Supplemental Digital Content is available in the text
Keywords: meta-analyses, prediabetes, protocol, systematic review, yoga
Abstract
Background:
Type 2 diabetes mellitus (T2DM) is becoming a leading problem worldwide. Emerging reports reveal alarming evidence of increasing prevalence of T2DM that has reached pandemic levels. Despite the significant incidence, there are limited reliable data resources and comprehensive systematic review and meta-analysis on the effects of yoga on people who are a prediabetic or high risk for developing T2DM.
Objective:
The objective of this protocol is to conduct a full-scale systematic review and meta-analyses on the effects of yoga on people who are prediabetes or high risk of developing T2DM.
Methods:
The articles enrolled in the study will be retrieved from the online databases between 2002 and the date the searches are executed. The searches will be repeated just before the final analyses and further relevant studies for inclusion. We will conduct a bibliographic search in databases: Medline/PubMed, Scopus, Cochrane Library, EBSCO, and IndMED using keywords including prediabetes state, high risk for diabetes, metabolic syndrome, and yoga. A defined search strategy will be implemented along with selection criteria to obtain full-text articles of relevant studies. This study protocol was prepared according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis for Protocols 2015 guidelines. There will be no language restrictions.
Ethics and dissemination:
The proposed study will be based on published studies and publicly available anonymized data without directly involving human participants and therefore requires neither formal human ethical review nor approval by a human research ethics committee. We published an outline of the protocol in the International Prospective Register of Systematic Reviews (PROSPERO) in 2018. We plan to disseminate the findings of this systematic review and meta-analysis through publication in a peer-reviewed journal and presentation at relevant conference proceedings. In addition, we believe the results of the systematic review will have implications for policy and practice. We will prepare policymaker summary using a validated format, disseminate through social media and email discussion groups.
Review registration number:
PROSPERO registration number CRD 42018106657
1. Introduction
Type 2 diabetes mellitus (T2DM) is one of the greatest public health challenges in today's world.[1] The body becomes either resistant to insulin or gradually loses the ability to produce insulin.[2] According to the World Health Organization, global report on diabetes incidence, an estimated 422 million people were found to be living with diabetes in 2014.[3] International Diabetes Federation reported that it is estimated that there will be 629 million people with diabetes by the end of 2045, and diabetes-related health expenditure will exceed US$776 billion.[4]
The development and maintenance of T2DM are attributed to sedentary lifestyle,[5] unhealthy diet, and psychologic stress. Psychologic stress has a strong correlation with both the risk factors[6–8] and maintenance of the disease.[9,10] Several acquired risk factors such as prediabetic state contribute to the development of T2DM apart from the genetic background.[5,11]
Many complementary and alternative practices are explored by people in both the prevention and treatment of diabetes.[12,13] Yoga is one such Eastern practice that originated in India over 5000 years ago principally to develop mental faculties.[14,15] Yoga advocates that a healthy body is a by-product of healthy mind.[16,17] Most importantly, a growing body of research suggests that the practice of yoga may reduce insulin resistance syndrome and may attenuate signs, reduce complications, and improve the prognosis of diabetes.[18–23] Also, studies have shown that the progression of diabetic condition from prediabetes could be either delayed or halted with regular physical activity,[24–27] healthy diet,[27] and effective stress management.[28,29]
It is proposed yoga intervenes T2DM by 2 proposed mechanisms downregulation of both the hypothalamic pituitary adrenal axis and the sympathetic nervous system.[30–32]
2. Rationale
2.1. What is the issue and how will our study address this?
Several studies in the prediabetic population show the effectiveness of yoga in reducing the risk of progression to diabetic state.[33–36] There is not a single review to show the benefits of yoga in prediabetes. This will be the 1st systematic review that will show evidence that yoga significantly affects the prediabetic state and will summarize the results of these available studies. This study will announce the gaps in present research and will set directions for future research. The study will further provide evidence for people to adopt yoga practise as an attractive alternative to other forms of physical training especially for people who are discouraged by the perceived rigor of other exercises.
2.2. Review questions
The aim of our systematic review and meta-analysis protocol is to describe the methodologic approach for conducting a systematic review and meta-analysis to examine the effects of yoga on people who are prediabetic or high risk for developing T2DM.
The questions for this review are as follows:
-
1.
Does yoga delay or prevent the progression of diabetes in prediabetic population?
-
2.
What is the significance of yoga compared with exercise in a prediabetic population?
-
3.
