Abstract
Background
Hypertension is a rapidly growing epidemic in China. Yet, it remains inadequately controlled, especially in rural areas. The internet has shown potential for better health management in different settings; however, few studies have investigated its role in hypertension management in China.
Objective
This study aims to examine the association between internet access and hypertension awareness, treatment, and control among elderly Chinese adults and to investigate whether the association between internet access and hypertension management differed between those living in urban and rural areas.
Methods
We obtained data from the nationally representative survey of the China Health and Retirement Longitudinal Study in 2011. Hypertension was defined as (1) average systolic blood pressure of ≥140 mm Hg or average diastolic blood pressure of ≥90 mm Hg or (2) currently taking antihypertensive medications. The outcome assessed included hypertension awareness, treatment, and control. The key independent variable was defined as whether one had internet access at home. We performed multivariate logistic regressions for each of the 3 outcomes.
Results
Among 5135 hypertensive respondents (age 62.4 [SD 9.9] years; 2351/5135, 45.78% men), 12.89% (662/5135) had internet access at home. Compared with those who had no internet access, internet access was positively associated with hypertension awareness (odds ratio [OR] 1.36, 95% CI 1.07-1.73) and treatment (OR 1.38, 95% CI 1.09-1.75), but not with control (OR 1.19, 95% CI 0.90-1.58). Internet access reduced urban-rural disparity in hypertension awareness by 9.6% (P=.02), treatment by 8.3% (P=.05), but not in control. In addition, the moderating effect of internet access on urban-rural disparities in hypertension management was larger among females. The decreased urban-rural disparities were primarily driven by that internet access improved the management level in rural areas.
Conclusions
Despite the low rate of internet access among the elderly population, the internet shows its potential as a platform for achieving better hypertension management in China. Strategies for reducing the disparities in hypertension management and overall disease burden of hypertension among the elderly population might consider the internet as a platform.
Keywords: China, health disparity, hypertension, internet
Introduction
Hypertension is a major health problem and largely contributes to morbidity and mortality worldwide [1]. In China, there is a growing epidemic of hypertension among the population as a whole and urban and rural population specifically [2]. Over the past decades, lifestyle and dietary pattern have changed substantially in rural areas owing to China’s rapid economic growth and urbanization [3]. As a result, the hypertension prevalence in the rural population is getting close to that of their urban counterparts [3]. However, most health facilities and human resources are located in urban areas [4]. Partially owing to the unequal distribution of health resources, a very pronounced gap exists in hypertension awareness, treatment, and control between urban and rural residence in China [2].
The successful management of hypertension, like optimal control of many other chronic diseases, requires early detection and sufficient compliance to medications [5]. A growing strand of literature has studied the internet as a potential platform for improved disease management. The internet provides patients opportunities for efficient information search and purchase of medication and devices, timely consulting with health providers, as well as real-time data monitoring [6-8]. Positive empirical evidence in developed countries has accumulated in the field of chronic diseases control like diabetes, respiratory disease, and cardiac disease [9-11]. However, 2 key questions remained unanswered; first, does the positive effect on chronic disease management found in other settings apply to hypertension management in China, where access to qualified health workers and effective medications is limited [12]; second, given the large urban-rural disparity in hypertension management in China [13], is the association between internet access and hypertension management differential between urban and rural areas? If so, is internet widening or narrowing existing urban-rural disparities of hypertension management?
To fill this gap, this study uses a nationally representative survey to examine the role of internet access in hypertension management among the elderly population in China. The objectives of this study are 2-fold as follows: (1) to examine the association between internet access and hypertension awareness, treatment and control among elderly Chinese adults and (2) to investigate whether the association between internet access and hypertension management differed between those living in urban and rural areas.
Methods
Data and Sample
Data for this study were obtained from the 2011 round of China Health and Retirement Longitudinal Study (CHARLS 2011). In China, CHARLS is a nationally representative longitudinal survey of adults aged ≥45 years and their spouses, including assessments of social, economic, and health circumstances of community residents [14]. CHARLS 2011 was conducted between June 2011 and March 2012 and included 17,708 participants from 450 communities in 28 provinces. All participants provided written informed consent, and survey protocols were approved by the Peking University Ethics Review Board [15].
This study sample was selected from respondents who completed the survey and provided biomarker information of blood pressure measurement in CHARLS 2011 (n=13,965). The likelihood of nonresponse appeared to be uncorrelated with demographic, socioeconomic status characteristics [15]. Of 13,965 participants, 5260 (37.66%) were found to have hypertension (see the following subsection for detailed measurement of hypertension). Our final analytic sample included 5135 individuals who had hypertension and provided complete data for all study variables (Figure 1).
Figure 1.
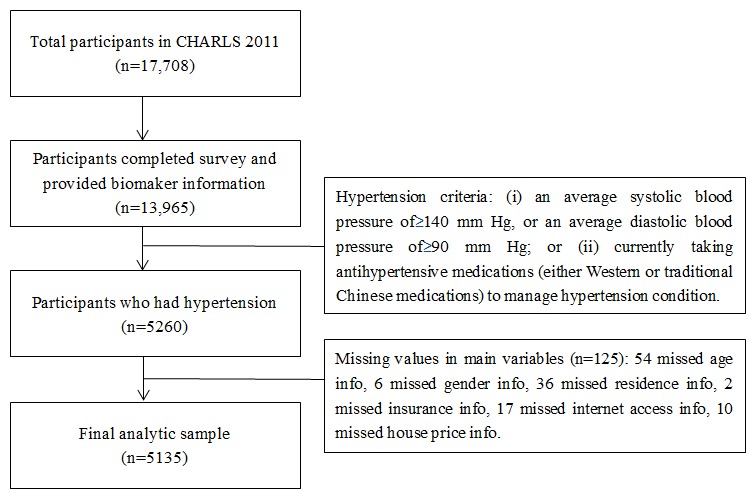
Flowchart of sample selection from the CHARLS 2011.
Outcome Measures and Covariates
Blood pressure was measured 3 times at 45-second intervals using an Omron HEM-7200 monitor (Omron, Dalian Co, LTD, Dalian, China) during the daytime. Respondents were asked to relax and remain seated when measured by professionals. The final analytic blood pressure level was calculated by averaging these 3 measures. Hypertension was defined as (1) average systolic blood pressure of ≥140 mm Hg or average diastolic blood pressure of ≥90 mm Hg or (2) currently taking antihypertensive medications (either Western or traditional Chinese medications) to manage hypertension condition.
