion with their physician, and are more likely to opt for symptom-directed care when they recognize their illness is terminal [23]. While GoC discussions improve the dying experience for patients [24], this study adds to the literature demonstrating that patient and family factors are the biggest barriers to effective GoC discussions as perceived by clinicians [21]. Although study participants rated practitioner factors as less important barriers to GoC, this has several interpretations and implications. First, it reflects that patients who have advanced cancer and their families may often find it difficult to confront a poor prognosis. As a result, oncology clinicians should anticipate that patients and families may find GoC conversations difficult or emotionally laden and be prepared to guide patients and families through these discussions. However patients who have cancer report that physicians are particularly inadequate in discussing emotional symptoms, life support preferences and hospice care, regardless of the patient’s age or disease stage [25]. Indeed, other studies have found that oncology practitioners often lack communication skills training and have discomfort with difficult discussions that include mortality acknowledgement and the introduction of a palliative approach to care [26–29]. This suggests that oncology clinicians may benefit from further training and continuing professional development to enhance their communication skills in order to best support patients and their families in GoC conversations [30]. Patients facing serious illnesses prefer to actively participate in EOL care planning [31–34]. While patient factors are often rated as the most significant barriers to communication, with formal training, oncology clinicians can master communication skills that will empower them to guide patients with advanced cancer through frank discussions about their prognosis and preferences for care at the end of life, preferably early in the course of disease [35, 36]. Formal training would also give clinicians an opportunity to learn and use validated tools for initiating these discussions [37] and develop an approach that recognizes the benefits of these conversations, while helping patients to discuss their values and preferences [19].
Despite many highly-rated barriers to GoC discussions, oncology physicians, residents and nurses described themselves as willing to engage in these important conversations. This likely reflects progressive awareness among providers that many cancer patients have not had GoC discussions, even at the time of admission to hospital, and of those who have, as many as half lack formal documentation of these conversations [9]. There is growing appreciation for both the importance and the timing of GoC discussions, as cancer patients who discuss their GoC with their healthcare team enter hospice care earlier, have fewer critical care admissions, a greater likelihood of dying outside the hospital, and a significantly improved quality of life [14, 38]. Finally, it likely reflects a rising awareness of advanced cancer patients wishing to avoid unwanted life support as a key element of quality end of life care [39].
The findings of this study also emphasized a lack of time as an important barrier, across all categories. Prioritizing protected time for important discussions is of great importance [40]. An acute admission to hospital marks an important change in disease trajectory, but only half of patients with advanced cancer who have documented EOL care discussions with their providers do so in the context of an emergency room visit or inpatient hospitalization [41]. Furthermore, acute care hospitals have performed poorly overall when evaluated on the quality of their end-of-life communication, as measured by validated quality indicators [42]. Ultimately, hospitalizations leave little time for discussion unless it is a priority, and patients may not have the same ability to recognize their hospitalization as a worsening of their prognosis. An admission to acute care often represents an important inflection point in a patient’s illness trajectory and should serve as a potent reminder to oncology clinicians to open the lines of communication and to discuss or revisit goals of care with their patients.
To further support patients and families, many tools and decision aids for patients have been explored, with the intention of helping patients ask questions, understand difficult decisions, and ultimately receive care that is aligned with their values and goals [43]. Question prompt lists have assisted patients and their caregivers to ask questions about end-of-life issues without contributing anxiety or impairing satisfaction [44]. Video decision aids have significantly decreased the likelihood that patients will opt for CPR and resuscitation, and be more certain of their decision-making [45, 46]. More significantly, decision aids have increased the likelihood that their choices ultimately reflect their own values [47]. While these tools are promising, the results of this study bring to light a myriad of barriers perceived by healthcare providers that need to be addressed. While decision aids may be helpful adjuncts, they cannot personalize disclosure of prognosis, and do not take the place of an honest, nuanced, and compassionate interaction between the patient and the clinicians caring for them.
Another implication of this study is the opportunity to include allied health professionals in GoC discussions. Second to physicians, study participants felt advanced practice nurses were most appropriate to engage in GoC discussions. Similarly, bedside nurses and social workers were felt to be acceptable individuals to specifically initiate discussions and act as a decision coach. This is supported by literature, where both nurses and social workers are significantly involved in end of life care, including a willingness to participate in GoC decision-making [48]. Social workers can be integral in information giving and education, as well as helping patients reach final decisions [49]. There is also great initiative and willingness on the part of other allied health members to play an active role [50–52]. These skilled individuals have a unique understanding of a patients’ health status, and concurrently can establish a unique rapport. This study’s findings suggest that there is an opportunity to adopt a more interprofessional approach to having conversations about a patient’s values, preferences, and goals of care.
