Figure 1. Simplified Schematic of Mineral and Bone Disorder (MBD) Physiology in Chronic Kidney Disease.
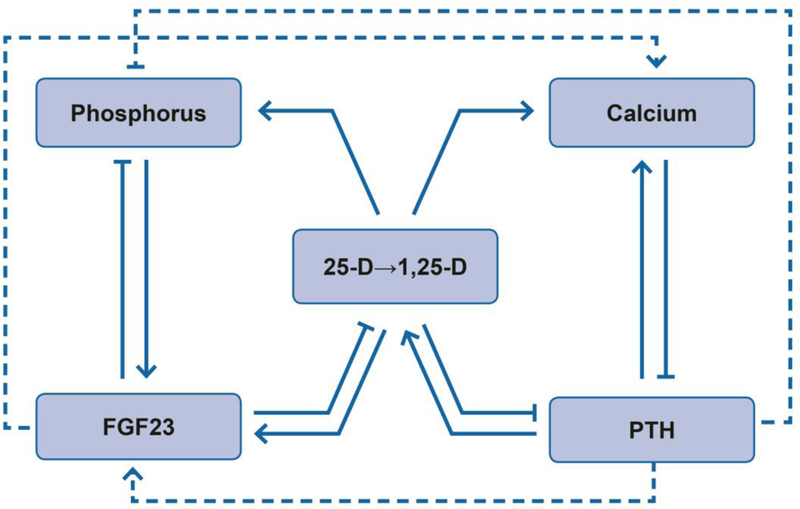
Solid lines and arrows depict dominant physiologic effects on circulating MBD factors including: (1) effects of fibroblast growth factor 23 (FGF23) to lower serum phosphorus by inhibiting 1α-hydroxylase that converts 25-hydroxyvitamin D (25-D) to 1,25-dihydroxyvitamin D (1,25-D) and stimulating urinary phosphorus excretion; (2) effects of parathyroid hormone (PTH) to raise serum calcium by stimulating 1α-hydroxylase and increasing urinary calcium reabsorption and bone remodeling; (3) effects of vitamin D to promote gastrointestinal absorption of calcium and phosphorus and feedback on FGF23 (stimulation) and PTH (inhibition). Dashed lines and arrows depict additional non-dominant effects of FGF23 to increase urinary calcium reabsorption and PTH to increase urinary phosphorus excretion and FGF23 transcription. In each case, arrows (→) represent actions that raise the associated MBD factor whereas capped lines (┤) represent actions that lower the associated MBD factor. Altogether, the physiology encompasses major effects of FGF23 to reduce phosphorus and vitamin D and major effects of PTH to increase calcium and vitamin D, along with substantial redundancy, feedback, and crosstalk.