How much does the effect size of physiologic outcomes vary across studies and subgroups?
3. Methods
3.1. Search strategy and study selection
The proposed systematic review and meta-analysis will be performed according to the guidelines of Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement issued in 2015. The authors will consider the published studies explaining the effectives of yoga in prediabetic and metabolic syndrome with no restrictions on study participant's age, ethnicity, morbidity, and occupation. There will be no language restrictions. The authors will perform a literature search using 5 computerized English and Indian scientific electronic bibliographic databases: PubMed, Scopus, Cochrane Library, EBSCO, and IndMED. The search strategy will include only search terms related to “yoga” and “cardiovascular disease risk factors” and adapted for each database as necessary. Studies published between 2002 and the date the searches executed will be sought. The searches will be repeated just before the final analyses. Many searches in the proposed study will be undertaken to ensure the identification of eligible studies using one of the several search term combinations for the effectiveness of yoga on the high risk of diabetes or prediabetic population or metabolic syndrome (prediabetes state, high risk for diabetes, metabolic syndrome, and yoga). Keywords used were: “yoga [abstract],” “prediabetes [abstract],” and “glucose [text].” Keywords used included yoga + type 2 diabetes [in the title of the article], yoga + type II diabetes [in the title of the article], and exercise therapy + type 2 diabetes patients [in the title of the article].
3.2. Search strategy
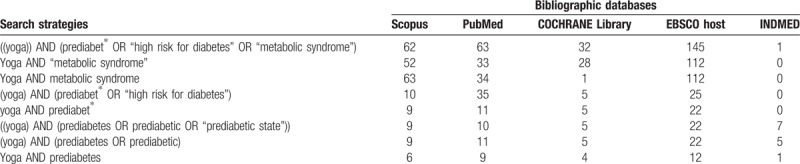
A draft search strategy for the databases and search string that will be used to identify the studies describing effects of yoga in prediabetic and metabolic syndrome is shown in Table 1.
Table 1.
Search strings and databases used for the review and analysis.
3.3. Study selection criteria
3.3.1. Inclusion criteria
-
1.
Study examining yoga intervention (including at least one of asana, pranayama, meditation) to promote T2DM management and comparing yoga intervention with other usual care or physical exercise or nontherapeutic intervention.
-
2.
Study that is randomized control trial, randomized cross-over studies, cluster-randomized trials, or quasi-experimental design will be included.
-
3.
Studies evaluating the primary outcome measure-glycemic control, measured in both the intervention and control group conditions as well as other measures such as HbA1c, blood pressure, or fasting blood sugar, and lipid profile (triglycerides, high-, and low-density lipoprotein [HDL and LDL] cholesterol, systolic blood pressure [SBP], and diastolic blood pressure [DBP]) will be included.
-
4.
Study participants must be prediabetic or designated as high risk for diabetes because of physiologic measures, and the outcomes must be reported specifically for each group
3.3.2. Exclusion criteria
-
1.
Studies will be excluded if participants were members of a specific age group, such as adolescents or geriatric age groups.
-
2.
Studies will be excluded if participants were all in a transient state, such as pregnancy or menopause.
-
3.
Studies will be excluded if the yoga intervention was modified to a dance program.
-
4.
Conference proceedings, editorials, commentaries, and book chapters/book reviews will be excluded.
3.4. Data extraction and management
Two authors will be involved in data extraction and independently evaluate the published studies with the selection criteria, and corresponding authors will be contacted for missing information in the studies. Data will be extracted on study design and methods, demographic characteristics of study participants, as well as details of yoga interventions, control interventions, and outcome measures PRISMA guidelines will be used to prepare the data extraction form using MS Excel data extraction form. This form will be utilized to standardize the data collection process.
3.5. Selection process
The relevant titles and abstracts will be screened with the selection criteria and PRISMA guidelines for eligibility by the first author. Potential full-text eligible articles will be downloaded and reviewed independently by the authors. The corresponding author will perform a final review for the double check to recover any omitted articles in the analysis. The references of the selected articles will be imported into EndNote file to form an initial list of eligible studies following that duplicates will then be removed. All the authors will be involved in the selection process, and a file will be removed only when there is an agreement that it did not fulfill the eligibility criteria. Any discrepancies associated with selection of the studies will be resolved by mutual discussions involving the third reviewer. The entire selection process is illustrated in Figure 1.
Figure 1.