There are several limitations to this study. It was conducted at a single academic cancer centre, and the respondents, on average, were relatively young or, in the case of oncology residents, had relatively little experience in subspecialty oncology settings. In addition, to the extent that non-responders held different views than our study participants, the 37% response rate in our study may limit the generalizability of our findings. However, our findings were remarkably similar to findings from a multi-center survey of practitioners (response rate 78%) that we conducted on hospital medical wards [21]. Therefore, our study confirms that the findings of our earlier study are generalizable to the oncology setting, suggesting that barriers to goals-of-care discussions during serious illness may be similar regardless of the specific disease state and that disease-agnostic interventions to improve communication during serious illness may be useful. Finally, it is possible that respondents might have been influenced by infrequent but very memorable interactions with advanced cancer patients or their families. Certain challenging interactions are subject to recall bias and as a result, respondents may have placed undue weight on patient and family factors.
Conclusions
Oncology clinicians perceive patient and family factors as the most important barriers to GoC discussions. This insight forms an important platform for future interventions. Our findings highlight the potential for high levels of anxiety or even denial faced by patients with advanced cancer. This underscores the need for oncology clinicians to be equipped with strong communication skills to help patients and their families to navigate GoC decisions. Making time for these crucial conversations and planning to have them throughout the course of illness is imperative. GoC discussions should be initiated by physicians and nurses who have received focused training in this regard, and the discussion would be made richer with the help of skilled allied health professionals.
Additional files
Mean scores from physicians and nurses on a Likert scale, rating barriers related to patient and family factors, the role of physicians and nurses from their own perspective, system and external factors, and the role of physicians from nurses’ perspective. (DOCX 19 kb)
Mean Likert scores, physicians and nurses rating their own willingness to engage in goals of care discussions. (DOCX 50 kb)
Mean scores from physicians and nurses on a Likert scale, rating their perceptions of inter-professional roles in communicating and decision-making around goals of care. (DOCX 91 kb)
Acknowledgements
The authors would like to thank Parveen Wasi, Lindsay Melvin, Ian Mazzetti, Jessica Singh, Jennifer Goy and Sharon Hendershott for their contribution to the development and distribution of this study’s questionnaire.
Presented: The study was reported previously as a poster presentation at the Canadian Society of Internal Medicine Conference in 2015.
Funding
This study did not receive private or public funding.
Availability of data and materials
The study database is available from the authors upon request.
Abbreviations
- EOL
End of Life
- ER
Emergency Room
- GoC
Goals of Care
- ICU
Intensive Care Unit
- MTU
Medical Teaching Unit
Authors’ contributions
All authors have read and approved the manuscript and made the following contributions: KLP: Data analysis, manuscript preparation and critical review of the manuscript. AP (Ameen Patel): conception of the study, critical review of the manuscript. AW: data analysis, critical review of the manuscript. LM: data analysis, critical review of the manuscript. AP (Alexandra Patel): data collection, critical review of the manuscript. MP: data collection, critical review of the manuscript. YL: conception of the study, critical review of the manuscript. BD: conception of the study, critical review of the manuscript. JY: conception of the study, data collection, manuscript preparation and approval.
Ethics approval and consent to participate
This study has full approval from the Hamilton Integrated Research Ethics Board (study reference #11–631). Participant consent was implied by completion of the study questionnaire.
Consent for publication
Not applicable, no individual participant’s data is reported.
Competing interests
All authors have read and approved this manuscript, and declare that this is a work of original intellectual effort. They have no conflicts of interest to disclose. The manuscript is not under consideration for publication by any other journal.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Katrina Lynn Piggott, Phone: 416.864.5015, Email: katrina.piggott@mail.utoronto.ca.
Ameen Patel, Email: patela@mcmaster.ca.
Arthur Wong, Email: arthur.wong@medportal.ca.
Leslie Martin, Email: leslie.martin@medportal.ca.
Alexandra Patel, Email: alexandra.patel@mail.utoronto.ca.
Matthew Patel, Email: matthewpatel@rcsi.ie.
Yudong Liu, Email: yliu2018@dents.uwo.ca.
Sukhbinder Dhesy-Thind, Email: dhesy@hhsc.ca.
