Abstract
BACKGROUND:
Objective measures of adherence to high-frequency chest wall compression (HFCWC), a form of airway clearance therapy for patients with cystic fibrosis, are lacking. We used a novel electronic monitoring device integrated into an HFCWC vest to measure adherence compared with self-reported adherence. We determined factors that influenced adherence and how adherence correlated with baseline pulmonary function and pulmonary exacerbations.
METHODS:
Data were collected by direct measurement of date, time of day, and duration of HFCWC use to determine the number of daily treatments and daily duration of treatments. Chart review provided prescribed airway clearance therapy treatment and demographic and clinical information. Subject and caregiver report of the daily number of airway clearance therapy treatments was obtained by telephone interviews. Analysis used 2-sample and paired t test, analysis of variance, and linear regression.
RESULTS:
Average adherence was 69%. Adherence was highest in children (82%, P = .02) and those receiving assistance with treatment (82%, P < .001). Subjects overestimated therapy duration from a mean ± SD of 127 ± 169% by adults to 19.2 ± 26.3% by parents or guardians of children. Average adherence decreased with increasing prescribed therapy time (P = .02). Average daily therapy time and adherence had significant positive associations with baseline FEV1 percent of predicted (P = .02 and P = .02, respectively) and negative associations with pulmonary exacerbations during the pre-study period and at baseline (P = .044 and P = .02, respectively).
CONCLUSIONS:
Greater adherence to HFCWC measured directly by a novel recorder was associated with better baseline pulmonary function and fewer exacerbations in the pre-study and baseline period. Adherence decreased with age and prescribed therapy time and increased with therapy assistance. Self-report overestimation is large and thus not an accurate measure of adherence.
Keywords: adherence, cystic fibrosis, high-frequency chest wall compression, pulmonary function test, pulmonary exacerbation
Introduction
Approximately 80% of deaths in patients with cystic fibrosis (CF) stem from respiratory insufficiency (about 67%) or from complications of lung transplantation (about 13%).1 Impaired mucociliary clearance predisposes patients to recurrent infection, mucus plugging, inflammation, and airway obstruction that ultimately leads to progressive loss of lung function.2 A growing number of inhaled and oral medications are available to counteract this process. In addition to drug treatments, the Cystic Fibrosis Foundation also recommends regular performance of airway clearance therapy employing one of several techniques.3
Advances in treatment have substantially improved survival over the past 3 decades,1 but there is evidence that poor adherence prevents patients from fully realizing the benefits of CF therapies.4–6 Relatively little is known about predictors of non-adherence in patients with CF, but duration and complexity of the regimen are likely to be negatively related to adherence.7,8 Previous studies also indicate that non-adherence is particularly prevalent during weekends and summer months in school-age patients9 as well as among adolescents at any time.4,5 Family functioning as well as depression among children and their parents are additional important determinants of adherence.8,10,11 Even with the advent of CF transmembrane conductance regulator gene correctors and potentiators, consistent use of airway clearance therapy remains paramount for preserving lung function because these novel medications are unlikely to reverse established bronchiectasis.
Prior studies of airway clearance therapy adherence in subjects with CF commonly employ patient self-report to measure adherence, but this approach consistently yields higher levels of adherence than objective measures. For instance, Daniels et al12 compared adherence to prescribed nebulizer therapies in subjects with CF measured by self-report versus electronic monitoring, and found adherence rates of 80 and 36%, respectively. Published studies that have focused specifically on adherence to airway clearance therapy among subjects with CF have relied primarily on patient, parent, and clinician surveys, with self-reported adherence in the past decade ranging from 14 to 94%.13–16 Actual adherence to airway clearance therapy remains unknown due to the lack of studies with objective electronic monitoring of airway clearance therapy adherence.
Our study compared objectively measured adherence to airway clearance therapy with patient- and parent-reported adherence among children, adolescents, and young adults with CF. We employed a novel electronic monitoring device that recorded the daily timing and duration of patient use of a high-frequency chest wall compression (HFCWC) device. Based on our above review of the literature and our clinical experience, we hypothesized that: (1) objectively measured adherence is lower than self-reported adherence; (2) adherence is lower among adolescents and young adults than children; (3) adherence decreases as prescribed duration of therapy increases; (4) patients who live with a parent or guardian or receive assistance with therapy are more adherent; and (5) patients with recent exacerbations and lower baseline FEV1 are more likely to have lower adherence.