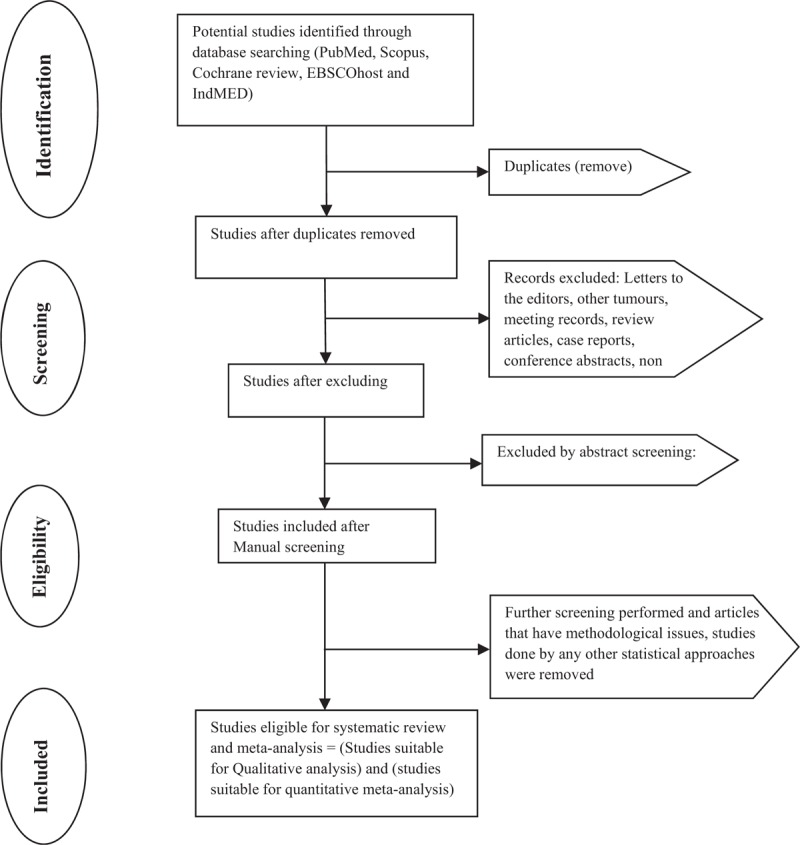
Flowchart of systematic review according to Preferred Reporting Items for Systematic Reviews and Meta-Analysis for Protocols statement.
3.6. Data items
The authors will extract 6 categories of data:
-
1.
Bibliometric data (1st author, year of publication, country, a journal of publication, the study period).
-
2.
Study design (a type of research, details of randomised control trial, randomized cross-over studies and cluster-randomized trials or quasi-experimental design and the validity of confirmative diagnosis and method of data collection).
-
3.
Study participants characteristics (condition, age, gender, race, sample size, and sampling procedures).
-
4.
Yoga interventions characteristics (yoga type: asana, pranayama, meditation, components, frequency, duration).
-
5.
Control interventions characteristics (type: usual care or physical exercise or nontherapeutic intervention, frequency, duration).
-
6.
Outcome measures: SBP, DBP; heart rate; respiratory rate; abdominal obesity (waist circumference, waist-hip ratio, index of central obesity); blood lipid levels (triglycerides, HDL, and LDL cholesterol); glycemic control (both the intervention and control group conditions, such as HbA1c, blood pressure, or fasting blood sugar).
3.7. Study outcomes
3.7.1. Primary outcome
The primary outcome is to measure the glycemic control (HbA1c, fasting blood glucose [FBG], and postprandial glucose [PPBG]) in both the intervention and control group conditions.
3.7.2. Secondary outcomes
The secondary outcomes are to measure other markers of diabetes management including triglycerides, HDL, LDL, SBP, DBP, body composition, and fasting cortisol.
3.8. Assessment of risk of bias
Risk of bias of included studies will be assessed using the Cochrane Risk of Bias Assessment tool that contains several items under 7 categories such as random sequence generation, allocation concealment, blinding of participants and investigators, the blindness of outcome assessments, incomplete outcome data, selective outcome reporting, and other biases. Based on the assessment, the studies will be evaluated as low, unclear, or high bias. The Jadad scale will be used to evaluate the quality of each trial where three domains in the scale cover Randomization (0–2 points), blinding (0–2 points), and dropouts and withdrawals (0–1 point). A trial with a score ≤2 indicates low quality while a score of ≥3 indicates high quality. Assessment of publication bias will be performed using funnel plots generated by Comprehensive Meta-Analysis (CMA) 3.0 software.