This study analyzed the following 3 hypertension management variables as outcome variables: (1) Hypertension Awareness, defined as an individual with hypertension who reported previous diagnosis of hypertension or simply claimed to have hypertension; (2) Hypertension Treatment, defined as an individual with hypertension who claimed to be taking any antihypertensive medications (either Western or traditional Chinese medications); and (3) Hypertension Control, defined as an individual with hypertension whose average systolic blood pressure <140 mm Hg and average diastolic blood pressure <90 mm Hg from the blood pressure measures.
Demographic and socioeconomic status covariates for this study included age (45-59, 60-69, and >70), gender (male or female), educational attainment (illiterate, part of primary school, primary school, middle school, high school or above), marital status (married, widowed, separated, divorced, or never married), and insurance status (whether or not uninsured). Family wealth was measured by the market price of the house an individual owned and currently resided. As about 16.38% (841/5135) of our sample did not own a house, their family wealth was coded as zero. Then, a categorical variable of 3 terciles was generated, which cut the sample into lower, middle, and upper tercile based on the value of their family wealth. Lifestyle covariate included smoking behavior (currently smoking or not), comorbidities covariate included the number of co-occurring chronic diseases (whether >3 co-occurring chronic diseases). The key independent variable was defined as whether one had internet access at home. Urban or rural residence was defined as the Hukou household registration record of the individual during the survey.
Statistical Analysis
A descriptive analysis presented the characteristics of study participants among the full sample as a whole and by a subsample of urban and rural areas. Two multivariate logistic regression models were estimated to investigate the role of internet access in hypertension management. Model 1 regressed each outcome variable on internet access and urban residence. Model 2 added an additional regressor of the interaction term between urban residence and internet access. Both models were adjusted for covariates with a P ≤.05 in the descriptive analysis. Province fixed effects were added in both models to adjust for unobserved provincial-level factors. The sign of interaction term in Model 2 could be interpreted as whether internet access modified the urban-rural disparity of hypertension management [16,17].
To provide a more intuitive interpretation of the moderating effect of internet access on the urban-rural disparity of hypertension management, we computed the mean and SE of marginal effects for the interaction term in logistic regressions. We repeated our computation using full sample and subsample by gender. In addition, we calculated whether the moderating effect of internet access on urban-rural disparities was primarily driven by the fact that internet changed hypertension management levels in urban or rural areas. All analyses were conducted in Stata 14.1 (StataCorp LP).
Results
Characteristics of Study Participants
Data from 5135 eligible participants with hypertension aged ≥45 years (4000 rural subjects and 1135 urban subjects) were included for analysis. Table 1 provides the characteristics of these participants. Hypertension management levels were low, and among the 5135 participants, awareness, treatment, and control rate were 56.94% (2924), 49.15% (2524), and 20.29% (1042), respectively. Compared with urban participants, rural participants were younger (945/4000, 23.62%, aged ≥70 years in rural areas vs 324/1135, 28.6%, in urban; P<.001), comprised more females (2228/4000, 55.70% vs 556/1135, 48.99%; P<.001), were less educated (1497/4000, 37.42%, were illiterate in rural areas vs 144/1135, 12.69%, in urban; P<.001), were poorer (1160/4000, 29.0%, were in rich tercile of family wealth in rural areas vs 522/1135, 45.99%, in urban; P<.001), and had less access to internet at home (329/4000, 8.22% vs 333/1135, 29.34%; P<.001), but were less likely to be uninsured (236/4000, 5.90% vs 118/1135, 10.40%; P<.001). In terms of hypertension management, rural participants had lower rates of awareness (2165/4000, 54.12%, in rural vs 759/1135, 66.87%, in urban; P<.001), treatment (1834/4000, 45.85%, in rural vs 690/1135, 60.79%, in urban; P<.001), and control (734/4000, 18.35%, in rural vs 308/1135, 27.14%, in urban; P<.001) than their urban counterparts.
Table 1.
Characteristics of the study participants.
| Characteristics | National (n=5135), n (%) | Rural (n=4000), n (%) | Urban, (n=1135), n (%) | P value | ||||||||
| Covariates | ||||||||||||
|
|
Age in years | <.001 | ||||||||||
|
|
|
45-59 | 2153 (41.93) | 1718 (42.95) | 435 (38.33) | |||||||
|
|
|
60-69 | 1713 (33.36) | 1337 (33.42) | 376 (33.13) | |||||||
|
|
|
≥70 | 1269 (24.71) | 945 (23.62) | 324 (28.55) | |||||||
|
|
Male sex | 2351 (45.78) | 1772 (44.30) | 579 (51.01) | <.001 | |||||||
|
|
Education | <.001 | ||||||||||
|
|
|
Illiterate | 1641 (31.96) | 1497 (37.42) | 144 (12.69) | |||||||
|
|
|
Part of primary school | 945 (18.40) | 822 (20.55) | 123 (10.84) | |||||||
|
|
|
Primary school | 1139 (22.18) | 883 (22.07) | 256 (22.56) | |||||||
|
|
|
Middle school | 913 (17.78) | 612 (15.30) | 301 (26.52) | |||||||
|
|
|
High school or above | 497 (9.68) | 186 (4.65) | 311 (27.40) | |||||||
|
|
Marital status | .32 | ||||||||||
|
|
|
Married | 4220 (82.18) | 3269 (81.72) | 951 (83.79) | |||||||
|
|
|
Widowed | 801 (15.60) | 647 (16.18) | 154 (13.57) | |||||||
|
|
|
Separated, divorced, or never married | 114 (2.22) | 84 (2.10) | 30 (2.64) | |||||||
|
|
Market price of house | <.001 | ||||||||||
|
|
|
Poor tercile | 1803 (35.11) | 1415 (35.38) | 388 (34.19) | |||||||
|
|
|
Middle tercile | 1650 (32.13) | 1425 (35.62) | 225 (19.82) | |||||||
|
|
|
Rich tercile | 1682 (32.76) | 1160 (29.00) | 522 (45.99) | |||||||
|
|
Uninsured | 354 (6.89) | 236 (5.90) | 118 (10.40) | <.001 | |||||||
|
|
>3 co-occurring chronic diseases | 1180 (36.61) | 1415 (35.38) | 465 (40.97) | .001 | |||||||
|
|
Currently smoke | 2007 (39.08) | 1556 (38.90) | 451 (39.74) | .61 | |||||||
| Internet access at home as key independent variable | 662 (12.89) | 329 (8.22) | 333 (29.34) | <.001 | ||||||||
| Hypertension management | ||||||||||||
|
|
Awareness | 2924 (56.94) | 2165 (54.12) | 759 (66.87) | <.001 | |||||||
|
|
Treatment | 2524 (49.15) | 1834 (45.85) | 690 (60.79) | <.001 | |||||||
|
|
Control | 1042 (20.29) | 734 (18.35) | 308 (27.14) | <.001 | |||||||
Association Between Internet Access and Hypertension Management
Figure 2 plots the odds ratios (ORs) of multivariate logistic regressions. Without adding the interaction term between urban residence and interaction access (Model 1), internet access at home was positively associated with all of the 3 hypertension management outcomes; however, none of the coefficients was statistically significant: hypertension awareness (OR 1.14, 95% CI 0.95-1.37; P=.17), treatment (OR 1.19, 95% CI 0.99-1.43; P=.06), and control (OR 1.14, 95% CI 0.93-1.41; P=.21). In addition, we found significant and notable urban-rural disparities in hypertension awareness (OR 1.55, 95% CI 1.33-1.82; P<.001), treatment (OR 1.66, 95% CI 1.43-1.94; P<.001), and control (OR 1.50, 95% CI 1.25-1.78; P<.001).
