Abstract
Background
Dermatology patients continue to receive improved treatment, but for patients with psoriasis, there have been few studies on ways to improve patient management by improving communication with patients and their dermatologists. This study aimed to investigate the feasibility and efficacy of cloud-based interactive patient and physician management of psoriasis.
Material/Methods
The cloud-based platform was created by professional software engineers to educate and manage patients with psoriasis in a single hospital, where patients and research staff had a network platform for sharing data. A total of 79 patients with psoriasis were included in this study and were randomly divided into the control group (n=39) and the intervention group (n=40). Patients in the control group were given a psoriasis nursing manual and underwent regular follow-up. Patients in the intervention group were managed using the cloud platform, with the same management as the control group. The Psoriasis Area Severity Index (PASI), the Self-Rating Anxiety Scale (SAS), the Dermatology Life Quality Index (DLQI), and the Symptom Checklist-90-Revised (SCL-90-R) were used.
Results
Cloud-based interactive patient and physician management resulted in clinical improvement, and reduced the degree of anxiety in patients with psoriasis and improved their physical and mental health. Patients in the intervention group had an improved understanding of psoriasis treatment, resulting in an improved relationship with the medical staff and improved treatment compliance.
Conclusions
Cloud-based interactive patient and physician management improved the mental health and quality of life for patients with psoriasis and allowed patients to manage their disease more effectively.
MeSH Keywords: Mental Health, Psoriasis, Quality of Life
Background
Worldwide, psoriasis is as a chronic autoimmune and inflammatory disease of the skin, which affects between 2–3% of people and which can have an adverse effect on the quality of life [1,2]. The pathogenesis of psoriasis remains unclear although it is an autoimmune condition with a genetic basis, the severity of symptoms are associated with immune, infectious, endocrine, psychological, traumatic, temperature, and other factors [3,4]. Patients with psoriasis present with skin lesions, pruritus, and desquamation, and the disease is rarely curable. Also, because of the chronic course of psoriasis and the repeated episodes of this condition, it can lead to a variety of psychological problems in patients, including increased anxiety. Psychological symptoms have been shown to further aggravate the severity of the signs and symptoms of psoriasis [5,6]. Therefore, psoriasis is not only associated with skin disease but also has a significant psychosomatic component.
Patients with psoriasis require targeted individualized health education to develop self-management skills within the scope of their ability, and even patients with well-controlled psoriasis of varying severity have been shown to have unmet health education needs [7]. The traditional roles of nurses and physicians include varying degrees of health education at diagnosis and outpatient follow-up, but which lack guidelines and vary in quality and amount [8]. Currently, there is usually a lack of direct interaction between the patients and physicians and nurses, due to the lack of time and the large healthcare resources required to provide individualized and continued patient information, guidance, and monitoring of patient self-management in psoriasis [8].
The recently developed use of multimedia technology in healthcare has been shown to be a potentially powerful way to provide information and support for patients in an efficient way, including the provision of patient health education and disease management [9]. The use of modern multimedia for patient health education is more image-based and interactive than traditional health education methods and can be more interesting, which improves both the uptake of the information and patient compliance with such programs. Studies have now shown that patient satisfaction and knowledge are significantly increased with the use of multimedia health education when compared with traditional patient education methods, and can also reduce the workload of physicians and nurses, resulting in standardized information and improved patient treatment and self-management compliance [10,11].
Therefore, the aims of the present study were to investigate the feasibility and efficacy of cloud-based interactive patient and physician management of psoriasis using a demand-oriented multimedia application (app) to identify the individual needs of patients to build a convenient and efficient health management system.
Material and Methods
Patient enrollment and grouping
A total of 79 patients from our hospital were enrolled in this study from May 7, 2015, to July 30, 2016, and were randomly divided into the control group (n=39) and the intervention group (n=40). Patients in the control group were given a psoriasis nursing manual and followed-up regularly. Patients in the intervention group were managed using the application (app) on the cloud platform, with psoriasis management items that were the same as those of the control group. The Local Ethics Committee approved this study, and all study participants provided informed consent.
Inclusion and exclusion criteria
Participants who were included in the study had a confirmed diagnosis of psoriasis and more than one month’s duration, an ability to listen, speak, read, and write independently, and to complete the study questionnaires and operate the application (app) system independently, who had no mental illness, and who were willing to take part in the study. The exclusion criteria included patients with psoriasis who were suffering from other serious diseases, who had a mental illness, and who were unable or unwilling to take part in the study.