3.9. Data synthesis
Data will be synthesised into 3 different steps:
-
1.
Step 1 will provide a descriptive overview (qualitative data synthesis or Systematic Review based on selection criteria and PRISMA guidelines).
-
2.
Step 2 will provide a quantitative analysis of the characteristics of the selected studies (calculation of pooled estimates and meta-analysis). Meta-analysis will calculate pooled estimates of the study findings on the effectiveness of yoga interventions on the glycemic status of the prediabetic population.
-
3.
Step 3 will examine the influence of study, participant, and outcome characteristics based on the difference in intervention among the prediabetic population by conducting subgroup and meta-regression analyses.
3.10. Meta-analysis
Meta-analyses on the effectiveness of yoga interventions on the glycemic status of the prediabetic population will be performed using CMA 3.0 for the obtained pooled estimates, standardized mean difference (SMD) and 95% confidence intervals from the included studies. Forest plots will be generated to show the pooled effect size of the study findings and with random-effects models of meta-analysis due to between-study heterogeneity into the model. Heterogeneity will be calculated using Cochrane Q test and I2 statistic. Q statistics will be estimated for each outcome and provides a test of the null hypothesis that all studies in the proposed meta-analysis share a common effect size. If all studies shared the same effect size, the expected value of Q would be equal to the degrees of freedom (the number of studies minus 1). I2 statistics informs what proportion of the observed variance reflects the difference in true effects sizes rather than sampling error. Z-statistic will be performed to assess heterogeneity. FBG, PPBG, TC, LDL-c, VLDL-c, HDL-c, and TG are reported as mg/dL, where studies reported as mmol/L a numerical conversion to mg/dL will be done. HbA1c is reported.
3.11. Publication bias
Publication bias of the included studies will be assessed using Egger bias indicator test, Orwin and Classic fail-safe N test, Begg and Mazumdar rank collection test, Duval and Tweedie trim and fill[37] calculation. An inverted funnel plot will be constructed simultaneously alongside the forest plot, with the aid of SMD (SMD values used in the meta-analysis) and the standard error. The symmetrical funnel plots will indicate low risk, and asymmetrical funnel plots will indicate a high risk of publication bias.
3.12. Subgroup analyses
Subgroup analyses will be performed according to study, participant and outcome characteristics and methodologic factors if sufficient studies and retrieved data are identified and available. We plan to investigate specific subgroup analyses according to differences in intervention and key features of identified study participants such as condition, age, gender, race, sample size, and sampling procedures, follow-up, clinical setting, of prediabetic participants. Further, specific subgroup analyses will be performed based on the outcome measures such as blood pressure (systolic, diastolic); heart rate; respiratory rate; abdominal obesity (waist circumference, waist-hip ratio, index of central obesity); blood lipid levels (triglycerides, HDL, and LDL cholesterol); glycemic control (both the intervention and control group conditions, such as HbA1c, blood pressure, or fasting blood sugar) (if sufficient additional information is identified and available). Tables, flowchart, and figures will be plotted to depict the results appealingly.
4. Meta-regression
Prediabetic participant characteristics such as gender, methods of data collection, sample size, research quality, and sampling procedure will be evaluated. A random-effects model will be selected and assigned to weight for each study by calculating R2 with the quantity of the proposed variance. The heterogeneity of intervention associations with one or more study variables will be explained using meta-regression analysis.
5. Reporting of this review and its findings
The findings will be published as per PRISMA guidelines.[38] A flowchart will be employed to outline the selection process (Fig. 1). Text description will be used to review the qualitative data of the included studies. Outputs of meta-analyses will be depicted in a forest plot. Publication bias will be represented in the inverted funnel plot. The search strategy will be provided in Supplement Table 1 (Supplemental Digital Content).
Author contributions
Conceptualization: Ramya Ramamoorthi, Daniel Gahreman, Simon Moss, Timothy Skinner.
Data curation: Ramya Ramamoorthi, Daniel Gahreman, Simon Moss.
Investigation: Ramya Ramamoorthi.
Methodology: Ramya Ramamoorthi.
Project administration: Ramya Ramamoorthi.
Resources: Ramya Ramamoorthi.
Supervision: Daniel Gahreman, Simon Moss, Timothy Skinner.
Validation: Ramya Ramamoorthi, Daniel Gahreman.
Visualization: Ramya Ramamoorthi.
Writing – original draft: Ramya Ramamoorthi.
Writing – review & editing: Ramya Ramamoorthi, Daniel Gahreman, Simon Moss, Timothy Skinner.