Figure 2.
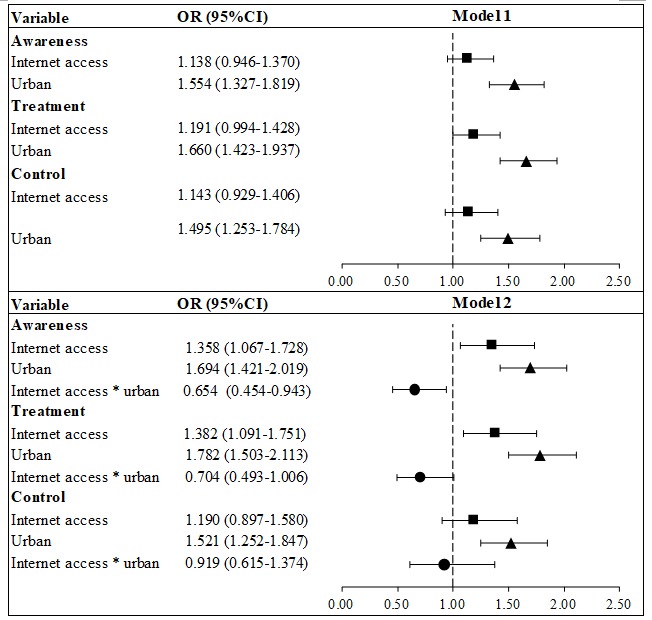
Multivariate logistic regressions on multivariate relationship of internet access and urban residence to hypertension management.
After adding the interaction term (Model 2), the positive associations between internet access and hypertension management became statistically significant and with larger coefficient sizes in hypertension awareness (OR 1.36, 95% CI 1.07-1.73; P=.01) and treatment (OR 1.38, 95% CI 1.09-1.75; P=.007), but not in hypertension control (OR 1.19, 95% CI 0.90-1.58; P=.23). In terms of urban-rural disparities, the coefficient sizes were even larger in all 3 outcomes: hypertension awareness (OR 1.69, 95% CI 1.42-2.02; P<.001), treatment (OR 1.78, 95% CI 1.50-2.11; P<.001), and control (OR 1.52, 95% CI 1.25-1.85; P<.001).
Association Between Internet Access and Urban-Rural Disparity of Hypertension Management
The ORs of the interaction term were <1 for each outcome, indicating that internet access reduced the urban-rural gap in hypertension management, although the OR of the interaction term in hypertension control was statistically insignificant. Specifically, the OR of the interaction term between internet access and urban residence in hypertension awareness was 0.65 (95% CI 0.45-0.94; P=.02), indicating that the effect of internet access on being aware of hypertensive status for urban residents was 35% smaller than that on rural residents. Similar patterns were also observed for hypertension treatment (OR 0.70, 95% CI 0.49-1.01; P=.05) and control (OR 0.92, 95% CI 0.62-1.37; P=.68).
Tables 2, 3, and 4 provide a more intuitive interpretation of whether internet access modified the urban-rural disparities on hypertension management by presenting the mean marginal effects of the interaction term between urban residence and internet access. Internet access reduced the urban-rural disparities on hypertension awareness by 9.6% (P=.02), hypertension treatment by 8.3% (P=.05). We observed no statistically significant change in hypertension control. In addition, these interaction effects were disproportionally and more significantly benefiting female participants; internet access reduced the urban-rural disparities in hypertension awareness by 14.7% (P=.01), in hypertension treatment by 14.5% (P=.01) among female participants.
Table 2.
Marginal effects of the interaction term between urban residence and internet access for the awareness hypertension.
| Population | Coefficient | SE | P value |
| Total (N=5135) | −0.096a | 0.042 | .02 |
| Male (N=2351) | −0.046a | 0.061 | .45 |
| Female (N=2784) | −0.147a | 0.057 | .01 |
aAll values adjusted for 6 covariates with a P ≤.05 in Table 1: age, gender, educational level, uninsured, the market price of the house, >3 co-occurring chronic diseases. Province fixed effects were also adjusted.
Table 3.
Marginal effects of the interaction term between urban residence and internet access for the treatment of hypertension.
| Population | Coefficient | SE | P value |
| Total (N=5135) | −0.083a | 0.042 | .05 |
| Male (N=2351) | −0.012a | 0.062 | .83 |
| Female (N=2784) | −0.145a | 0.058 | .01 |
aAll values adjusted for 6 covariates with a P ≤.05 in Table 1: age, gender, educational level, uninsured, the market price of the house, and >3 co-occurring chronic diseases. Province fixed effects were also adjusted.
Table 4.
Marginal effects of the interaction term between urban residence and internet access for the control of hypertension.
| Population | Coefficient | SE | P value |
| Total (N=5135) | −0.010a | 0.036 | .79 |
| Male (N=2351) | 0.075a | 0.052 | .15 |
| Female (N=2784) | −0.091a | 0.050 | .07 |
aAll values adjusted for 6 covariates with a P ≤.05 in Table 1: age, gender, educational level, uninsured, the market price of the house, and >3 co-occurring chronic diseases. Province fixed effects were also adjusted.