Cloud-based interactive patient and physician management
The advantage of the cloud platform was that it allowed patients to receive professional health education and to transmit personal information to the cloud to get timely guidance from physicians. According to the cloud platform, patients can view the medical education information on psoriasis and upload their data. The physician was then able to understand the patient information on the platform and carry out appropriate health management. The workflow process of the cloud-based patient and physician medical interactive management in psoriasis is shown in Figure 1.
Figure 1.
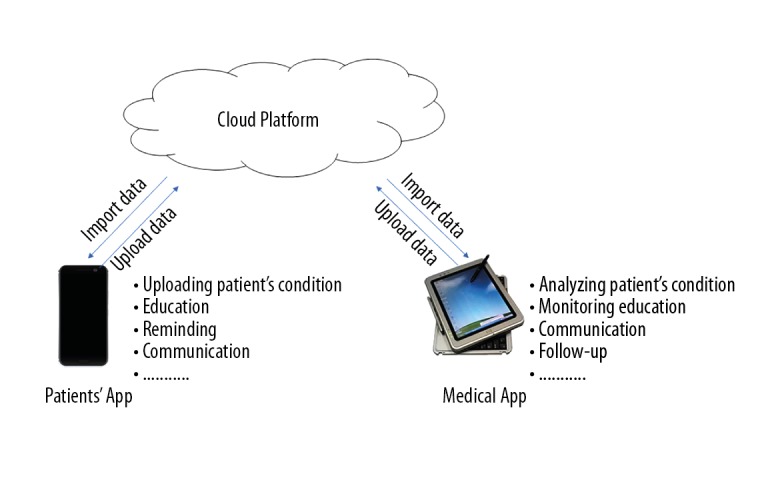
Workflow process of cloud-based patient and physician medical interactive management in psoriasis.
The content of the cloud-based platform, the application (app), and data record of patients with psoriasis (completed daily)
The cloud-based platform included questions on the physiological and psychological aspects of psoriasis and patient needs. The physiological questions included the degree of itching and pain from the skin lesions, which were evaluated daily using a visual analog scale (VAS), patients photographed their skin lesions daily and uploaded the images were analyzed using platform-specific software intelligence to analyze the severity of the skin lesions, and for patients with diabetes or hypertension, patients completed daily blood glucose and blood pressure measurements as accurately as possible.
The psychological questions included weekly responses using an anxiety and depression scale, following treatment. The platform recorded the data and presented a trend map, for nurses to understand the psychological changes that occurred during patient hospitalization.
Patients also completed a monthly Patient Needs Questionnaire for psoriasis, which included a 5-point scale ranging from 0 (not important) to 4 (very important), which was used to allow physicians to understand the needs of the patient to provide individualized health management services.
Health education for patients using the cloud-based platform
Health education for patients with psoriasis included one of the following six topics, one per day: an introduction to understanding psoriasis; self-care guidance for managing the psoriasis skin lesions; diet and exercise guidance for patients with psoriasis; guidance and precautions for the use of oral and topical treatments for psoriasis; physical therapy for psoriasis, including phototherapy and hydrotherapy; and the diagnostic findings and diagnosis of psoriasis. The six aspects of medical education used text, pictures, videos, and other multimedia images to provide health education to patients. Patients were able to view videos and written information each day.
The cloud-based platform had a reminder function that included a time-controlled pop-up dialog box at the following times: at the time required for taking medicine each day, to improve treatment compliance; and to remind the patient to enter each day’s data.
The cloud-based platform for physicians and nurses
The working cloud-based platform for physicians and nurses consisted of three components, the daily data for each patient, the ability to advise on treatment and improve treatment compliance, and the ability to provide online advice and counseling. Physicians were able to see the daily data of all patients with psoriasis on the platform interface, including a data trend map, the patient’s psychological status, any need for hospitalization, blood glucose and blood pressure measurements. The physician provided individualized guidance, including psychological care, health education, and behavioral intervention. Physicians were able to see videos of the patients on the platform interface every day if patients do not insist on watching. Physicians were able to supervise and encourage patients, improve treatment compliance, improve patient knowledge of disease health education and improve their self-management ability. Physicians were able to provide online counseling and communication services for patients with the help of remote assistance and regular follow-up.