John J. You, Email: jyou@mcmaster.ca
References
- 1.Canadian Cancer Society. Right to Care: Palliative Care for All Canadians, 2016 Report. Accessed 19 May 2016. https://www.cancer.ca/~/media/cancer.ca/CW/get%20involved/take%20action/Palliative-care-report-2016-EN.pdf?la=en
- 2.Bruera E, Russell N, Sweeney C, et al. Place of death and its predictors for local patients registered at a comprehensive cancer center. J Clin Oncol. 2002;20:2127–2133. doi: 10.1200/JCO.2002.08.138. [DOI] [PubMed] [Google Scholar]
- 3.Angus DC, Barnato AE, Linde-Zwirble WT, et al. Use of intensive care at the end of life in the United States. Crit Care Med. 2004;32:638–643. doi: 10.1097/01.CCM.0000114816.62331.08. [DOI] [PubMed] [Google Scholar]
- 4.Earle CC, Landrum MB, Souza JM, et al. Aggressiveness of cancer care near the end of life: is it a quality-of-care issue? J Clin Oncol. 2008;26:3860–3866. doi: 10.1200/JCO.2007.15.8253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Emanuel EJ, Young-Xu Y, Levinsky NG, et al. Chemotherapy use among Medicare beneficiaries at the end of life. Ann Intern Med. 2003;138:639–643. doi: 10.7326/0003-4819-138-8-200304150-00011. [DOI] [PubMed] [Google Scholar]
- 6.Temel JS, McCanon J, Greer JA, et al. Aggressiveness of care in a prospective cohort of patients with advanced NSCLC. Cancer. 2008;113:826–833. doi: 10.1002/cncr.23620. [DOI] [PubMed] [Google Scholar]
- 7.Sharma G, Freeman J, Zhang D, et al. Trends in end-of-life ICU use among older adults with advanced lung cancer. Chest. 2008;133:72–78. doi: 10.1378/chest.07-1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Earle C, Neville B, et al. Trends in the aggressiveness of Cancer care near the end of life. J Clin Oncol. 2004;24(2):315–321. doi: 10.1200/JCO.2004.08.136. [DOI] [PubMed] [Google Scholar]
- 9.The SUPPORT Principal Investigators A controlled trial to improve Care for Seriously ill Hospitalized Patients: the study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT)—the SUPPORT principal Investigators. JAMA. 1995;274:1591–1598. doi: 10.1001/jama.1995.03530200027032. [DOI] [PubMed] [Google Scholar]
- 10.Zhang B, Wright A, et al. Health care costs in the last week of life – associations with end-of-life conversations. Arch Intern Med. 2009;169(5):480–488. doi: 10.1001/archinternmed.2008.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sinuff T, Dodek P, You JJ, et al. Improving end-of-life communication and decision making: the development of a conceptual framework and quality indicators. J Pain Symptom Manag. 2015;49(6):107080. doi: 10.1016/j.jpainsymman.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 12.Huskamp HA, Keating NL, Malin JL, et al. Discussions with physicians about hospice among patients with metastatic lung cancer. Arch Intern Med. 2009;169:954–962. doi: 10.1001/archinternmed.2009.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nelson JE, Meier DE, Oei EJ, et al. Self reported symptom experience of critically ill cancer patients receiving intensive care. Crit Care Med. 2001;29(2):277–282. doi: 10.1097/00003246-200102000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Wright A, Keating N, et al. Place of death: correlations with quality of life of patients with Cancer and predictors of bereaved caregivers’ mental health. J Clin Oncol. 2010;28(29):4457–4464. doi: 10.1200/JCO.2009.26.3863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patients’ mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300:1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end-of-life care at the last place of care. JAMA. 2004;291:88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 17.Fries JF, Koop CE, Beadle CE, et al. Reducing health care costs by reducing the need and demand for medical services. N Engl J Med. 1993;329(5):321–325. doi: 10.1056/NEJM199307293290506. [DOI] [PubMed] [Google Scholar]
- 18.The American Society of Clinical Oncology (ASCO) Cancer care during the last phase of life. J Clin Oncol. 1998;16:1986–1996. doi: 10.1200/JCO.1998.16.5.1986. [DOI] [PubMed] [Google Scholar]