QUICK LOOK.
Current knowledge
A majority of deaths from cystic fibrosis stem from respiratory insufficiency. Advances in treatment have substantially improved survival for this disease over the past 3 decades. Regular performance of airway clearance therapy is recommended for these patients; however, adherence is regarded as poor based largely on subjective data.
What this paper contributes to our knowledge
We used a novel electronic chronometer and data recorder integrated into a high frequency chest wall compression device to objectively measure daily duration of use. Children with caregivers who assisted with starting therapy had the highest adherence, and adults had the lowest. Neither electronic monitoring nor monthly technician visits affected adherence. Higher baseline FEV1 (percent of predicted) and absence of recent pulmonary exacerbation were associated with better adherence.
Methods
Subjects
Subjects age 6–24 y treated at the University of Minnesota Cystic Fibrosis Center were enrolled. CF was confirmed with a sweat chloride concentration >60 mmol/L using Gibson-Cooke pilocarpine iontophoresis.17 To be included, subjects had a current prescription for HFCWC for their airway clearance technique, had HFCWC equipment (the Vest System, Hill-Rom, Batesville, Indiana), were able to perform valid spirometry, and lived in the region of Minnesota, eastern North and South Dakota, northern Iowa, and western Wisconsin. We excluded those who were in hospice care, did not have 1 y of Minnesota CF center records, or had not been seen for >1 y. Subjects <13 y of age were placed into the childhood cohort, those 13–18 y of age were placed into the adolescent cohort, and those ≥19 y of age were placed into the adult cohort.
Subjects who consented for the study but were diagnosed with a pulmonary exacerbation within 2 weeks of enrollment or who had more than one exacerbation in the preceding 6 months were placed in a pulmonary exacerbation group. A generally accepted definition of a pulmonary exacerbation of CF lung disease based on signs and symptoms that was applicable to children and adults and to our available dataset was not available.18 We used a working definition for this study. To be most inclusive, a pulmonary exacerbation was defined as symptoms of a respiratory infection (any one or more of increased cough, increased sputum production, new crackles, new wheeze, new hemoptysis) that resulted in prescribing a new antibiotic and an increase in inhaled medications and airway clearance therapy with or without evidence of a decline in pulmonary function or hospitalization by patient report and chart review. This working definition is most similar to the definition found by Rabin et al19 in analysis of the Epidemiologic Study of Cystic Fibrosis data set to correlate with medical caregiver diagnosis and antibiotic treatment of pulmonary exacerbation and that found by Byrnes et al20, in their analysis of the Australasian CF BronchoAlveolar Lavage randomized controlled trial data set, to correlate with family or physician diagnosis of pulmonary exacerbation.21
Study Design
The Vest System model 105 (Hill-Rom) equipped with a novel data recorder was used for the study. All subjects who were using another model of the Vest System were provided with a model 105 device with a data recorder. Patients and their parents or guardians were approached for the study, and consent (or assent with parent/guardian's consent for those <18 y old) was obtained by the principal investigator or one of the study staff, not the patient's medical care providers or Hill-Rom. Study personnel did not alter medications, treatment plans, or other CF therapies.
The institutional review board at the University of Minnesota approved this study. After informed consent and enrollment, a questionnaire was filled out by telephone interview performed by study staff. The subjects and the parents/guardians of subjects <18 y of age were asked: “How many times a day are you prescribed to do chest therapy?”; “How many minutes is each session prescribed to be?”; “Have you been on antibiotics for a pulmonary exacerbation in the last 2 months?”; “Are you currently living with a parent or guardian?”; and “Does your parent/guardian assist you with starting your chest therapy?” (only for subjects <18 y old). Hill-Rom technicians were required to visit the home to set up the data recorders and download the data at set intervals. Technician visits occurred as close as possible to 30, 60, and 90 d after the initial home visit to establish 3 30-d observation blocks. At each visit, data were downloaded from the recorders, and if the subject was ≥18 y old, he or she was asked, “How many chest therapy treatments did you do in the last 2 weeks?” If the subject was <18 y old, the parent/guardian was asked, “How many chest therapy treatments did your child do in the last 2 weeks?” Each chest therapy treatment reported was assumed to be the prescribed 30-min session. Downloaded data and visit forms were sent electronically to the principal investigator (CM).