Scoring methods and content: The Psoriasis Area Severity Index (PASI), the Dermatology Life Quality Index (DLQI), the Self-Rating Anxiety Scale (SAS), and the Symptom Checklist-90-Revised (SCL-90-R)
The Psoriasis Area Severity Index (PASI) was used to compare the total score of the two groups before and after the intervention, to evaluate the effect of the cloud-based platform using the PASI scoring criteria [12]. To subjectively evaluate the impact of psoriasis on patient physiology, psychology, and quality of life, the Dermatology Life Quality Index (DLQI) was used [13]. The DLQI evaluation usually takes only three minutes to complete and has been previously shown to be a good indicator for the evaluation of psychosomatic diseases. The Self-Rating Anxiety Scale (SAS) is mainly applicable to patients with symptoms of anxiety, and to assess their subjective feelings of anxiety, using 20 main questions, with scores being <40 for normal, 40–60 for moderate anxiety, and ≥60 for severe anxiety [14]. The Symptom Checklist-90-Revised (SCL-90-R) was used to assess mental health and included the assessment of nine symptoms of psychopathology and three global anxiety indices [15].
Statistical analysis
Data were analyzed using the Statistical Product and Service Solutions (SPSS) version 18.0 statistical analysis software (SPSS Inc., Chicago, IL, USA). Data were expressed as the mean ± standard deviation (SD) and analyzed by analysis of variance and were also represented as the percentage (%). The chi-squared (χ2) test was used. A P-value of <0.05 was considered to be statistically significant.
Results
General characteristics of the patients of the two study groups
A total of 79 patients were included in this study and randomly divided into the control group (n=39) and the intervention group (n=40). There were no significant differences in patient age and the course of psoriasis between the control group and the intervention group. The baseline characteristics of the patients are summarized in Table 1.
Table 1.
Comparison of the demographic and clinical information of individuals between the two groups.
| Group | n | Gender | Age (yrs) | Course of disease | Current therapies | |||
|---|---|---|---|---|---|---|---|---|
| Male | Female | None | Emollients only | Active therapies | ||||
| Control group | 39 | 22 | 17 | 44.3±18.6 | 11.70±12.76 | 2 | 9 | 28 |
| Intervention group | 40 | 24 | 16 | 43.5±17.3 | 10.99±11.48 | 3 | 8 | 29 |
| P-value | >0.05 | >0.05 | >0.05 | >0.05 | ||||
Comparison of the Psoriasis Area Severity Index (PASI), Self-Rating Anxiety Scale (SAS) and Dermatology Life Quality Index (DLQI) scores at baseline and at the end of follow-up between the two study groups
The Psoriasis Area Severity Index (PASI) score was used as the main index to evaluate the efficacy of treating psoriasis. The Self-Rating Anxiety Scale (SAS) was used to evaluate the subjective symptoms of psoriasis. The Dermatology Life Quality Index (DLQI) scale was used for the evaluation of the physical, psychological, and social health of the patients. In this study, there were no significant differences between the PASI, DLQI or SAS scores at baseline between the control group and the intervention group. However, at the end of 12 months of follow-up, the values of the PASI, DLQI and SAS scores of the intervention group were significantly lower than those of the control group, as shown in Table 2. This finding showed that interactive management between patients with psoriasis and physicians could result in improved treatment outcomes, and reduced the degree of anxiety, and improved the physical and mental health of patients.
Table 2.
Comparison of the Psoriasis Area Severity Index (PASI), the Self-Rating Anxiety Scale (SAS), and the Dermatology Life Quality Index (DLQI) scores at baseline and the end of follow-up between the two study groups.
| Group | n | PASI | SAS | DLQI | |||
|---|---|---|---|---|---|---|---|
| Baseline | End of follow-up | Baseline | End of follow-up | Baseline | End of follow-up | ||
| Control group | 39 | 25.64±10.83 | 25.01±11.77 | 11.97±6.21 | 10.99±5.78 | 43.77±6.81 | 42.88±5.96 |
| Intervention group | 40 | 24.92±9.86 | 10.38±5.76 | 12.43±4.74 | 4.53±3.44 | 42.83±5.97 | 25.03±4.34 |
| P-value | >0.05 | <0.05 | >0.05 | <0.05 | >0.05 | <0.05 | |
PASI – Psoriasis Area and Severity Index; SAS – Self-Rating Anxiety Scale; DLQI – Dermatology Life Quality Index.