The decreased urban-rural disparities in hypertension awareness and treatment associated with internet access were primarily driven by the significant improvement of management level in rural areas among those with internet access at home compared with those without internet access at home. However, the management level remained constant in urban areas between those with and without internet access at home (Tables 5, 6, and 7).
Table 5.
Estimated hypertension awareness by urban residence and internet access.
| Variable | Rurala | Urbana |
| No Internet | 0.43 (0.03) | 0.54 (0.02) |
| Internet | 0.49 (0.03) | 0.49 (0.03) |
| P value | .03 | .10 |
aAll values adjusted for 6 covariates with a P ≤.05 in Table 1: age, gender, educational level, uninsured, the market price of the house, and >3 co-occurring chronic diseases. Province fixed effects were also adjusted.
Table 6.
Estimated hypertension treatment by urban residence and internet access.
| Variable | Rurala | Urbana |
| No Internet | 0.34 (0.03) | 0.47 (0.02) |
| Internet | 0.41 (0.03) | 0.44 (0.03) |
| P value | .02 | .27 |
aAll values adjusted for 6 covariates with a P ≤.05 in Table 1: age, gender, educational level, uninsured, the market price of the house, >3 co-occurring chronic diseases. Province fixed effects were also adjusted.
Table 7.
Estimated hypertension control by urban residence and internet access.
| Variable | Rurala | Urbana |
| No Internet | 0.15 (0.03) | 0.22 (0.02) |
| Internet | 0.17 (0.02) | 0.22 (0.03) |
| P value | .44 | .89 |
aAll values adjusted for 6 covariates with a P ≤.05 in Table 1: age, gender, educational level, uninsured, the market price of the house, >3 co-occurring chronic diseases. Province fixed effects were also adjusted.
Discussion
Principal Findings
To the best of our knowledge, this study was the first to examine the role of internet access in hypertension management among the elderly population in China. Hypertension is a leading cause of mortality and disability around the world [18]. In China, it accounted for >2.5 million deaths (almost one-third of total deaths) and 15% of total disability-adjusted life-years in 2013, mainly from stroke and ischemic heart disease [18,19]. Over the past decade, the proportion of population connected to the internet has been growing exponentially [20], and researchers in the field of health promotion have been quick to capitalize on the internet to promote changes in health behavior in many settings [21]. Taking advantage of the population-based nationally representative survey CHARLS 2011, we were able to investigate whether the positive effect of the internet on disease management found in other settings still holds in the context of China, where fast economic growth and population aging are happening simultaneously, and more importantly, whether the internet has a moderating effect on the existing urban-rural gap in hypertension management.
In this study, several key findings were highlighted. First, internet access at home was associated with better hypertension management among elderly Chinese adults. Previous studies have found a positive effect of the internet on disease management in different settings [22-26]. For example, one randomized trial proved that internet-based chronic disease self-management program was effective in changing health-related behaviors and improving the health status of patients with chronic diseases [7]. However, few have investigated whether this positive effect still holds in developing context such as China. The positive association between internet access and hypertension management in this study was of practical importance in the sense that China is facing a huge public health crisis of hypertension in which sufficient awareness and compliance to medications are the necessary steps to achieve adequate control.
Second, the finding that internet access was associated with decreased urban-rural disparities in hypertension management was encouraging. The existing gap in hypertension awareness, treatment, and control between urban and rural areas found in this study paralleled that of a recent nationwide population-based epidemiology study of hypertension prevalence and management among Chinese adults [2]. In this study, we were able to use a rich individual-level dataset and examine the association between internet access and urban-rural disparities in hypertension management adjusted for demographic characteristics, socioeconomic status, comorbidity, and lifestyle factors. The magnitudes of 9.6% decrease in hypertension awareness and 8.3% decrease in hypertension treatment were considered to be substantial compared with other studies measuring urban-rural disparities in hypertension management among Chinese patients [13,27]. A well-documented contributor to China’s urban-rural disparities in health, including hypertension management, is the unequal distribution of health workforce [28]. Efforts to cope with the shortage of health care workers in rural areas have been slow, especially at primary care level [29]. Our finding provided suggestive evidence that the internet could help to cope with the limited access to quality care in rural areas. More broadly, our results might shed lights to improve health equity in China [30].
Third, a significant and substantial reduction in urban-rural disparity of hypertension awareness and treatment did not translate into the reduction of hypertension control; therefore, improving both is necessary but not sufficient to achieve the optimal control of hypertension [2]. Hypertension control often requires multiple medications, yet in rural China, the availability and affordability to antihypertensive drugs were limited [31]. A recent national study showed that less than one-third of primary health care institutions stocked guideline-recommended and low-cost antihypertensive medications, and unfortunately the deficiencies were even worse in rural areas [31].
Exploring clear mechanisms in explaining the association between internet access and decreased urban-rural disparities in hypertension management was beyond the scope of this study. Nevertheless, we found the association was more notable and statistically significant among female participants. This was in line with a series of studies emphasizing the fact that female patients are more responsive to hypertension management interventions [32,33]. Future studies should focus on understanding channels through which internet access works on improving hypertension management. In addition, decreased urban-rural disparities in hypertension management were primarily driven by the fact that internet access improved management levels in rural areas. This is an encouraging finding, highlighting the importance of improving the hypertension management in rural areas to reduce the burden of hypertension [34]. Furthermore, the results of this study were consistent with previous studies that showed better health management by the internet-based health care models in rural areas and less-developed regions [35,36].
Limitations
This study has several limitations. First, the observational nature of our study limited our ability to draw any causal inference from our findings. The results should not be interpreted as the effect of internet access on reducing urban-rural disparities in hypertension management. Rather, the association found in this study underscored the need for research to capitalize on new technologies to mitigate the disease burden of hypertension. Second, measuring blood pressure 3 times in the CHARLS study might not lead to the most accurate hypertension diagnosis. The medical literature has confirmed that the 24-hour ambulatory blood pressure monitoring to be the best assessment of hypertension [37]. However, given the large-scale, population-based survey design of CHARLS, the 24-hour ambulatory blood pressure monitoring might not be cost-effective or feasible in implementation. Third, in the 2011 round of CHARLS survey, only 29% and 8% household had internet access in urban and rural areas. This low rate of internet access among our sample population might limit us to generate policy relevance. Although we did not have data of latest internet access among the elderly population, it was reported that internet availability has improved markedly across the country over the past few years [20]. Nonetheless, this lower internet access rate might make our estimates of the association between internet access and reduced urban-rural disparities in hypertension management conservative. Fourth, although the 2.4% nonresponse rate could be considered as low given the large-scale survey of CHARLS, our nonresponse analysis was only limited to comparing hypertension outcome variables between response and nonresponse groups. We have to acknowledge that the nonresponse analysis provided by CHARLS was based on the whole sample, which might not apply to our sample of hypertensive participants. However, because those nonresponses in our study did not complete the survey and only provided biomarker information, we were only to compare the hypertension outcome variables and found nonresponse was not associated with hypertension awareness, treatment, and control (see Multimedia Appendix 1). Last but not least, even if we used a nationally representative survey of the elderly population in China, the generalizability of our results should be limited to the context of China. Given the rapid pace of population aging in China, we believed that our results among elderly adults were of policy importance to that specific population in China.