HFCWC Recorder Information
At the Minnesota Cystic Fibrosis Center, patients are routinely prescribed twice daily HFCWC sessions that are 30 min in duration and consist of 6 different oscillation frequencies of 5-min duration each. HFCWC therapy data were recorded as the total time the system was turned on (in min) during each session, and the total number of sessions. Sessions with pauses >1 h were considered 2 separate sessions. All sessions were included unless they lasted <5 min or >60 min, since it was unlikely that a subject was actually participating in a session lasting >1 h.
A recording device, integrated into each subject's HFCWC device, was turned on at the start of the study. Date; clock time of start, stops, and pauses of high frequency compressions; the compression frequency setting (in Hz); and compression pressure intensity setting (1–10) were recorded. If the subject made any key press changes to the settings of frequency, pressure (intensity), and time, this also resulted in a recorded event. The recording devices had a maximum storage capacity of 1,024 events or approximately 60 d. If the maximum number of events were reached, the first event from the beginning of the recording period would be overwritten, and each sequential entry would be overwritten as the number of events beyond the maximum increased. Data were downloaded approximately every 30 d during a home visit by the technical staff.
The first day of the block in which data were available was used as day 1. This approach was used for all 3 30-d blocks. If a subject was hospitalized during the study period, these days were removed, because they would otherwise appear as days of no therapy. The data for each 30-d block were then separated into 4 equal quarters. Adherence during the different quarters was compared to assess the influence of an upcoming monitoring visit on adherence.
Clinical Data
Baseline demographics were obtained by chart review. Spirometry met American Thoracic Society/European Respiratory Society validity criteria,22 and FEV1 percent of predicted was derived from the National Health and Nutrition Examination Survey III.23 Pancreatic insufficiency was considered present if pancreatic enzyme replacement were prescribed. If the HFCWC prescription was not explicitly charted in a visit note, the standard Minnesota Cystic Fibrosis Center prescription of 30 min twice daily was used, since this is the default prescription that our respiratory therapists provide in their airway clearance therapy instructions to patients.
Statistical Analysis
Descriptive statistics were computed for demographic attributes (Table 1). Average daily therapy time was calculated directly from the daily measured data averaged over each 30-d interval. Adherence was measured as the measured average daily therapy time as a percentage of the prescribed daily therapy time. This definition was in accord with the World Health Organization initiative on adherence to long-term therapies.24 Mean percentage overestimation of performed therapy was calculated as the subject- or parent/guardian-reported duration of airway clearance therapy during these 2 weeks minus the actual duration of airway clearance therapy during these 2 weeks, which was then divided by this actual duration of airway clearance therapy during these 2 weeks and multiplied by 100. The last 2 weeks of data from each block were used to calculate the mean percent overestimation of performed therapy.
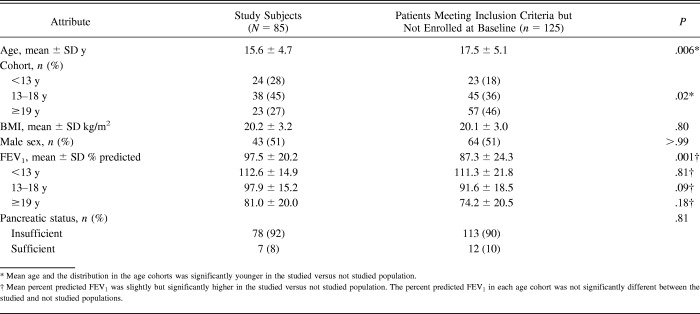
Table 1.
Comparative Demographics
To assess whether adherence decreased over the study period, adherences for blocks 1 and 3 were paired for each subject and analyzed by paired t test. The same analysis was used to evaluate the influence of anticipating technician visits by comparing adherence in quarters 2 and 4 of each block, again analyzed by paired comparison for each subject.
The influences of (1) assistance with therapy and (2) living with a parent for those <18 y old were examined using a 2-sample t test. Average adherences and mean percent overestimation were stratified first by prescription and then for age cohort and evaluated by analysis of variance, with follow-up pairwise comparisons using Tukey's standardized range method.
