Abstract
Background
Extensive global experience shows that rabies pre-exposure prophylaxis (PrEP) through vaccination is effective and well tolerated, yet many travellers opt not to be vaccinated when travelling to rabies-endemic countries. Previous research has identified several factors influencing the choices travellers make to reduce the risk of rabies, including cost, time constraint and perspective on the importance of vaccination. The objectives of this study were to assess travellers’ awareness of rabies and advice-seeking attitudes and to evaluate travel clinics practices regarding rabies pre-travel advice.
Methods
We surveyed individuals aged 18–65 years residing in the UK, Germany, Canada and Sweden who had travelled to rabies-endemic countries between 2013 and 2016 and defined this as the rabies visit-risk sample. The first 850 respondents from the visit-risk sample who had undertaken pre-defined at-risk activities (e.g. contact with animals during the trip) completed an additional 15-min online questionnaire and were included in the activity-risk subsample. We also interviewed travel clinic personnel using a 25-min online or phone questionnaire.
Results
The visit-risk sample included 4678 individuals. Many sought pre-travel health information online (33%) or talked to a family doctor (24%). Within the activity-risk subsample, 83% of travellers were aware of at least a few basic facts about rabies, and 84% could identify at least one correct rabies prevention measure; 49% were aware of a rabies vaccine, however, only 8% reported receiving PrEP vaccination within the past 3 years. Among 180 travel clinic respondents, 21% reported recommending PrEP against rabies to all travellers to rabies-endemic countries. Travel clinics estimated that 81% of travellers complete their travel vaccination schedules and reported sending reminders by e-mails (38%), text (38%), phone calls (37%) or by using vaccination cards (37%).
Conclusions
These findings suggest that although travellers had frequently heard of rabies, awareness of the risks of this serious infectious disease was relatively low.
Keywords: Rabies, endemic, PrEP, vaccination, traveller, travel clinic
Background
Rabies is a viral disease endemic in more than 150 countries and territories, with the highest risk of exposure in Asia and Africa.1–3 Rabies is usually transmitted to humans from bites and licks from infected dogs, although rabies can infect a wide variety of mammals, including bats.3 However, dogs are the principal host in Asia, parts of America and large parts of Africa.3 After clinical symptoms manifest in humans, rabies is almost always fatal.4 Worldwide, there are an estimated 60 000 fatal cases of rabies each year, with about 99% of cases occurring in Africa and Asia.1,3
Many tourists travel to destinations where rabies prevalence is still high and an overall increase in international arrivals has been reported5: between January and April 2018, international arrivals increased by 8% in Asia, 6% in Africa and 3% in the Americas compared with the same period in 2017.6 Rabies exposure poses a risk particularly to travellers to Southeast Asia, including expatriates.7 It has been reported that tourists are inadequately informed about this life-threatening infection;8 in several endemic countries, effective vaccination of dogs is not fully implemented and it is therefore essential to avoid contact with unfamiliar dogs. Because human rabies has also been reported following exposure to non-human primates,9 travellers should also avoid any interactions with these. If bitten, travellers should be clearly informed of the need to seek immediate healthcare to evaluate the need for post-exposure prophylaxis (PEP), in line with official guidelines: wound washing with soap, water and disinfectant and multiple-dose vaccination with or without rabies immune globulin administration. Pre-exposure prophylaxis (PrEP) is also recommended for travellers and consists of three doses of vaccine given within 3 or 4 weeks, according to manufactures’ recommended schedule; although recently updated recommendations from the World Health Organization (WHO) suggest that, based on review of the available evidence, intradermal PrEP can be shortened to 1 week with two-visit regimens.4 If PrEP has been administered and the immune system is primed before exposure, PEP is reduced to wound washing and two doses of vaccine without rabies immune globulin.4
Although global experience with vaccines against rabies show that PrEP is immunogenic and well tolerated, an estimated 70% of travellers to rabies-endemic countries do not receive PrEP vaccine pre-travel.10
We conducted a questionnaire-based, online survey to assess travellers’ awareness of rabies and advice-seeking attitudes and to evaluate travel clinics practices regarding rabies pre-travel advice.
Methods
We conducted an online survey between October and November 2016 with participants from Canada, Germany, Sweden and UK. All respondents were recruited from panels of individuals who had previously agreed to take part in online market research. The survey included travellers to rabies- and/or TBE (tick-born encephalitis)-endemic regions. In this paper, we present the results of the rabies survey.