Conclusions
Hypertension is becoming a public crisis in China and around the globe. Using a nationally representative survey of Chinese elderly, we found that internet access at home was associated with better hypertension management, and internet access reduced the urban-rural gap in hypertension management outcomes. Despite the low rate of internet access among the elderly population, the internet shows its potential as a platform for achieving better hypertension management in China. Longitudinal studies on the internet and hypertension management, because internet facilities have improved significantly in recent years, are needed. Given the growing epidemic of hypertension and the rapid pace of population aging in China, we believe that this study sheds lights on designing polices for achieving optimal hypertension management and health equity in China. Strategies for reducing the disparities in hypertension management and overall disease burden of hypertension might consider the internet as a platform for disease management.
Acknowledgments
The authors would like to acknowledge Jingyuan Xiao (Yale University) for her insightful comments and proofreading of the manuscript. They would also like to acknowledge the CHARLS team for providing data and the training of using the dataset.
This study was supported by Peking University Health Science Center start-up fund (grant no. BMU20160514). The study sponsor has no role in study design, data analysis and interpretation of data, the writing of the manuscript, or the decision to submit the paper for publication.
Abbreviations
- CHARLS
China Health and Retirement Longitudinal Study
- OR
odds ratio
Comparison of hypertension management outcomes between response group and non-response group.
Footnotes
Authors' Contributions: YJ analyzed the data and revised the manuscript. MJ, LZ, and SS revised the manuscript. XM designed the study, analyzed the data, and revised the manuscript.
Conflicts of Interest: None declared.
References
- 1.Olsen MH, Angell SY, Asma S, Boutouyrie P, Burger D, Chirinos JA, Damasceno A, Delles C, Gimenez-Roqueplo A, Hering D, López-Jaramillo P, Martinez F, Perkovic V, Rietzschel ER, Schillaci G, Schutte AE, Scuteri A, Sharman JE, Wachtell K, Wang JG. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension. Lancet. 2016 Dec 26;388(10060):2665–2712. doi: 10.1016/S0140-6736(16)31134-5. http://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(16)31134-5.pdf .10.1016/s0140 -6736(16)31134-5 [DOI] [PubMed] [Google Scholar]
- 2.Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, Cheng X, Mu L, Zhang H, Liu J, Su M, Zhao H, Spatz ES, Spertus JA, Masoudi FA, Krumholz HM, Jiang L. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE Million Persons Project) Lancet. 2017 Dec 09;390(10112):2549–2558. doi: 10.1016/S0140-6736(17)32478-9. http://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(17)32478-9.pdf .10.1016/S0140-6736(17)32478- 9 [DOI] [PubMed] [Google Scholar]
- 3.Li J, Shi L, Li S, Xu L, Qin W, Wang H. Urban-rural disparities in hypertension prevalence, detection, and medication use among Chinese Adults from 1993 to 2011. Int J Equity Health. 2017 Dec 14;16(1):50–60. doi: 10.1186/s12939-017-0545-7. https://equityhealthj.biomedcentral.com/articles/10.1186/s12939-017-0545-7 .10.1186/s12939-017-0545-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yip W, Hsiao W, Chen W, Hu S, Ma J, Maynard A. Early appraisal of China's huge and complex health-care reforms. Lancet. 2012 Mar 03;379(9818):833–42. doi: 10.1016/S0140-6736(11)61880-1. http://sci-hub.hk/https:/www.sciencedirect.com/science/article/pii/S0140673611618801 .10.1016/S0140-6736(11)61880-1 [DOI] [PubMed] [Google Scholar]
- 5.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003 May 21;289(19):2560–72. doi: 10.1001/jama.289.19.2560. https://www.researchgate.net/profile/Lee_Green2/publication/10759194_The_Seventh_Report_of_the_Joint_National_Committee_on_Prevention_Detection_Evaluation_and_Treatment_of_High_Blood_Pressure_The_JNC_7_Report/links/00463524d85b7d77ad000000.pdf .10.1001/jama.289.19.2560 [DOI] [PubMed] [Google Scholar]
- 6.Fox SP. Chronic disease and the Internet. Washington, DC: Pew Internet & American Life Project; 2010. [Google Scholar]
- 7.Lorig KR, Ritter PL, Laurent DD, Plant K. Internet-based chronic disease self-management: a randomized trial. Med Care. 2006 Nov;44(11):964–71. doi: 10.1097/01.mlr.0000233678.80203.c1. http://telehomecare.otn.ca/documents/10157/19426/Internet-Based+Chronic+Disease+Self-Management+A+Randomized+Trial.pdf?version=1.0 .10.1097/01.mlr.0000233678.80203.c1 [DOI] [PubMed] [Google Scholar]
- 8.Stellefson M, Chaney B, Barry AE, Chavarria E, Tennant B, Walsh-Childers K, Sriram PS, Zagora J. Web 2.0 chronic disease self-management for older adults: a systematic review. J Med Internet Res. 2013 Feb 14;15(2):e35. doi: 10.2196/jmir.2439. http://www.jmir.org/2013/2/e35/ 10.2196/jmir.2439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Polisena J, Tran K, Cimon K, Hutton B, McGill S, Palmer K. Home telehealth for diabetes management: a systematic review and meta-analysis. Diabetes Obes Metab. 2009 Oct;11(10):913–30. doi: 10.1111/j.1463-1326.2009.01057.x. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1463-1326.2009.01057.x .10.1111/j.1463-1326.2009.01057.x [DOI] [PubMed] [Google Scholar]