Supplementary Material
Footnotes
Abbreviations: CMA = comprehensive meta-analysis, DBP = diastolic blood pressure, FBG = fasting blood glucose, HbA1c = hemoglobin A1C, HDL = high-density lipoprotein, LDL = low-density lipoprotein, PPBG = postprandial blood glucose, PRISMA-P = Preferred Reporting Items for Systematic Reviews and Meta-Analysis for Protocols, PROSPERO = the protocol in the International Prospective Register of Systematic Reviews, SBP = systolic blood pressure, SMD = standardized mean difference, T2DM = type 2 diabetes mellitus, TC = total cholesterol, VLDL = very low-density lipoproteins.
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Chen L, Magliano DJ, Zimmet PZ. The worldwide epidemiology of type 2 diabetes mellitus—present and future perspectives. Nat Rev Endocrinol 2011;8:228–36. [DOI] [PubMed] [Google Scholar]
- [2].Gardner CD, Trepanowski JF, Del Gobbo LC, et al. Effect of low-fat vs low-carbohydrate diet on 12-month weight loss in overweight adults and the association with genotype pattern or insulin secretion: the DIETFITS randomized clinical trial. JAMA 2018;319:667–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Fact sheet on Diabetes. WHO. 2017. Available at: http://www.who.int/news-room/fact-sheets/detail/diabetes. [Google Scholar]
- [4].International Diabetes Federation. 2017. Available at: https://www.idf.org/ [DOI] [PubMed] [Google Scholar]
- [5].Violi F, Targher G, Vestri A, et al. Effect of aspirin on renal disease progression in patients with type 2 diabetes: a multicenter, double-blind, placebo-controlled, randomized trial. The renaL disEase progression by aspirin in diabetic pAtients (LEDA) trial. Rationale and study design. Am Heart J 2017;189:120–7. [DOI] [PubMed] [Google Scholar]
- [6].Yudkin JS, Kumari M, Humphries SE, et al. Inflammation, obesity, stress and coronary heart disease: is interleukin-6 the link? Atherosclerosis 2000;148:209–14. [DOI] [PubMed] [Google Scholar]
- [7].Heraclides A, Chandola T, Witte DR, et al. Psychosocial stress at work doubles the risk of type 2 diabetes in middle-aged women: evidence from the Whitehall II study. Diabetes Care 2009;32:2230–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Black PH. The inflammatory response is an integral part of the stress response: implications for atherosclerosis, insulin resistance, type II diabetes and metabolic syndrome X. Brain Behav Immun 2003;17:350–64. [DOI] [PubMed] [Google Scholar]
- [9].Delamater AM, Jacobson AM, Anderson B, et al. Psychosocial therapies in diabetes: report of the Psychosocial Therapies Working Group. Diabetes Care 2001;24:1286–92. [DOI] [PubMed] [Google Scholar]
- [10].Faulenbach M, Uthoff H, Schwegler K, et al. Effect of psychological stress on glucose control in patients with type 2 diabetes. Diabet Med 2012;29:128–31. [DOI] [PubMed] [Google Scholar]
- [11].Bonora E, Kiechl S, Willeit J, et al. Population-based incidence rates and risk factors for type 2 diabetes in white individuals: the Bruneck study. Diabetes 2004;53:1782–9. [DOI] [PubMed] [Google Scholar]
- [12].Falci L, Shi Z, Greenlee H. Peer reviewed: multiple chronic conditions and use of complementary and alternative medicine among US adults: results from the 2012 National Health Interview Survey. Prev Chronic Dis 2016;13:E61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Medagama AB, Bandara R. The use of complementary and alternative medicines (CAMs) in the treatment of diabetes mellitus: is continued use safe and effective? Nutr J 2014;13:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Singh K. Effect of yoga on dental care: pranayama techniques or rhythmic breathing exercises on the oral hygiene and gingival bleeding. Int J App Dent Sci 2017;3:91–5. [Google Scholar]
- [15].Mooventhan A, Nivethitha L. Evidence based effects of yoga practice on various health related problems of elderly people: a review. J Bodyw Mov Ther 2017;21:1028–32. [DOI] [PubMed] [Google Scholar]
- [16].Kumar V, Poonia P. Impact of yoga on psychological health. Int J Yogic Hum Mov Sport Sci 2017;2:248–50. [Google Scholar]
- [17].Weinstein R. 2018. North American Yoga Practitioners’ Lived Experiences of Mind-Body Connection: A Phenomenological Study Adler School of Professional Psychology, ProQuest Dissertations Publishing, 10788413. [DOI] [PubMed] [Google Scholar]