Respondents aged 18–65 years, who had travelled to rabies- or TBE-endemic countries in the prior 3 years, were invited to complete a 5-min questionnaire (visit-risk sample) and a subset who met criteria for activities with high risk for rabies were selected to take part in an additional 15-min survey (activity-risk sample). High-risk activities were trips to rabies-endemic countries lasting longer than 1 month, or a visit during which the individual had limited access to healthcare or had contact with animals. Eligibility of healthcare providers (HCPs) was assessed via a screening questionnaire, with the inclusion criteria: at least 3-year experience of working in a travel clinic, a minimum of 10 h per week spent working in a travel clinic (10 h per month in Sweden) and responsibility for advising on, and making decisions about, travel vaccination, administering at least five (for the UK and Germany) or three (for Sweden and Canada) rabies vaccines a month.
Briefly, the visit-risk sample answered a series of closed-end questions based on travel destinations and preparation for trips and activities, including knowledge of travel clinics, and awareness of rabies disease and risk, as well as knowledge of preventive measures, including vaccination. The activity-risk subsample proceeded to answer additional closed- and open-ended questions addressing rabies’ risk behaviour and drivers and barriers to vaccination. The travel clinic’s questionnaire assessed practices regarding pre-travel advice, including risk assessment and prevention.
A sample size of >4000 individuals (1000 in each country) for the visit-risk survey and 850 individuals (250 in Canada, Germany and the UK and 100 in Sweden) for the activity-risk survey was planned. Analyses were descriptive and were performed separately for travellers’ and travel clinic data. A more detailed explanation can be found in Supplement 1.
Results
Visit-risk sample
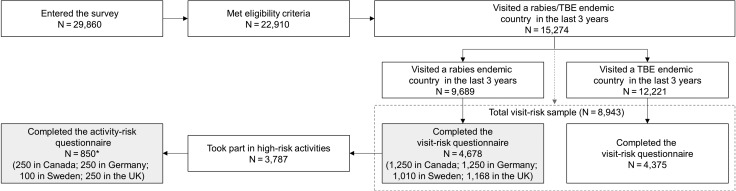
Of the 22 910 eligible individuals, 4678 had visited a rabies-endemic country and completed the visit-risk survey (visit-risk sample) (Figure 1). Demographic and socio-economic characteristics for the visit-risk sample are presented in Supplement 2.
Figure 1.
Flow diagram of screened individuals and respondents. N, number of respondents; TBE, tick-born encephalitis; UK, United Kingdom.
Note: *the first 850 travellers who had visited a rabies-endemic country and had completed the visit-risk questionnaire and met activity-risk eligibility criteria were invited to complete the activity-risk questionnaire.
The most visited rabies-endemic countries were Turkey (20%), Mexico (16%), Thailand (12%), Poland (11%) and Croatia (9%).
In the visit-risk sample, respondents most commonly searched for pre-travel health advice online (33%). Between 20% and 24% of respondents talked to either their family doctor or family/friends who had visited the same country. Smaller proportions read a guide book (16%) or visited a travel clinic (12%), a pharmacist (12%) or a healthcare centre/private clinic/occupational health clinic (13%). Approximately 16% said they had a good knowledge of rabies, while others indicated they knew basic facts (35%) or had some understanding of rabies (32%); only a small proportion (4%) had never heard of the disease. Less than half of the visit-risk travellers (43%) were aware of a rabies vaccine, with awareness being the lowest in Sweden (35%) and the highest in Germany (53%).
Activity-risk subsample
Among the rabies visit-risk sample, 81% (850 travellers) took part in a high-risk activity and completed the activity-risk questionnaire (Figure 1). While travelling, 48% had spent part or the entire trip in remote locations with difficult access to hospitals/medical centres, 55% had contact with animals and 59% spent ≥4 weeks in a rabies-endemic country. Demographics and socio-economic characteristics for the activity-risk subsample are shown in Table 1.
Table 1.