- 10.Clark RA, Inglis SC, McAlister FA, Cleland JG, Stewart S. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. BMJ. 2007 May 05;334(7600):942–950. doi: 10.1136/bmj.39156.536968.55. http://www.bmj.com/content/bmj/334/7600/942.full.pdf .10.1136/bmj.39156.536968.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jaana M, Paré G, Sicotte C. Home telemonitoring for respiratory conditions: a systematic review. Am J Manag Care. 2009 May;15(5):313–20. http://www.ajmc.com/journals/issue/2009/2009-05-vol15-n5/ajmc_09may_jaana_313to320 .11123 [PubMed] [Google Scholar]
- 12.National Health and Family Planning Commission . Health statistics yearbook. Beijing: Ministry of Health; 2012. [Google Scholar]
- 13.Hou X. Urban-rural disparity of overweight, hypertension, undiagnosed hypertension, and untreated hypertension in China. Asia Pac J Public Health. 2008;20(2):159–69. doi: 10.1177/1010539507312306. http://journals.sagepub.com/doi/pdf/10.1177/1010539507312306 .10.1177/1010539507312306 [DOI] [PubMed] [Google Scholar]
- 14.Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS) Int J Epidemiol. 2014 Feb;43(1):61–8. doi: 10.1093/ije/dys203. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3937970/pdf/dys203.pdf .doi: 10.1093/ije/dys203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhao Y, Strauss J, Yang G, Giles J, Hu P, Hu Y, Lei X, Liu M, Park A, Smith JP, Wang Y. China health and retirement longitudinal study? 46-2012 national baseline users? guide. Beijing: Peking University; 2011. [Google Scholar]
- 16.Norton EW, Ai C. The Stata Journal. 2004. Computing interaction effects and standard errors in logit and probit models https://www.researchgate.net/profile/Paul_Louangrath/post/How_can_I_ENTER_a_4-way_interactions_of_variables_in_blocks_of_the_hierarchical_multiple_regression_analysis_in_SPSS/attachment/59d644d2c49f478072ead786/AS:273819644694528@1442295099036/download/INTERACTION-1.pdf .
- 17.Buis ML. The Stata Journal. 2010. [2018-11-28]. Stata tip 87: Interpretation of interactions in non-linear models http://ageconsearch.umn.edu/bitstream/152319/2/sjart_st0194.pdf . [PMC free article] [PubMed]
- 18.GBD 2013 Risk Factors Collaborators. Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, Brauer M, Burnett R, Casey D, Coates MM, Cohen A, Delwiche K, Estep K, Frostad JJ, Astha KC, Kyu HH, Moradi-Lakeh M, Ng M, Slepak EL, Thomas BA, Wagner J, Aasvang GM, Abbafati C, Abbasoglu Ozgoren A, Abd-Allah F, Abera SF, Aboyans V, Abraham JP, Abraham JP, Abubakar I, Abu-Rmeileh NME, Aburto TC, Achoki TE, Adelekan A, Adofo K, Adou AK, Adsuar JC, Afshin AC, Agardh EE, Al Khabouri MJ, Al Lami FH, Alam SS, Alasfoor D, Albittar MI, Alegretti MA, Aleman AV, Alemu ZA, Alfonso-Cristancho R, Alhabib S, Ali MK, Ali MK, Alla F, Allebeck PS, Allen PJ, Alsharif U, Alvarez EC, Alvis-Guzman N, Amankwaa AA, Amare AT, Ameh EA, Ameli O, Amini H, Ammar W, Anderson BO, Antonio CAT, Anwari P, Argeseanu Cunningham s, Arnlöv J, Arsenijevic VSA, Artaman Al, Asghar RJ, Assadi RC, Atkins LS, Atkinson CL, Avila MA, Awuah B, Badawi A, Bahit MC, Bakfalouni T, Balakrishnan K, K S, Balu RK, Banerjee A, Barber RM, Barker-Collo SL, Barquera S, Barregard L, Barrero LH, Barrientos-Gutierrez TM, Basto-Abreu AC, Basu S, Basu S, Basulaiman MO, Batis Ruvalcaba C, Beardsley J, Bedi N, Bekele T, Bell ML, Benjet C, Bennett DA, Benzian H, Bernabé E, Beyene TJ, Bhala N, Bhalla A, Bhutta ZA, Bikbov B, Bin Abdulhak AA, Blore JD, Blyth FM, Bohensky MA, Bora BaÅŸara B, Borges G, Bornstein NM, Bose D, Boufous S, Bourne RR, Brainin M, Brazinova A, Breitborde NJ, Brenner H, Briggs ADM, Broday DM, Brooks PM, Bruce NG, Brugha TS, Brunekreef P, Buchbinder R, Bui LN, Bukhman G, Bulloch AG, Burch M, Burney PGJ, Campos-Nonato IR, Campuzano JC, Cantoral AJ, Caravanos J, Cárdenas R, Cardis E, Carpenter DO, Caso V, Castañeda-Orjuela CA, Castro RE, Catalá-López F, Cavalleri F, Çavlin A, Chadha VK, Chang J-C, Charlson FJ, Chen W, Chen Z, Chen Z, Chiang PB, Chimed-Ochir O, Chowdhury R, Christophi CA, Chuang T-W, Chugh SS, Cirillo M, Claßen TKD, Colistro V, Colomar M, Colquhoun SM, Contreras AG, Cooper C, Cooperrider K, Cooper LT, Coresh J, Courville KJ, Criqui MH, Cuevas-Nasu L, Damsere-Derry J, Danawi H, Dandona R, Dandona R, Dargan PI, Davis A, Davitoiu DV, Dayama A, de Castro EP, De la Cruz-Góngora V, De Leo D, de Lima G, Degenhardt L, del Pozo-Cruz B, Dellavalle RP, Deribe K, Derrett S, Des Jarlais DC, Dessalegn M, deVeber GA, Devries KM, Dharmaratne SD, Dherani MK, Dicker D, Ding EL, Dokova K, Dorsey ER, Driscoll TR, Duan L, Durrani AM, Ebel BE, Ellenbogen RG, Elshrek YM, Endres M, Ermakov SP, Erskine HE, Eshrati B, Esteghamati A, Fahimi S, Faraon EJA, Farzadfar F, Fay DFJ, Feigin VL, Feigl AB, Fereshtehnejad S-M, Ferrari