Average daily therapy time as a correlate of baseline FEV1 percent of predicted was assessed by linear regression. The adherence, therapy time, and FEV1 percent of predicted of subjects experiencing a pulmonary exacerbation in the baseline period to those not experiencing a pulmonary exacerbation was compared by 2-sample t test. All analyses were performed with SAS 9.2 (SAS Institute, Cary, North Carolina) and R software 3.3.2.25
Results
Comparative Demographics
Of 210 patients meeting inclusion criteria, 125 remained after exclusion criteria were applied. Of these 125, 104 consented; of these 104, 19 withdrew, leaving 85 studied subjects (Table 1). Patients who met inclusion criteria but were not enrolled consisted of 85 patients who met only inclusion criteria, 21 who did not consent to be studied, and 19 who withdrew between enrollment and the study start (n = 125). The studied subjects with CF had a greater proportion of younger individuals, and the average FEV1 percent of predicted was higher than for those who were not studied. The difference in mean FEV1 percent of predicted between each age group in the studied sample versus those not studied was small and ranged from 1.3 percent of predicted (between the <13-y-old age groups) to 6.8 percent of predicted (between the ≥19-y-old age groups).
Objectively Measured Therapy Time, Adherence, Overestimation of Performed Therapy, and Effect of Technician Visits
Ten subjects had default prescriptions for airway clearance therapy used because prescriptions were not available in the visit charts. Only 2 discrepancies between physician- and subject-reported prescriptions were found. One subject believed they were to do 30 min less/d and the other 30 min more.
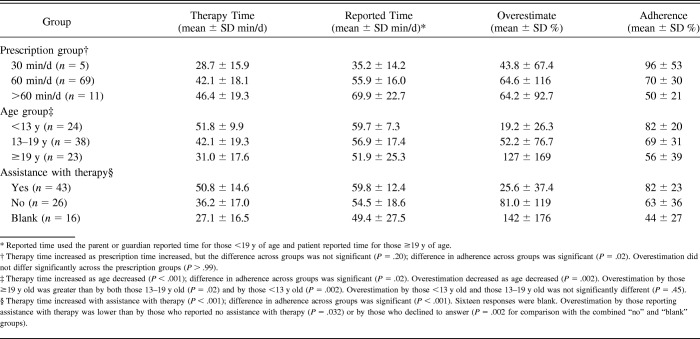
The average ± SD therapy time was 41.8 ± 18.3 min/d (range 4.9–87.2 min/d), and the average ± SD adherence to airway clearance therapy was 69 ± 32% (range 8–175%). Adult subjects overestimated the minutes of daily airway clearance therapy they performed in the prior 2 weeks by a mean of 127% with large variability (SD = 169%) (Table 2). Parents or guardians of teens overestimated the amount of daily airway clearance therapy performed by 52.2 ± 76.7%, and parents or guardians of pre-teens overestimated the amount of daily airway clearance therapy performed by 19.2 ± 26.3%. Comparisons between the age groups were statistically different comparing the adult versus the teen and the adult versus the pre-teen groups (P = .02 and P = .002, respectively). Where subject and parent or guardian both reported, overestimation did not differ significantly (P = .33). Parents or guardians who reported that they assisted with starting HFCWC therapy overestimated the daily amount of airway clearance therapy by 25.6 ± 37.4%, which was significantly less than in those who reported no assistance (81 ± 119%, P = .032) or declined to answer (P = .002 for comparison with the combined “no” and “blank” groups).
Table 2.
Predictors of Therapy Time, Reported Time, Overestimation, and Adherence
No monitoring effect was seen. The adherence did not change significantly over the 3 30-d observation blocks with adherence in blocks 1, 2, and 3 being 71, 70, and 69%, respectively (SD = 34, 33, and 32%, respectively). Adherence across quarters within each 30-d block did not differ. Average ± SD adherence per quarter of all 30-d blocks was 70 ± 32% during quarter 1, 69 ± 34% during quarter 2, 69 ± 34% during quarter 3, and 69 ± 32% during quarter 4. The difference between quarter 2 and quarter 4 adherence, testing the effect of anticipation of a technician visit, was not significant (P = .92).