Characteristics of respondents to the activity-risk questionnaire (N = 850)
| Canada | Germany | Sweden | UK | Total | |
|---|---|---|---|---|---|
| Mean age, years | 43 | 39 | 41 | 41 | 41 |
| Age group, % | |||||
| 18–25 years | 8 | 16 | 18 | 10 | 12 |
| 26–35 years | 24 | 29 | 22 | 29 | 27 |
| 36–45 years | 29 | 24 | 21 | 24 | 25 |
| 46–55 years | 19 | 19 | 22 | 19 | 19 |
| 56–65 years | 21 | 11 | 17 | 18 | 17 |
| Male, % | 53 | 54 | 53 | 46 | 51 |
| Travel habits, % | |||||
| Frequent traveller | 36 | 39 | 33 | 36 | 37 |
| Occasional traveller | 37 | 34 | 34 | 36 | 36 |
| Infrequent traveller | 27 | 26 | 33 | 27 | 28 |
| Highest level of formal education | |||||
| Grade school or some high school | 0% | 5% | 2% | 6% | 4% |
| Completed high school | 7% | 24% | 28% | 15% | 17% |
| Technical or trade school/community college | 19% | 9% | 13% | 16% | 14% |
| Community college or university but did not finish | 13% | 26% | 15% | 12% | 17% |
| Complete university degree (e.g. bachelor’s) | 39% | 20% | 31% | 37% | 32% |
| Post-graduate degree (e.g. master’s or PhD) | 22% | 16% | 11% | 15% | 17% |
| Employment status | |||||
| Employed full time | 72% | 66% | 67% | 63% | 67% |
| Employed part time | 10% | 16% | 18% | 18% | 15% |
| Not employed | 6% | 12% | 12% | 10% | 10% |
| Retired | 13% | 6% | 3% | 8% | 8% |
UK, United Kingdom; N, number of respondents; %, percentage of respondents in each category.
The majority (54%) of the visit-risk respondents reported some understanding or good knowledge of rabies. Only 14% reported having felt at risk of rabies on at least one occasion and 22% never felt at risk. Travellers felt at risk of rabies most frequently when travelling to South America, Asia and Africa compared with Europe or North and Central America. However, 26% of travellers to Africa reported not having taken any preventative measures, compared with16% of travellers to North and Central America (Table 2).
Table 2.
Perception of rabies risk and prevention steps taken, by destination region (activity-risk subsample, N = 850)
| Africa | Asia | North/Central America | Europe | South America | |
|---|---|---|---|---|---|
| Perception of risk of catching rabies when travelling to a rabies-endemic region | |||||
| Extremely high risk | 4% | 4% | 2% | 2% | 2% |
| High risk | 9% | 9% | 5% | 6% | 11% |
| Some risk | 27% | 26% | 23% | 17% | 31% |
| At very slight risk | 27% | 30% | 37% | 34% | 31% |
| At no risk at all | 22% | 24% | 29% | 37% | 21% |
| Measures taken to minimize risk of catching rabies | |||||
| Correct measures | |||||
| Avoiding contact with wild animals | 55% | 62% | 59% | 55% | 66% |
| Washing hands after contact with animals | 46% | 52% | 54% | 44% | 54% |
| Avoiding contact with domestic animals | 41% | 48% | 45% | 33% | 43% |
| Rabies PrEP vaccination before travelling | 12% | 14% | 14% | 8% | 23% |
| Incorrect measures | |||||
| Covering up cuts/scratches if travelling in the countryside | 30% | 35% | 30% | 22% | 36% |
| Using antiseptic cream on animal bites or scratches | 33% | 35% | 28% | 22% | 36% |
| No measures taken | 26% | 21% | 16% | 23% | 18% |
N, number of respondents; %, percentage of respondents in each category; PrEP, pre-exposure prophylaxis.
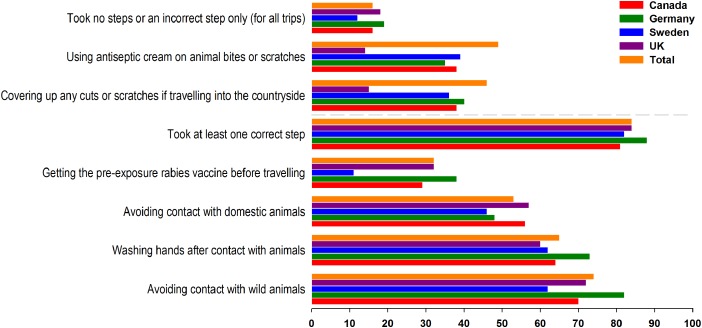
Approximately 90% of activity-risk respondents could identify at least one correct prevention measure; most travellers (78%) were aware of the need to avoid contact with wild or stray animals, to wash the wound when bitten or scratched (47%) or to have the PEP vaccination (40%). Avoiding contact with domestic animals was identified by 43% of respondents, and only 27% were aware of PrEP vaccination. Those with a greater awareness of rabies were also those more likely to have taken appropriate prevention measures; however, 16% of the activity-risk sample did not take any correct steps to minimize their risk (Figure 2).