- [18].Pandya DP, Vyas VH, Vyas SH. Mind-body therapy in the management and prevention of coronary disease. Compr Ther 1999;25:283–93. [DOI] [PubMed] [Google Scholar]
- [19].Damodaran A, Malathi A, Patil N, et al. Therapeutic potential of yoga practices in modifying cardiovascular risk profile in middle aged men and women. J Assoc Physicians India 2002;50:633–40. [PubMed] [Google Scholar]
- [20].Sahay B, Sahay RK. Lifestyle modification in management of diabetes mellitus. J Indian Med Assoc 2002;100:178–80. [PubMed] [Google Scholar]
- [21].Garfinkel M, Schumacher HR., Jr Yoga. Rheum Dis Clin North Am 2000;26:125–32. [DOI] [PubMed] [Google Scholar]
- [22].Chandler K. The emerging field of yoga therapy. Hawaii Med J 2001;60:286–7. [PubMed] [Google Scholar]
- [23].Raub JA. Psychophysiologic effects of Hatha yoga on musculoskeletal and cardiopulmonary function: a literature review. J Altern Complement Med 2002;8:797–812. [DOI] [PubMed] [Google Scholar]
- [24].Colberg SR, Sigal RJ, Yardley JE, et al. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care 2016;39:2065–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Schellenberg ES, Dryden DM, Vandermeer B, et al. Lifestyle interventions for patients with and at risk for type 2 diabetes: a systematic review and meta-analysis. Ann Intern Med 2013;159:543–51. [DOI] [PubMed] [Google Scholar]
- [26].Sanders AB. Effectiveness of a low dose behavior change intervention on physical activity maintenance following an exercise trial in pre-type II diabetics: Colorado State University. Libraries; Thesis 2017. [Google Scholar]
- [27].Katula JA, Kirk JK, Pedley CF, et al. The Lifestyle Intervention for the Treatment of Diabetes study (LIFT Diabetes): design and baseline characteristics for a randomized translational trial to improve control of cardiovascular disease risk factors. Contemp Clin Trials 2017;53:89–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].O’Dea A, Tierney M, McGuire BE, et al. Can the onset of type 2 diabetes be delayed by a group-based lifestyle intervention in women with prediabetes following gestational diabetes mellitus (GDM)? Findings from a randomized control mixed methods trial. J Diabetes Res 2015;2015: 798460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Hardie EA, Critchley CR, Moore SM. Prediabetes Subtypes: patterns of risk, vulnerabilities, and intervention needs. Aust Psychol 2015;50:455–63. [Google Scholar]
- [30].Sengupta P. Health impacts of yoga and pranayama: a state-of-the-art review. Int J Prev Med 2012;3:444–58. [PMC free article] [PubMed] [Google Scholar]
- [31].Rahman F, Ferdousi S. Effect of deep relaxation technique on cardiac autonomic dysfunction in type 2 diabetes mellitus. J Bangla Soc Physiol 2018;13:22–8. [Google Scholar]
- [32].Pal G, Velkumary S, Madanmohan Effect of short-term practice of breathing exercises on autonomic functions in normal human volunteers. Indian J Med Res 2004;120:115–21. [PubMed] [Google Scholar]
- [33].Mooventhan A. A narrative review on role of Yoga as an adjuvant in the management of risk factor, disease progression and the complications of type 2 diabetes mellitus. Diabetes Metabo Syndr 2017;11Suppl 1:S343–6. [DOI] [PubMed] [Google Scholar]
- [34].Sinha SS, Jain AK, Tyagi S, et al. Effect of 6 months of meditation on blood sugar, glycosylated hemoglobin, and insulin levels in patients of coronary artery disease. Int J Yoga 2018;11:122–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].McDermott KA, Rao MR, Nagarathna R, et al. A yoga intervention for type 2 diabetes risk reduction: a pilot randomized controlled trial. BMC Complement Altern Med 2014;14:212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Netam R, Yadav RK, Khadgawat R, et al. Interleukin-6, vitamin D & diabetes risk-factors modified by a short-term yoga-based lifestyle intervention in overweight/obese individuals. Indian J Med Res 2015;141:775–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Duval S, Tweedie R. Trim and fill: a simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000;56:455–63. [DOI] [PubMed] [Google Scholar]
- [38].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