Objectively Measured Adherence Was Lower Among Adults Than Children
Children had the longest average daily therapy time of 51.8 min/d and had the highest adherence of 82% (Table 2). The adolescent and adult cohorts performed on average 42.1 and 31.0 min/d of therapy time, respectively, and had an adherence of 69 and 56%, respectively. The difference among these 3 age groups was significant (P = .02). Pairwise comparison by Tukey's test showed a significant difference between the children and adults (difference between means = 26% and 95% CI = 5–47%).
Longer Duration of Prescribed Therapy Correlated With Lower Adherence
Subjects showed a slight but insignificant increase in therapy time as the prescribed time increased (Table 2). Adherence decreased significantly as prescribed therapy time increased.
Subjects Who Received Assistance With Therapy Were More Adherent
Assistance with starting therapy was associated with significantly higher adherence; those who reported parental/guardian assistance had an 82% mean adherence compared with 63% among those who did not (Table 2). Living with one's parents or guardians was not associated with increased adherence (75 ± 26% vs 60 ± 46%, P = .25).
Lower Baseline Lung Function Correlated With Lower Adherence
We used FEV1 percent of predicted as a measure of airflow adjusted for growth. This allowed us to compare airflow across our subjects of different ages and sizes. FEV1 percent of predicted at entry into the study was positively correlated with therapy time (P = .02) and adherence (P = .02) observed during the study.
Subjects who experienced pulmonary exacerbation shortly before or within 2 weeks of study enrollment were less adherent
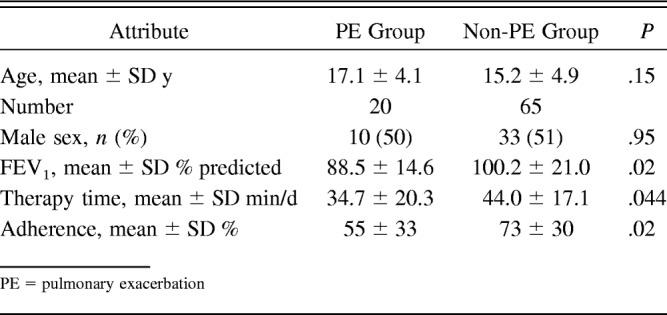
Comparisons between the pulmonary exacerbation and non-pulmonary exacerbation groups are provided in Table 3. Subjects who received antibiotics for more than one pulmonary exacerbation in the 6 months before or had one pulmonary exacerbation within 2 weeks of study enrollment were significantly less adherent during the study period than those who did not. As expected, mean FEV1 percent of predicted was significantly lower in the pulmonary exacerbation group compared with the non-pulmonary exacerbation group.
Table 3.
Comparison of Pulmonary Exacerbation and Non-Pulmonary Exacerbation Groups
Discussion
We used a new electronic event-monitoring system integrated into an HFCWC device prescribed for airway clearance therapy in subjects with CF to objectively measure adherence. Unlike medications, including those delivered by metered-dose inhalation, airway clearance therapy is time-consuming. At our CF center, the standard prescription is for 2 30-min therapy sessions daily when the patient is well and up to 4 times daily when he or she has increased cough, wheeze, sputum production, or shortness of breath. In studies using self-reporting, adherence to airway clearance therapy is between 14 and 94%.13,14,15,16 As expected from studies using medication event-monitoring systems, we found that parents and subjects overestimated time spent using the HFCWC from about 20 to 127%, respectively, using 2-week recall. Interestingly, the group of parents or guardians who reported that they assisted with starting HFCWC therapy had a significantly more accurate and precise estimate of the therapy time measured in the prior 2 weeks than those who did not report assisting or did not respond to this question.
Our subjects showed a mean 69% adherence to airway clearance therapy by the event-monitoring system. This was at the higher end of the range previously documented from self-report. The younger age of our study population and the assistance of parents or caregivers in the therapy may account for this because the maximum adherence was found in those <13 y of age. This is consistent with studies of subjects with asthma who showed lower adherence using medication event-monitoring systems in adolescents and adults compared with children.26 Our study showed that high adherence (82%) was associated with the assistance of parents or guardians with the airway clearance therapy of younger subjects. This is consistent with the findings using electronic monitoring of nebulizer adherence of subjects with CF.27 Strategies to address the drop-off in adherence between childhood and adolescence include behavior-, education-, and technology-based interventions.28 Electronic monitoring devices may prove useful for patients interested in tracking their own adherence and also offer objective measures of adherence in intervention trials.