Comparison of the results of a questionnaire on knowledge of psoriasis at the end of follow-up between the two study groups
A questionnaire survey was conducted to evaluate the degree of understanding of patients of their basic knowledge, their attitude towards treatment and the progress of psoriasis. As shown in Table 3, at the end of follow-up, patients in the intervention group showed a significantly better understanding of psoriasis compared with the control group. Specifically, when compared with the control group, patients in the intervention group had an improved understanding of the treatment of their psoriasis, which was likely to improve treatment compliance and to improve the relationship between patients and medical staff.
Table 3.
Comparison of the results of a questionnaire on knowledge of psoriasis at the end of follow-up between the two study groups.
| Question | Control group | Intervention group | ||||
|---|---|---|---|---|---|---|
| Right | Wrong | Accuracy (%) | Right | Wrong | Accuracy (%) | |
| Whether psoriasis is contagious or not? | 37 | 2 | 94.9 | 40 | 0 | 100 |
| Whether psoriasis is hereditary or not? | 26 | 13 | 66.7 | 39 | 1 | 97.5 |
| Do patients with psoriasis need to avoid certain food? | 8 | 31 | 20.5 | 38 | 2 | 95.0 |
| Can the psoriasis be cured? | 34 | 5 | 87.2 | 40 | 0 | 100 |
| Whether traditional Chinese medicines are safe and nontoxic or not? | 16 | 23 | 41.0 | 40 | 0 | 100 |
| Whether mental and emotional factors affect the disease or not? | 38 | 1 | 97.4 | 40 | 0 | 100 |
| Only drugs can treat psoriasis? | 19 | 20 | 48.7 | 40 | 0 | 100 |
| Do you believe in folk prescription or advertisement? | 23 | 16 | 59.0 | 39 | 1 | 97.5 |
| Are you aware of the hazards of anti-cancer drugs, hormones, immunosuppressive agents and heavy metal preparations? | 17 | 22 | 43.6 | 39 | 1 | 97.5 |
| Are there effective measures to prevent recurrence or exacerbation of psoriasis? | 32 | 7 | 82.1 | 40 | 0 | 100 |
| Are you eager to pursue the immediate effect? | 5 | 34 | 12.8 | 39 | 1 | 97.5 |
Comparison of the results of the Symptom Checklist-90-Revised (SCL-90-R) questionnaire at the end of follow-up between the two study groups
The nine domains of the scores of the Symptom Checklist-90-Revised (SCL-90-R) in the two study groups were analyzed. The results showed that there were significant differences between the two groups in the domains of somatization (SOM), depression (DEP), anxiety (ANX), hostility (HOS) and psychoticism (PSY). This finding showed that interactive management between patients with psoriasis and physicians could improve the mental health of patients with psoriasis and improve their quality of life, as shown in Table 4.
Table 4.
Comparison of the results of the Symptom Checklist-90-Revised (SCL-90-R) questionnaire survey at the end of follow-up between the two groups.
| Control group | Intervention group | P-value | |
|---|---|---|---|
| SOM | 16.09±4.43 | 9.22±3.22 | <0.05 |
| O-C | 13.86±3.01 | 11.43±5.57 | 0.264 |
| I-S | 14.55±4.21 | 10.27±3.39 | 0.422 |
| DEP | 27.50±5.44 | 21.53±4.42 | <0.05 |
| ANX | 24.37±4.29 | 15.28±3.27 | <0.05 |
| HOS | 12.69±3.66 | 7.28±3.37 | <0.05 |
| PHOB | 10.20±3.28 | 8.16±2.18 | 0.185 |
| PAR | 12.35±4.50 | 9.34±3.23 | 0.521 |
| PSY | 14.26±4.35 | 9.26±4.33 | <0.05 |
SOM – somatization; O-C – obsessive-compulsive behavior; I-S – interpersonal sensitivity; DEP – depression; ANX – anxiety; HOS – hostility; PHOB – phobic anxiety; PAR – paranoid ideation; PSY – psychoticism.
Discussion
As a chronic disease, psoriasis usually has a long duration and is influenced by physiological, psychological, and social factors [6]. In the course of clinical treatment, it can be difficult for physicians to accurately obtain long-term health data on patients with chronic diseases when patients are not hospitalized. As a result, the treatment of chronic disease, such as psoriasis, may not be timely and the cure rate remains low [12]. An increasingly recognized area of healthcare improvement is now directed to the management of patients in the community and includes patients diagnosis, self-management, and education about their disease.