AJ, Ferri CP, Flaxman AD, Fleming TD, Foigt N, Foreman KJ, Paleo UF, Franklin RC, Gabbe B, Gaffikin L, Gakidou E, Gamkrelidze A, Gankpé FG, Gansevoort RT, García-Guerra FA, Gasana E, Geleijnse JM, Gessner BD, Gething P, Gibney KB, Gillum RF, Ginawi IAM, Giroud M, Giussani G, Goenka S, Goginashvili K, Gomez Dantes H, Gona P, Gonzalez de Cosio T, González-Castell D, Gotay CC, Goto A, Gouda HN, Guerrant RL, Gugnani HC, Guillemin F, Gunnell D, Gupta R, Gupta R, Gutiérrez RA, Hafezi-Nejad N, Hagan H, Hagstromer M, Halasa YA, Hamadeh RR, Hammami M, Hankey GJ, Hao Y, Harb HL, Haregu TN, Haro JM, Havmoeller R, Hay SI, Hedayati MT, Heredia-Pi IB, Hernandez L, Heuton KR, Heydarpour P, Hijar M, Hoek HW, Hoffman HJ, Hornberger JC, Hosgood HD, Hoy DG, Hsairi M, Hu H, Hu H, Huang JJ, Huang JJ, Hubbell BJ, Huiart L, Husseini A, Iannarone ML, Iburg KM, Idrisov BT, Ikeda N, Innos K, Inoue M, Islami F, Ismayilova S, Jacobsen KH, Jansen HA, Jarvis DL, Jassal SK, Jauregui A, Jayaraman S, Jeemon P, Jensen PN, Jha V, Jiang G, Jiang Y, Jiang Y, Jonas JB, Juel K, Kan H, Kany Roseline SS, Karam NE, Karch A, Karema CK, Karthikeyan G, Kaul A, Kawakami N, Kazi DS, Kemp AH, Kengne AP, Keren A, Khader YS, Khalifa SEAH, Khan EA, Khang Y-H, Khatibzadeh S, Khonelidze I, Kieling C, Kim S, Kim Y, Kim Y, Kimokoti RW, Kinfu Y, Kinge JM, Kissela BM, Kivipelto M, Knibbs LD, Knudsen AK, Kokubo Y, Kose MR, Kosen S, Kraemer A, Kravchenko M, Krishnaswami S, Kromhout H, Ku T, Kuate Defo B, Kucuk Bicer B, Kuipers EJ, Kulkarni VS, Kulkarni VS, Kumar GA, Kwan GF, Lai T, Lakshmana Balaji A, Lalloo R, Lallukka T, Lam H, Lan Q, Lansingh VC, Larson HJ, Larsson A, Laryea DO, Lavados PM, Lawrynowicz AE, Leasher JL, Lee J-T, Leigh J, Leung R, Levi M, Li Y, Li Y, Liang X, Liang X, Lim SS, Lindsay MP, Lipshultz SE, Liu Y, Liu Y, Lloyd BK, Logroscino G, London SJ, Lopez N, Lortet-Tieulent J, Lotufo PA, Lozano R, Lunevicius R, Ma S, Ma S, Machado VMP, MacIntyre MF, Magis-Rodriguez C, Mahdi AA, Majdan M, Malekzadeh R, Mangalam S, Mapoma CC, Marape M, Marcenes W, Margolis DJ, Margono C, Marks GB, Martin RV, Marzan MB, Mashal MT, Masiye F, Mason-Jones AJ, Matsushita K, Matzopoulos R, Mayosi BM, Mazorodze TT, McKay AC, McKee M, McLain A, Meaney PA, Medina C, Mehndiratta MM, Mejia-Rodriguez F, Mekonnen W, Melaku YA, Meltzer M, Memish ZA, Mendoza W, Mensah GA, Meretoja A, Mhimbira FA, Micha R, Miller TR, Mills EJ, Misganaw A, Mishra S, Mohamed Ibrahim N, Mohammad KA, Mokdad AH, Mola GL, Monasta L, Montañez Hernandez JC, Montico M, Moore AR, Morawska L, Mori R, Moschandreas J, Moturi WN, Mozaffarian D, Mueller UO, Mukaigawara M, Mullany EC, Murthy KS, Naghavi M, Nahas Z, Naheed A, Naidoo KS, Naldi L, Nand D, Nangia V, Narayan KMV, Nash D, Neal B, Nejjari C, Neupane SP, Newton CR, Ngalesoni FN, Ngirabega JD, Nguyen NT, Nguyen NT, Nieuwenhuijsen MJ, Nisar MI, Nogueira JR, Nolla JM, Nolte S, Norheim OF, Norman RE, Norrving B, Nyakarahuka L, Oh I-H, Ohkubo T, Olusanya BO, Omer SB, Opio JN, Orozco R, Pagcatipunan RS, Pain AW, Pandian JD, Panelo CIA, Papachristou C, Park E-K, Parry CD, Paternina Caicedo AJ, Patten SB, Paul VK, Pavlin BI, Pearce N. doi: 10.1016/S0140-6736(15)00128-2. [DOI] [Google Scholar]
- 19.Wang L, Kong L, Wu F, Bai Y, Burton R. Preventing chronic diseases in China. Lancet. 2005 Nov 19;366(9499):1821–4. doi: 10.1016/S0140-6736(05)67344-8. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(05)67344-8/fulltext .10.1016/S0140-67 36(05)67344-8 [DOI] [PubMed] [Google Scholar]
- 20.Kulkarni R, Malouin RA. State of Telehealth. N Engl J Med. 2016 Dec 06;375(14):1399–400. doi: 10.1056/NEJMc1610233. http://www.lesdebatspublicsdelipc.com/wp-content/uploads/2016/07/state-ot-telehealth-nejm.pdf .10.1056/NEJMra1601705 [DOI] [PubMed] [Google Scholar]
- 21.Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res. 2010 Feb 17;12(1):e4. doi: 10.2196/jmir.1376. http://www.jmir.org/2010/1/e4/ 10.2196/jmir.1376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parati G, Torlasco C, Omboni S, Pellegrini D. Smartphone Applications for Hypertension Management: a Potential Game-Changer That Needs More Control. Curr Hypertens Rep. 2017 Jun;19(6):48. doi: 10.1007/s11906-017-0743-0. https://www.researchgate.net/publication/317012638_Smartphone_Applications_for_Hypertension_Management_a_Potential_Game-Changer_That_Needs_More_Control .10.1007/s11906-017-0743-0 [DOI] [PubMed] [Google Scholar]
- 23.Green BB, Cook AJ, Ralston JD, Fishman PA, Catz SL, Carlson J, Carrell D, Tyll L, Larson EB, Thompson RS. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008 Jun 25;299(24):2857–67. doi: 10.1001/jama.299.24.2857. http://europepmc.org/abstract/MED/18577730 .299/24/2857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yatabe MS, Yatabe J, Asayama K, Staessen JA, Mujaj B, Thijs L, Ito K, Sonoo T, Morimoto S, Ichihara A. The rationale and design of reduction of uncontrolled hypertension by Remote Monitoring and Telemedicine (REMOTE) study. Blood Press. 2018 Dec;27(2):99–105. doi: 10.1080/08037051.2017.1406306. https://www.tandfonline.com/doi/pdf/10.1080/08037051.2017.1406306?needAccess=true .10.1080/08037051.2017.1406306 [DOI] [PubMed] [Google Scholar]
