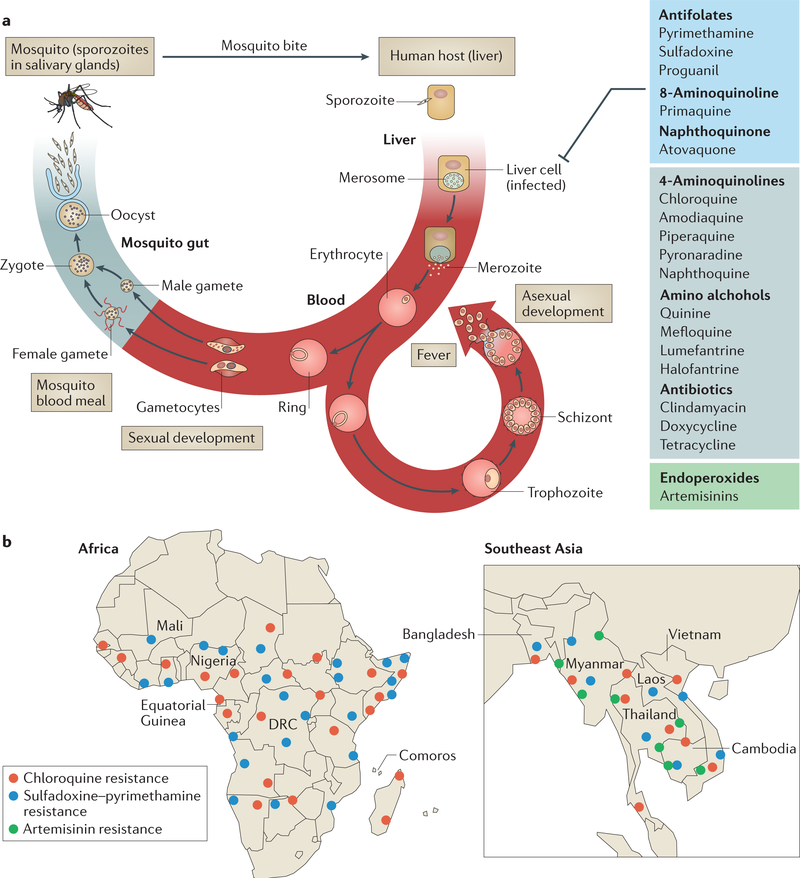
Figure 1 |. Life cycle of Plasmodium falciparum and epidemiology of antimalarial drug resistance.
a | Infection begins when a mosquito bite releases sporozoites into the bloodstream of the vertebrate host. Sporozoites subsequently infect hepatocytes, in which they proliferate and develop into merozoites. Merozoites are released into blood, where they invade erythrocytes. The parasites develop into the ring form and subsequently develop into proliferative (and morphologically distinct) trophozoite and schizont stages. When the schizont lyses, new merozoites are released, which initiate a new asexual cycle in the blood. A small proportion of ring-form parasites develop into gametocytes (sexual stages), which are taken up by the mosquito during a blood meal. In the mosquito midgut, male and female gametes emerge and fuse to form zygotes, which further differentiate into oocysts. Each oocyst divides to produce and release thousands of haploid sporozoites into the mosquito body cavity. These sporozoites travel and invade the mosquito salivary glands, from where they are injected into the human host. Trophozoite and schizont stages are sequestered in host tissue to cause severe disease. All antimalarial classes shown (and comprehensively reviewed in TABLE 1) target the asexual trophozoite and schizont stages. Antifolates, primaquine (8-aminoquinoline) and atovaquone (naphthoquinone) also target liver-stage parasites. Endoperoxides (artemisinins) target all asexual and early sexual blood-stage parasites. Primaquine is the only drug that targets latency in the liver to prevent the relapsing infection characteristic of Plasmodium vivax. b | Detailed maps showing the distribution of P. falciparum resistance to chloroquine, sulfadoxine-pyrimethamine and artemisinin in Africa and southeast Asia18,19,21,61,62,74,119–125. Artemisinin resistance is based on two criteria: clearance and PfKelch13-associated mutation. Although the A578S mutation has been reported115, no pfkelch13 mutations associated with resistance have been reported yet in Bangladesh (resistance is indicated at the Bangladesh-Myanmar border). Resistance to chloroquine and sulfadoxine- pyrimethamine (but not artemisinin) has emerged in the Amazon basin of South America126 (not shown). Resistance of P. vivax to chloroquine is emerging127 (not shown). Each dot represents a region of emergence of drug resistance. DRC, Democratic Republic of the Congo. Part a adapted from REF. 128.