Currently, the management of psoriasis in China relies mainly on outpatient treatment [16]. This traditional approach to the management of psoriasis often includes drug therapy, with patient information provided publicly and in the form of health brochures [17]. Physicians and nurses who work in departments of dermatology do not have enough time to explain to patients how to explain the management of psoriasis and to explain the effects of drug and topical treatments, which leads reduced patient compliance with prescribed medication, or inappropriately frequent patient appointments with their physician. Medical staff may be unaware when patients are using medication or preventive measures in the right way, which ultimately reduces the effectiveness of treatment. These factors can make patients with psoriasis dissatisfied with the treatment provided by their physician, reduces treatment compliance, may result in worsening of the disease, and adversely affect the mental and economic burden to the patient [18].
Currently, few hospitals in China have been able to apply the concept of drug therapy combined with whole-course health education to the prevention and treatment of psoriasis. Because psoriasis is a chronic disease that has psychological and physiological components, there is a view that it can only be managed effectively within the framework of a new medical model that also includes health education [19]. Health education based on multimedia technology is a modern and efficient method to improve the management of chronic disease. In the early 1970s, the United States began to use multimedia channels for chronic disease prevention and management and this approach is now widely used in clinical treatment [20]. In China, multimedia technology has also been commonly used in clinical practice and has been shown to achieve good results in diseases including diabetes, cancer, and acquired immune deficiency syndrome (AIDS) [21].
In this study, a cloud-based interactive patient and physician management platform for psoriasis was developed using multimedia technology. Through the establishment of the cloud-based platform, patients can acquire a comprehensive knowledge of psoriasis and can provide information on any clinical problems they have in a timely manner to the platform, and physicians use this platform to receive the patient information and provide medical advice. This controlled study included a 12-month follow-up period to evaluate the experience of the patients and physicians. The Psoriasis Area Severity Index (PASI), the Dermatology Life Quality Index (DLQI), and the Self-Rating Anxiety Scale (SAS) scores in the intervention group were found to be lower than those in the control group at the end of the study. Also, patients in the intervention group had a better understanding of the treatment for psoriasis, which could improve the patient and physician interaction. Also, the nine domains of the scores of the Symptom Checklist-90-Revised (SCL-90-R) were used to assess the two groups, which showed that interactive patient and physician management could improve the physical and mental health of patients with psoriasis and increase their quality of life.
In this pilot study, a cloud-based platform was created by professional software engineers to educate and manage patients with psoriasis in a single hospital, using a control group and an intervention group and a duration of 12 months. The results supported the feasibility and efficacy of cloud-based interactive patient and physician management with psoriasis. The main limitations of this study were that the study population was small and the study was conducted in a single center and is a single-center. Further large-scale multi-center studies are required to validate the findings from this study. Also, further studies with an increased patient follow-up time are needed.
Conclusions
For patients with psoriasis, the use of a cloud-based interactive patient and physician management platform improved the mental health and quality of life for patients with psoriasis and allowed patients to manage their disease more effectively and improved communication with their physicians.
Footnotes
Source of support: This study was supported by the Chinese Academy of Medical Sciences (2018PT33022), the PUMC Youth Fund, and the Fundamental Research Fund for the Central Universities (3332015078)
Conflict of interest
None.
References
- 1.Gulliver WP, Randell S, Gulliver S, et al. An investigation of comorbid disease and health service utilization among patients with moderate to severe psoriasis in Newfoundland and Labrador. J Cutan Med Surg. :2018. doi: 10.1177/1203475418791114. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 2.Gulliver WP, Randell S, Gulliver S, et al. Biologic therapy utilization in patients with moderate to severe psoriasis and psoriatic arthritis: an observational summary of biologic therapy use in a clinical setting. J Cutan Med Surg. 2018;22(6):567–76. doi: 10.1177/1203475418786712. [DOI] [PubMed] [Google Scholar]