- 19.Granek L, Krzyzanowska M, et al. Oncologists’ strategies and barriers to effective communication about the end of life. J Oncol Pract. 2013;9:e129–e135. doi: 10.1200/JOP.2012.000800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mori M, Shimizu C, Ogawa A, et al. A National Survey to systematically identify factors associated with Oncologists' attitudes toward end-of-life discussions: what determines timing of end-of-life discussions? Oncologist. 2015;20(11):1304–11. doi: 10.1634/theoncologist.2015-0147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.You J, Downar J, Fowler R, et al. Barriers to goals of care discussions with seriously ill hospitalized patients and their families: a multicenter survey of clinicians. JAMA Intern Med. 2015;175(4):549–556. doi: 10.1001/jamainternmed.2014.7732. [DOI] [PubMed] [Google Scholar]
- 22.Dillman DA. Mail and Internet surveys: the tailored design method. New York, NY: Wiley; 2000. [Google Scholar]
- 23.Mack JW, Weeks JC, Wright AA, et al. End-of-life discussions, goal attainment, and distress at the end of life: predictors and outcomes of receipt of care consistent with preferences. J Clin Oncol. 2010;28:1203–1208. doi: 10.1200/JCO.2009.25.4672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lorenz KA, Lynn J, Dy SM, et al. Evidence for improving palliative care at the end of life: a systematic review. Ann Intern Med. 2008;148:147–159. doi: 10.7326/0003-4819-148-2-200801150-00010. [DOI] [PubMed] [Google Scholar]
- 25.Nelson JE, Gay EB, Berman AR, et al. Patients rate physician communication about lung cancer. Cancer. 2011;117:5212–5220. doi: 10.1002/cncr.26152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trice ED, Prigerson HG. Communication in end-stage cancer: review of the literature and future research. J Health Commun. 2009;14(Suppl 1):95–108. doi: 10.1080/10810730902806786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miyashita M, Sanjo M, Morita T, et al. Barriers to providing palliative care and priorities for future actions to advance palliative care in Japan: a nationwide expert opinion survey. J Palliat Med. 2007;10(2):390–399. doi: 10.1089/jpm.2006.0154. [DOI] [PubMed] [Google Scholar]
- 28.Feeg VD, Elebiary H. Exploratory study on end-of-life issues: barriers to palliative care and advance directives. Am J Hosp Palliat Care. 2005;22(2):119–124. doi: 10.1177/104990910502200207. [DOI] [PubMed] [Google Scholar]
- 29.Love A, Liversage LM. Barriers to accessing palliative care: a review of the literature. Progress in Palliative Care. 2014;22:9–19. doi: 10.1179/1743291X13Y.0000000055. [DOI] [Google Scholar]
- 30.Bernacki RE, Block SD. American College of Physicians High Value Care Task Force. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med. 2014;174(12):1994–2003. doi: 10.1001/jamainternmed.2014.5271. [DOI] [PubMed] [Google Scholar]
- 31.Parker SM, Clayton JM, Hancock K, et al. A systematic review of prognostic/end-of-life communication with adults in the advanced stages of a life-limiting illness: patient/caregiver preferences for the content, style, and timing of information. J Pain Symptom Manag. 2007;34:81–93. doi: 10.1016/j.jpainsymman.2006.09.035. [DOI] [PubMed] [Google Scholar]
- 32.Steinhauser KE, Christakis NA, Clipp EC, et al. Preparing for the end of life: Preferences of patients, families, physicians, and other care providers. J Pain Symptom Manage. 2001;22:727–737. doi: 10.1016/S0885-3924(01)00334-7. [DOI] [PubMed] [Google Scholar]
- 33.Steinhauser KE, Christakis NA, Clipp EC, et al. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284:2476–2482. doi: 10.1001/jama.284.19.2476. [DOI] [PubMed] [Google Scholar]
- 34.Steinhauser KE, Clipp EC, McNeilly M, et al. In search of a good death: observations of patients, families, and providers. Ann Intern Med. 2000;132:825–832. doi: 10.7326/0003-4819-132-10-200005160-00011. [DOI] [PubMed] [Google Scholar]
- 35.Yun YH, Lee CG, Kim SY, et al. The attitudes of cancer patients and their families toward the disclosure of terminal illness. J Clin Oncol. 2004;22:307–314. doi: 10.1200/JCO.2004.07.053. [DOI] [PubMed] [Google Scholar]
- 36.Hagerty RG, Butow PN, Ellis PA, et al. Cancer patient preferences for communication of prognosis in the metastatic setting. J Clin Oncol. 2004;22:1721–1730. doi: 10.1200/JCO.2004.04.095. [DOI] [PubMed] [Google Scholar]
- 37.Baile WF, Buckman R, Lenzi R, et al. SPIKES — a six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5:302–311. doi: 10.1634/theoncologist.5-4-302. [DOI] [PubMed] [Google Scholar]