Based on prior studies, we expected to see a Hawthorne effect, with increased adherence as the time of a study technician visit approached.29 Interestingly, we found no increase in adherence in the days before such a visit, although the subjects knew when the visit was scheduled and that monitoring their airway clearance therapy was the purpose of the study. One possible explanation is that this effect has generally been shown with relatively simple and short-duration interventions, such as handwashing. Airway clearance therapy with the HFCWC is relatively complex, and each treatment is of long duration, usually 30 min. Such interventions may be less influenced by awareness of once-monthly direct human observation. The electronic monitoring system we used on this HFCWC device performed like the electronic monitoring system of handwashing,29 and its use alone simply did not have a large impact on adherence, although the subjects in both of these studies knew that they were being electronically monitored. Alternatively, the subjects and families knew at enrollment that they would be monitored and so may have been at their maximum adherence at the study start, and any additional effect of electronic monitoring or the approaching time of a technician visit was attenuated. However, we found no decrease in adherence over the 3 months of our study period. This is most likely consistent with the subjects being at their routine adherence level during the study period.
Subjects with lower baseline FEV1 percent of predicted and subjects who experienced an antibiotic-treated pulmonary exacerbation had lower adherence during the study period than those who had higher FEV1 percent of predicted and were exacerbation-free. This is consistent with the hypothesis that those who were more adherent had less airway inflammation and obstruction and that the adherence during the study period was similar to adherence before this study period. However, our study does not prove a causal link between reduced adherence to therapy and exacerbation risk. For instance, it is also possible that worsening respiratory status acutely reduced adherence early in the study in the subset of subjects subsequently diagnosed with an exacerbation. The lack of change in adherence in subjects over the 3-month study period makes this possibility less likely.
Our study has several limitations. The studied subjects were self-selected. However, the baseline demographics of those studied and of those who were not were similar when adjusted for age. This suggests that our results were fairly representative of our patients with CF in each age group. The families knew that they were being monitored. This may have contributed to the higher adherence to airway clearance therapy that we observed. However, we found no effect of anticipation of technician visits on adherence nor difference in adherence during the first month of the study compared with the last month, suggesting that the subjects were in their routine adherence mode. The subjects, parents, or guardians could run the HFCWC device without having it on the subject. However, the continuous clock function recorded the time each day when the device was turned on and off and the duration in each of these modes. Most subjects were turning their HFCWC device on 2–4 times daily, with each “on” period alternating with significant “off” time. This is most consistent with, but does not guarantee, actual use of the HFCWC device on each subject. Previously available monitors simply kept a running total of therapy time. A subject could turn on his or her equipment for multiple hours without actually doing therapy. This “dumping” behavior has been seen in many studies using objective monitoring devices, such as pill and metered-dose inhaler counters.30,31 In addition to the date, time, and total duration of each session, the current monitoring device also recorded frequencies, pressures, and pauses used during each session. The subjects were varying frequencies and pausing between frequencies, and many were doing so as prescribed. This pattern is also consistent with use of the device on the subject. Electronic monitoring devices can fail, but we found no failures of devices used in this study over the 3-month observation periods. Finally, adherence to the HFCWC used in our study may not apply to other modes of airway clearance therapy.
A strength of this study was the long observation time in the home setting. This minimized the effect of short-term and clinic-related behavior changes, making accurate measurement of routine adherence more likely. More typical adherence behavior was also more likely to be seen because our study made minimal interventions and required no alterations to the subject's standard CF care.
We conclude from this study that objectively measured adherence to HFCWC airway clearance was lower than self-reported adherence; that adherence was lower among adolescents and young adults than among children; that adherence decreased as prescribed duration of therapy increased; and that subjects who received assistance with starting therapy were more adherent, but monthly, in-home technician visits had no measurable impact on adherence. Subjects with recent exacerbations and lower baseline FEV1 were more likely to have lower adherence. The electronic measuring device was reliable over at least a 3-month period. A prospective, comparative study of the effect on adherence of active assistance is needed to test the relative usefulness of such interventions to improve adherence, especially among adolescents and adults. The objective data that this novel monitoring device provides are useful in assessing adherence to airway clearance therapy, but further study is needed to determine whether this information can be used to improve adherence.