Figure 2.
Percentage of individuals taking prevention measures prior to trip to rabies-endemic countries, by country (activity-risk sample, N = 850). N, number of respondents; UK, United Kingdom.
Almost half of the respondents (49%) were aware of a rabies vaccine, with awareness being the lowest in Sweden (35%) and the highest in Germany (60%). Similar proportions of respondents were aware of rabies PrEP (29%) and PEP (27%) vaccination. In Sweden, awareness of rabies PrEP and PEP vaccination regimens was 8 and 7%, respectively, whereas in the other three countries, 31–32% and 28–35% were aware of PrEP and PEP, respectively. Most travellers who were aware of PrEP vaccination had heard of it from their doctor (47%). Additional sources were travel clinics (29%), online searches (26%), friends/family (25%) and the general media (17%).
Overall, 17% of the activity-risk subsample reported having previously received a rabies vaccine; 11% had been vaccinated in the 3 years before the survey, with most (8%) having received PrEP rather than PEP (3%). Following a HCP’s [mainly a doctor (54%) or a travel clinic (35%)] advice was the main reported reason for being vaccinated, for 69% of travellers. This was followed by the traveller’s risk awareness (41%), their ‘own peace of mind’ (24%), limited access to medical care during the trip (20%) or plans to engage in high-risk activities (18%) while travelling. Among rabies-vaccinated travellers, 60% reported booking follow-up appointments as a reminder of the vaccination schedule (Table 3).
Table 3.
Vaccination reminder services offered by travel clinics and their use among rabies-vaccinated travellers
| Travellers vaccinated against rabies (activity-risk sample) | Travel clinics | |||
|---|---|---|---|---|
| Reminder | Offered, used | Offered, not used | Not offered | Offered |
| Follow-up appointment (scheduled at initial vaccine dose) | 60% | 5% | 21% | 50% |
| Written on vaccination card/ booklet | 47% | 11% | 27% | Not asked |
| Vaccination wallet reminder card | 35% | 13% | 28% | 37% |
| Reminder phone calls | 23% | 12% | 41% | 37% |
| An email/the text | 22% | 9% | 46% | 38% |
| A web key toola | 19% | 9% | 51% | Not asked |
| A vaccine app for smartphone | 14% | 15% | 48% | 8% |
| A website (requiring registration) | 13% | 14% | 52% | 10% |
%, percentage of respondents in each category.
aA plug-in tool which linked the traveller to a reminder website, provided by a pharmacy.
Travellers cited a low sense of risk (42%), not having thought about it (29%) or not being prompted to have it (25%) as the leading reasons for not getting vaccinated (Table 4).
Table 4.
Main reasons for not taking rabies PrEP vaccination, from the travellers and HCPs’ perspective
| Travellers (activity-risk sample) | Travel clinics | ||||
|---|---|---|---|---|---|
| Reason | % | Reason | % | ||
| All | Visited a HCP before travel | ||||
| N = 753 | Yes (N = 410) | No (N = 343) | |||
| Rabies risk was not high enough to need vaccination | 42 | 43 | 40 | Vaccine is too expensive | 61 |
| Never really thought about it | 29 | 28 | 31 | Travellers do not consider rabies risk high enough | 56 |
| Nobody told them to get vaccinated | 25 | 28 | 23 | Travellers did not have enough time | 52 |
| Lack of time/logistical burden | 20 | 28 | 10 | Travellers have been to the same country before | 40 |
| Safety/vaccine rejection | 19 | 26 | 10 | Vaccine not reimbursed | 36 |
| Their doctor/nurse/pharmacist did not suggest it | 18 | 27 | 7 | Travellers can get the vaccine post-exposure if required | 36 |
| Did not have enough time for it | 18 | 23 | 12 | Vaccination safety/side effects concerns | 33 |
| Had been to the same location before | 15 | 16 | 14 | Vaccine schedule is too arduous | 24 |
| Cost burden | 14 | 21 | 5 | Travellers do not like needles | 24 |
| Did not find out about it until after their travel | 13 | 18 | 8 | Vaccination takes too much time | 23 |
| Their doctor/nurse/pharmacist said it was not needed | 13 | 20 | 4 | Travellers are not sure if vaccine is effective | 21 |
| Travellers do not feel sufficiently informed on the vaccine | 15 | ||||
HCP, healthcare provider; %, percentage of respondents; N, number of respondents in each category
Travel clinics' sample
A total of 180 travel clinic respondents were included in the survey (47 from Canada, 33 from Sweden and 50 from each Germany and the UK). According to these respondents, 39% of travellers visiting the clinics were informed about travel health risks, and 60% were aware of the travel vaccinations needed (with 29% being very well informed and 31% looking for confirmation).