- 3.Guo P, Luo Y, Mai G, et al. Gene expression profile-based classification models of psoriasis. Genomics. 2014;103:48–55. doi: 10.1016/j.ygeno.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Amin M, Lee EB, Bhutani T, Wu JJ. Review of European registries for psoriasis. J Dermatolog Treat. 2018;14:1–10. doi: 10.1080/09546634.2018.1506084. [DOI] [PubMed] [Google Scholar]
- 5.Snast I, Reiter O, Atzmony L, et al. Psychological stress and psoriasis: A systematic review and meta-analysis. Br J Dermatol. 2018;178:1044–55. doi: 10.1111/bjd.16116. [DOI] [PubMed] [Google Scholar]
- 6.Young H. Psychological effects of skin disease: the psoriasis exemplar. Br J Nurs. 2017;26:590–91. doi: 10.12968/bjon.2017.26.11.590. [DOI] [PubMed] [Google Scholar]
- 7.Qian M, Song NJ. Serum calprotectin correlates with risk and disease severity in psoriasis patients and the decrease of calprotectin predicts better response to tumor necrosis factor inhibitors. Eur Rev Med Pharmacol Sci. 2018;22:4299–309. doi: 10.26355/eurrev_201807_15426. [DOI] [PubMed] [Google Scholar]
- 8.Ersser SJ, Cowdell FC, Latter SM, Healy E. Self-management experiences in adults with mild-moderate psoriasis: an exploratory study and implications for improved support. Br J Dermatol. 2010;163:1044–49. doi: 10.1111/j.1365-2133.2010.09916.x. [DOI] [PubMed] [Google Scholar]
- 9.Sahlabadi A, Chandren MR, Sahlabadi M, Golshanbafghy H. Framework for parallel preprocessing of microarray data using hadoop. Adv Bioinformatics. 2018;2018 doi: 10.1155/2018/9391635. 9391635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adler AJ, Martin N, Mariani J, et al. Mobile phone text messaging to improve medication adherence in secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2017;4:CD011851. doi: 10.1002/14651858.CD011851.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mohamadirizi S, Shaygannejad V, Mohamadirizi S, Khosrawi S. The effect of electronic package on satisfaction in multiple sclerosis patients. Adv Biomed Res. 2016;5:89. doi: 10.4103/2277-9175.183143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Otero ME, van Geel MJ, Hendriks JC, et al. A pilot study on the Psoriasis Area and Severity Index (PASI) for small areas: Presentation and implications of the Low PASI score. J Dermatolog Treat. 2015;26:314–17. doi: 10.3109/09546634.2014.972316. [DOI] [PubMed] [Google Scholar]
- 13.Rencz F, Gulacsi L, Pentek M, et al. Proposal of a new scoring formula for the DLQI in psoriasis. Br J Dermatol. 2018;310:47–55. doi: 10.1111/bjd.16927. [DOI] [PubMed] [Google Scholar]
- 14.Lu CJ, Xiang Y, Xie XL, et al. A randomized controlled single-blind clinical trial on 84 outpatients with psoriasis vulgaris by auricular therapy combined with optimized Yinxieling Formula. Chin J Integr Med. 2012;18:186–91. doi: 10.1007/s11655-012-1020-3. [DOI] [PubMed] [Google Scholar]
- 15.Li P, Wang F, Ji GZ, et al. The psychological results of 438 patients with persisting GERD symptoms by Symptom Checklist 90-Revised (SCL-90-R) questionnaire. Medicine (Baltimore) 2018;97:e9783. doi: 10.1097/MD.0000000000009783. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 16.Baroni A, Ruocco E, Russo T, et al. The use of traditional Chinese medicine in some dermatologic diseases: Part I – Acne, psoriasis, and atopic dermatitis. Skinmed. 2015;13(1):32–38. [PubMed] [Google Scholar]
- 17.Marchesoni A, Lubrano E, Cauli A, et al. Psoriatic disease: Update on traditional disease-modifying antirheumatic drugs. J Rheumatol Suppl. 2015;93:61–64. doi: 10.3899/jrheum.150639. [DOI] [PubMed] [Google Scholar]
- 18.Legat FJ. [Importance of phototherapy in the treatment of chronic pruritus]. Hautarzt. 2018 doi: 10.1007/s00105-018-4229-z. [Epub ahead of print] [in German] [DOI] [PubMed] [Google Scholar]
- 19.Ding X, Wang T, Shen Y, et al. Prevalence of psoriasis in China: A population-based study in six cities. Eur J Dermatol. 2012;22:663–67. doi: 10.1684/ejd.2012.1802. [DOI] [PubMed] [Google Scholar]
- 20.Lamont S, Brunero S. ‘eSimulation’ part 1: Development of an interactive multimedia mental health education program for generalist nurses. Collegian. 2013;20:239–47. doi: 10.1016/j.colegn.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 21.Gan ZK, Jin H, Li JX, et al. Disease burden of enterovirus 71 in rural central China: A community-based survey. Hum Vaccin Immunother. 2015;11:2400–5. doi: 10.1080/21645515.2015.1059980. [DOI] [PMC free article] [PubMed] [Google Scholar]