Acknowledgment
We thank Lisa Henn PhD for statistical assistance, Ann Hazelwood CRT and Cynthia Williams CCRC for assistance in recruitment, and Marilyn Joseph MD for review of the manuscript.
Footnotes
This study was supported in part by grants from the Cystic Fibrosis Foundation and from Hill-Rom, which also provided equipment and assistance in data collection. Dr Laguna has disclosed relationships with the National Institutes of Health, the Cystic Fibrosis Foundation, the Robert Wood Johnson Foundation, the Minnesota Medical Foundation, and Cayston Pharmaceuticals. The other authors have disclosed no conflicts of interest.
Dr Mikesell presented versions of this work at the 2010 and 2011 North American Cystic Fibrosis Conferences, held October 21–23, 2010, in Baltimore, Maryland, and November 3–5, 2011, in Anaheim, California, and at the 2011 American Thoracic Society Conference, held May 13–18, 2011, in Denver, Colorado.
Reference
- 1. Marshall BC. Cystic Fibrosis Foundation Patient Registry: 2013. Annual Data Report. https://www.cff.org/2013_CFF_Patient_Registry_Annual_Data_Report.pdf Accessed February 23, 2017.
- 2. Schechter MS. Airway clearance applications in infants and children. Respir Care 2007;52(10):1382–1390; discussion 1390-1391. [PubMed] [Google Scholar]
- 3. Flume PA, Robinson KA, O'Sullivan BP, Finder JD, Vender RL, Willey-Courand DB, et al. Cystic fibrosis pulmonary guidelines: airway clearance therapies. Respir Care 2009;54(4):522–537. [PubMed] [Google Scholar]
- 4. Eakin MN, Bilderback A, Boyle MP, Mogayzel PJ, Riekert KA. Longitudinal association between medication adherence and lung health in people with cystic fibrosis. J Cystic Fibrosis 2011;10(4):258–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nasr SZ, Chou W, Villa KF, Chang E, Broder MS. Adherence to dornase α treatment among commercially insured patients with cystic fibrosis. J Med Econ 2013;16(6):801–808. [DOI] [PubMed] [Google Scholar]
- 6. Briesacher BA, Quittner AL, Saiman L, Sacco P, Fouayzi H, Quittell LM. Adherence with tobramycin inhaled solution and health care utilization. BMC Pulm Med 2011;11(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sawicki GS, Sellers DE, Robinson WM. High treatment burden in adults with cystic fibrosis: challenges to disease self-management. J Cystic Fibrosis 2009;8(2):91–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kettler LJ, Sawyer SM, Winefield HR, Greville HW. Determinants of adherence in adults with cystic fibrosis. Thorax 2002;57(5):459–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ball R, Southern KW, McCormack P, Duff AJ, Brownlee KG, McNamara PS. Adherence to nebulised therapies in adolescents with cystic fibrosis is best on week-days during school term-time. J Cystic Fibrosis 2013;12(5):440–444. [DOI] [PubMed] [Google Scholar]
- 10. Barker DH, Quittner AL. Parental depression and pancreatic enzymes adherence in children with cystic fibrosis. Pediatrics 2016;137(2):1–9. 10.1542/peds.2015-2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Smith BA, Modi AC, Quittner AL, Wood BL. Depressive symptoms in children with cystic fibrosis and parents and its effects on adherence to airway clearance. Pediatric Pulmonol 2010;45(8):756–763. [DOI] [PubMed] [Google Scholar]
- 12. Daniels T, Goodacre L, Sutton C, Pollard K, Conway S, Peckham D. Accurate assessment of adherence: self-report and clinician report vs electronic monitoring of nebulizers. Chest 2011;140(2):425–432. [DOI] [PubMed] [Google Scholar]
- 13. Arias Llorente RP, Bousoño García C, Díaz Martín JJ. Treatment compliance in children and adults with cystic fibrosis. J Cystic Fibrosis 2008;7(5):359–367. [DOI] [PubMed] [Google Scholar]