When assessing risks associated with travel, most travel clinic HCPs (72%) reported using their personal judgement. Others used a list of mandatory questions (69%), a health risk questionnaire/form (61%) or online/ electronic tools (35%). Most travel clinics used questions or tools based on guidelines from the WHO (66%) or national health organizations (64%). Only 37% conducted risk assessments based on guidelines developed by the clinic. Most questions asked to travellers when completing a personalized travel risk assessment were related to the trip (e.g. duration, location, planned activities) as well as medical history (Supplement 3).
When asked to prioritize vaccines recommended for travellers at risk of all conditions, most HCPs selected vaccines against yellow fever (62%), hepatitis A (57%) and hepatitis B (56%), followed by rabies (41%), typhoid fever (34%), meningitis (32%) and cholera (19%).
The main reasons HCPs recommended PrEP before travel were the likelihood of contact with animals (59%), restricted access to medical care (48%), remote travel (46%) or travel to a known risk area (46%). Only 21% of HCPs recommended vaccination to all travellers visiting a high-risk country. Most (74%) supported their PrEP recommendation with arguments around the risks and severity of the disease, with only 37% stressing it is fatal and others giving information about risks and complications (26%) or mentioning the severity of the disease (14%).
Most respondents (59%) would recommend PrEP rather than relying on PEP after exposure only (15%). In general, HCPs reported that 81% of travellers complete their travel vaccination schedules and most clinics use several types of reminders to encourage full adherence. Booking follow-up appointments was reported by 50% of HCPs. Other reminders included email (38%), text (38%), phone (37%) or use of vaccination cards (37%) (Table 3).
Travel clinics reported that the cost of the vaccine (61%), low risk perception (56%) and a lack of time (52%) were the main reasons for travellers not getting the vaccine (Table 4).
Discussion
In our study, among 4678 travellers to rabies-endemic countries in the past 3 years, the majority (83%) were aware of at least a few basic facts about rabies but awareness of their own risk to contract and how to prevent this serious infectious disease was relatively low. A perceived lack of risk was most frequently stated as the reason for not being vaccinated among activity-risk travellers, although travel clinic HCPs perceived cost to be the main barrier.
Travellers in the visit-risk sample were most likely to look online for information about travel health or talk to a family doctor. The results suggest that traditional sources of information such as doctors, pharmacists and healthcare centres were secondary to Internet-based sources of traveller information, and that travellers tended to look independently for information rather than ask for it. Further investigation might be needed on the sources of online information that travellers view and/or trust to assess the accuracy and presentation of rabies risks and how best to prevent this potentially fatal disease.
In the activity-risk subsample, over half of the travellers spent ≥4 weeks in a rabies-endemic country, and half reported spending time with limited access to medical care, yet despite this, only 22% reported ever feeling concerned about rabies. This sense of risk and awareness of rabies PrEP vaccination is consistent with previous reports of travellers which showed that the uptake of rabies vaccine was relatively low compared with hepatitis A, typhoid and yellow fever.11–13 We found that perceptions of the risk of rabies varied widely dependent on the travellers’ country of origin with Germans being the most likely to have ever felt at high risk of rabies (22%). Awareness of precautions against rabies was also the highest in Germany. The rabies' risk perception also varied with the visited region and the results of our study suggested that travellers are more likely to feel at risk when visiting Asia and Africa compared with areas that could be perceived more as ‘home territory’ such as Europe or Central America. This was also reflected in an overall awareness of the need to avoid wild animals to reduce the risk exposure to rabies, but a lower awareness of the risk of rabies associated with domestic animals, possibly due to the fact that for example in Europe rabies in dogs has been mostly eliminated.