- 38.Detering KM, Hancock AD, Reade MC, et al. The impact of advance care planning on end of life care in elderly patients: randomized controlled trial. BMJ. 2010;340:c1345. doi: 10.1136/bmj.c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Heyland DK, Dodek P, Rocker G, et al. Canadian Researchers' end-of-life network (CARENET). What matters most in end-of-life care: perceptions of seriously ill patients and their family members. CMAJ. 2006;174:627–633. doi: 10.1503/cmaj.050626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mack JW, Cronin A, Keating NL, et al. Associations between end-of-life discussion characteristics and care received near death: a prospective cohort study. J Clin Oncol. 2012;30:4387–4395. doi: 10.1200/JCO.2012.43.6055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mack JW, Cronin A, Taback N, et al. End-of-life care discussions among patients with advanced cancer: a cohort study. Ann Intern Med. 2012;156:204–210. doi: 10.7326/0003-4819-156-3-201202070-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heyland DK, Dodek P, You J, et al. Validation of quality indicators for end-of-life communication: results of a multicentre survey. CMAJ. 2017;189(30):E980–E989. doi: 10.1503/cmaj.160515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Elwyn G, Frosch D, Volandes AE, et al. Investing in deliberation: a definition and classification of decision support interventions for people facing difficult health decisions. Med Decis Mak. 2010;30:701–711. doi: 10.1177/0272989X10386231. [DOI] [PubMed] [Google Scholar]
- 44.Clayton JM, Butow PN, Tattersall MH, et al. Randomized controlled trial of a prompt list to help advanced cancer patients and their caregivers to ask questions about prognosis and end-of-life care. J Clin Oncol. 2007;25:715–723. doi: 10.1200/JCO.2006.06.7827. [DOI] [PubMed] [Google Scholar]
- 45.Volandes AE, Paasche-Orlow MK, Mitchell SL, et al. Randomized controlled trial of a video decision support tool for cardiopulmonary resuscitation decision making in advanced cancer. J Clin Oncol. 2013;31:380–386. doi: 10.1200/JCO.2012.43.9570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.El-Jawahri A, Podgurski LM, Eichler AF, et al. Use of video to facilitate end-of-life discussions with patients with cancer: a randomized controlled trial. J Clin Oncol. 2010;28:305–310. doi: 10.1200/JCO.2009.24.7502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stacey D, Bennett CL, Barry MJ, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2011;10:CD001431. doi: 10.1002/14651858.CD001431.pub3. [DOI] [PubMed] [Google Scholar]
- 48.Werner P, Carmel S, Ziedenberg H. Nurses' and social workers' attitudes and beliefs about and involvement in life-sustaining treatment decisions. Health Soc Work. 2004;29(1):27–35. doi: 10.1093/hsw/29.1.27. [DOI] [PubMed] [Google Scholar]
- 49.Heyman JC, Gutheil IA. Social work involvement in end of life planning. J Gerontol Soc Work. 2006;47(3–4):47–61. doi: 10.1300/J083v47n03_04. [DOI] [PubMed] [Google Scholar]
- 50.Meintzer, J., et al. The Role of Speech-Language Pathologists, Audiologists and Communication Health Assistants in End-of-Life Care. 2016; Available from: http://www.sac-oac.ca/sites/default/files/resources/end-of-life_position-statement_en.pdf. Accessed 17 Feb 2017.
- 51.The Canadian Association of Occupational Therapists CAOT position statement: occupational therapy and end-of-life care. Occupational Therapy Now. 2008;10(6):23–25. [Google Scholar]
- 52.Canadian Physiotherapy Association, C.P. Position Statement Primary Health Care. November, 2006; Available from: https://physiotherapy.ca/sites/default/files/positionstatements/primary-health-care_en.pdf. Accessed 24 Feb 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Mean scores from physicians and nurses on a Likert scale, rating barriers related to patient and family factors, the role of physicians and nurses from their own perspective, system and external factors, and the role of physicians from nurses’ perspective. (DOCX 19 kb)
Mean Likert scores, physicians and nurses rating their own willingness to engage in goals of care discussions. (DOCX 50 kb)
Mean scores from physicians and nurses on a Likert scale, rating their perceptions of inter-professional roles in communicating and decision-making around goals of care. (DOCX 91 kb)
Data Availability Statement
The study database is available from the authors upon request.