- 14. Myers LB, Horn SA. Adherence to chest physiotherapy in adults with cystic fibrosis. J Health Psychol 2006;11(6):915–926. [DOI] [PubMed] [Google Scholar]
- 15. Modi AC, Cassedy AE, Quittner AL, Accurso F, Sontag M, Koenig JM, Ittenbach RF. Trajectories of adherence to airway clearance therapy for patients with cystic fibrosis. J Pediatr Psychol 2010;35(9):1028–37. [DOI] [PubMed] [Google Scholar]
- 16. McIlwaine MP, Alarie N, Davidson GF, Lands LC, Ratjen F, Milner R, et al. Long-term multicentre randomised controlled study of high frequency chest wall oscillation versus positive expiratory pressure mask in cystic fibrosis. Thorax 2013;68(8):746–751. [DOI] [PubMed] [Google Scholar]
- 17. Rosenstein BJ, Cutting GR. The diagnosis of cystic fibrosis: a consensus statement. J Pediatr 1998;132(4):589–595. [DOI] [PubMed] [Google Scholar]
- 18. Flume PA, Mogayzel PJ, Jr, Robinson KA, Goss CH, Rosenblatt RL, Kuhn RJ, et al. Cystic fibrosis pulmonary guidelines: treatment of pulmonary exacerbations. American journal of respiratory and critical care medicine 2009;180(9):802–808. [DOI] [PubMed] [Google Scholar]
- 19. Rabin HR, Butler SM, Wohl ME, Geller DE, Colin AA, Schidlow DV, et al. Pulmonary exacerbations in cystic fibrosis. Pediatr Pulmonol 2004;37(5):400–406. [DOI] [PubMed] [Google Scholar]
- 20. Byrnes CA, Vidmar S, Cheney JL, Carlin JB, Armstrong DS, Cooper PJ, et al. Prospective evaluation of respiratory exacerbations in children with cystic fibrosis from newborn screening to 5 years of age. Thorax 2013;68(7):643–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Waters V, Ratjen F. Pulmonary exacerbations in children with cystic fibrosis. Ann Am Thorac Soc 2015;12(Suppl 2):S200–S206. [DOI] [PubMed] [Google Scholar]
- 22. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J 2005;26(2):319–338. [DOI] [PubMed] [Google Scholar]
- 23. Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general US population. Am J Respir Crit Care Med 1999;159(1):179–87. [DOI] [PubMed] [Google Scholar]
- 24. Sabaté E. Adherence to long-term therapies: evidence for action. World Health Organization; 2003. http://apps.who.int/iris/bitstream/10665/42682/1/9241545992.pdf Accessed February 23, 2017. [Google Scholar]
- 25. R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria: 2016. https://www.R-project.org Accessed February 23, 2017. [Google Scholar]
- 26. Bender B, Wamboldt FS, O'Connor SL, Rand C, Szefler S, Milgrom H, Wamboldt MZ. Measurement of children's asthma medication adherence by self report, mother report, canister weight, and Doser CT. Ann Allergy Asthma Immunol 2000;85(5):416–421. [DOI] [PubMed] [Google Scholar]
- 27. Modi AC, Marciel KK, Slater SK, Drotar D, Quittner AL. The influence of parental supervision on medical adherence in adolescents with cystic fibrosis: developmental shifts from pre to late adolescence. Child Health Care 2008;37(1):78–92. [Google Scholar]
- 28. Bishay LC, Sawicki GS. Strategies to optimize treatment adherence in adolescent patients with cystic fibrosis. Adolesc Health Med Ther 2016;7:117–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hagel S, Reischke J, Kesselmeier M, Winning J, Gastmeier P, Brunkhorst FM, et al. Quantifying the Hawthorne effect in hand hygiene compliance through comparing direct observation with automated hand hygiene monitoring. Infect Control Hosp Epidemiol 2015;36(8):957–962. [DOI] [PubMed] [Google Scholar]
- 30. DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care 2002;40(9):794–811. [DOI] [PubMed] [Google Scholar]
- 31. Burkhart PV, Dunbar-Jacob JM, Rohay JM. Accuracy of children's self-reported adherence to treatment. J Nurs Scholarsh 2001;33(1):27–32. [DOI] [PubMed] [Google Scholar]