- 25.Lu JF, Chen CM, Hsu CY. Effect of home telehealth care on blood pressure control: A public healthcare centre model. J Telemed Telecare. 2017 Jan 01;:1357633X17734258. doi: 10.1177/1357633X17734258. http://journals.sagepub.com/doi/pdf/10.1177/1357633X17734258 .10.1177/1357633X17734258 [DOI] [PubMed] [Google Scholar]
- 26.AbuDagga A, Resnick HE, Alwan M. Impact of blood pressure telemonitoring on hypertension outcomes: a literature review. Telemed J E Health. 2010 Sep;16(7):830–8. doi: 10.1089/tmj.2010.0015. http://paperpile.com/b/eMt7D6/nNty .10.1089/tmj.2010.0015 [DOI] [PubMed] [Google Scholar]
- 27.Wang J, Zhang L, Wang F, Liu L, Wang H, China National Survey of Chronic Kidney Disease Working Group Prevalence, awareness, treatment, and control of hypertension in China: results from a national survey. Am J Hypertens. 2014 Nov;27(11):1355–61. doi: 10.1093/ajh/hpu053. doi: 10.1093/ajh/hpu053.10.1093/ajh/hpu053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anand S, Fan VY, Zhang J, Zhang L, Ke Y, Dong Z, Chen LC. China's human resources for health: quantity, quality, and distribution. Lancet. 2008 Nov 15;372(9651):1774–81. doi: 10.1016/S0140-6736(08)61363-X. http://sci-hub.hk/http:/www.thelancet.com/journals/lancet/article/PIIS0140-6736(08)61363-X/fulltext .10.1016/S0140-6736(08)61363-X [DOI] [PubMed] [Google Scholar]
- 29.Yip W, Hsiao W. Harnessing the privatisation of China's fragmented health-care delivery. Lancet. 2014 Aug 30;384(9945):805–18. doi: 10.1016/S0140-6736(14)61120-X. http://sci-hub.hk/http:/www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(14)61120-X.pdf .10.1016/s0140-6736 (14)61120-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tang S, Meng Q, Chen L, Bekedam H, Evans T, Whitehead M. Tackling the challenges to health equity in China. Lancet. 2008 Oct 25;372(9648):1493–501. doi: 10.1016/S0140-6736(08)61364-1. https://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(08)61364-1.pdf?code=lancet-site .10.1016/S0140-6736(08)61364-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Su M, Zhang Q, Bai X, Wu C, Li Y, Mossialos E, Mensah GA, Masoudi FA, Lu J, Li X, Salas-Vega S, Zhang A, Lu Y, Nasir K, Krumholz HM, Jiang L. Availability, cost, and prescription patterns of antihypertensive medications in primary health care in China: a nationwide cross-sectional survey. Lancet. 2017 Dec 09;390(10112):2559–68. doi: 10.1016/S0140-6736(17)32476-5. https://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(17)32476-5.pdf .10.1016/s0140-6736(17)32476-5 [DOI] [PubMed] [Google Scholar]
- 32.Lustria ML, Smith SA, Hinnant CC. Exploring digital divides: an examination of eHealth technology use in health information seeking, communication and personal health information management in the USA. Health Informatics J. 2011 Sep;17(3):224–43. doi: 10.1177/1460458211414843. http://journals.sagepub.com/doi/pdf/10.1177/1460458211414843 .10.1177/1460458211414843 [DOI] [PubMed] [Google Scholar]
- 33.DiMaggio PH. From the 'Digital Divide' to 'Digital Inequality'tudying Internet Use As Penetration Increases. Princeton: Center for Arts and Cultural Policy Studies, Woodrow Wilson School, Princeton University; 2001. pp. 1–23. [Google Scholar]
- 34.Hou Z, Meng Q, Zhang Y. Hypertension Prevalence, Awareness, Treatment, and Control Following China's Healthcare Reform. Am J Hypertens. 2016 Apr;29(4):428–31. doi: 10.1093/ajh/hpv125. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4886484/pdf/hpv125.pdf .10.1093/ajh/hpv125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang T, Li J, Zhu C, Hong Z, An D, Yang H, Ren J, Zou X, Huang C, Chi X, Chen J, Hong Z, Wang W, Xu C, He Li, Li W, Zhou D. Assessment of Utilization and Cost-Effectiveness of Telemedicine Program in Western Regions of China: A 12-Year Study of 249 Hospitals Across 112 Cities. Telemed J E Health. 2016 Dec;22(11):909–20. doi: 10.1089/tmj.2015.0213. https://www.liebertpub.com/doi/10.1089/tmj.2015.0213 .10.1089/tmj.2015.0213 [DOI] [PubMed] [Google Scholar]
- 36.Piette JD, Mendoza-Avelares MO, Milton EC, Lange I, Fajardo R. Access to mobile communication technology and willingness to participate in automated telemedicine calls among chronically ill patients in Honduras. Telemed J E Health. 2010 Dec;16(10):1030–41. doi: 10.1089/tmj.2010.0074. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3025769/pdf/tmj.2010.0074.pdf .10.1089/tmj.2010.0074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O'Brien E, Coats A, Owens P, Petrie J, Padfield PL, Littler WA, de Swiet M, Mee F. Use and interpretation of ambulatory blood pressure monitoring: recommendations of the British hypertension society. BMJ. 2000 Apr 22;320(7242):1128–34. doi: 10.1136/bmj.320.7242.1128. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1127256/pdf/1128.pdf .PMC1127256 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Comparison of hypertension management outcomes between response group and non-response group.