Across all countries, half of the activity-risk subsamples were aware of a rabies vaccine, yet the rate of PrEP vaccination in the past 3 years was very low (8%). This rate is however consistent with previous reports from a study in international travellers attending a travel clinic in the Netherlands (7.8%)14 or travellers from the USA travelling for 1 month or more in countries with a strong recommendation for rabies (2%).15 In our study, awareness of rabies PrEP and PEP vaccination in Sweden was relatively low compared with the other countries. This is similar with data published by Angelin et al., which sampled people attending a travel clinic in Sweden.11 Although a third of the population stated that Thailand was the travel destination, only 0.5% reported being vaccinated against rabies, compared with 79.4% for hepatitis A, 12.2% for typhoid and 8.9% for yellow fever. The authors highlighted the need to increase rabies vaccination coverage among Swedish travellers to protect against rabies exposure.11 Finally, among the activity-risk subsample, we found approximately a third (28%) of the activity-risk subsample knew that PrEP consisted of three vaccine doses, although 59% of travellers, who had received PrEP, reported that the importance of receiving all doses had been made extremely clear. This suggests that greater awareness about the role and administration of rabies vaccine may be warranted for travellers.
Our results are consistent with previous surveys of travellers that reported a perception of low risk of rabies exposure as the main reason for declining vaccination.11–13,16–19 More specifically, in a US study of 2650 travellers who were eligible for PrEP, 44% refused vaccination, with the majority citing lack of concern as the reason.17 Studies from Demark and Switzerland reported similar findings.12,13 In a US records-based study of travellers that received PEP, it was estimated that about 0.4% of travellers to rabies-endemic countries are at risk of an animal bite.20 In another study of travellers to Southeast Asia, during an average stay of 30 days, among 870 backpackers, 31 (3.6%) reported being licked and 6 (0.7%) being bitten by an animal.21
Although the overall risk of exposure is low, spending time outdoors or in remote rural areas increases the chance of contact with wild animals and there is a need for increased awareness of the preventative measures that can be taken to avoid rabies, including the need to seek healthcare in case of contact with suspect animals, especially for children who might not report having been bitten. This need is supported by the large proportion of travellers in our study who reported that they had never thought about rabies vaccination or had been advised to get vaccinated.
The main limitation of the traveller survey was the selection bias associated with a self-selected sample recruited from an online panel, meaning that the populations cannot be considered as nationally representative. Selection bias was also a limitation of the travel clinic survey. Finally, an additional limitation was that feedback during the recruitment phase with travel clinic respondents suggested that the concept of ‘travel clinics’ does not exist in Sweden, rather travellers are more likely to attend vaccination sessions at their local health centre. Recall bias was a limitation of both surveys.
Conclusions
Our study showed that the perceived risk of exposure to rabies for travellers to endemic regions was low even though the majority of travellers claimed to have sourced advice online or from a HCP. Lack of perceived risk was most frequently stated as the reason for not being vaccinated among travellers, whereas HCPs stated that cost was the main barrier. There was uncertainty among travellers about the risk of being exposed to rabies from wild animals and the need for precautions in countries that are dog rabies-free. This suggests that the type of information and the methods of communication about the risk of rabies, such as online or discussion with HCPs, should be evaluated to identify gaps and to validate travel clinic protocols to ensure that travellers receive accurate and impactful advice.
Supplementary Material
Acknowledgements
The authors would like to thank all study participants and Frédérique Wiot for their contribution to the study. The authors also thank Annick Moon (freelance medical writer c/o GSK Vaccines) and Petronela M. Petrar (XPE Pharma & Sciences c/o GSK Vaccines) for providing medical writing support and Susana Montenegro Gouveia (XPE Pharma & Sciences c/o GSK Vaccines) for assisting with publication management and editorial support. Jamy Feng (MediTech Media, part of Nucleus Global) and Jenny Luxton (MediTech Media, part of Nucleus Global) for medical writing support, David Patching (Synaptik Digital, part of Nucleus Global) for the creative development and Piers Bishop (piersbishop.com) for providing narration.
Authors' Contributions
All authors participated in the conception or design of the study and the interpretation of the results. All authors had full access to the data, were involved in drafting this manuscript, gave final approval before submission and are accountable for all aspects of the work. In addition, Melissa Moodley and Elaine Melander participated in the acquisition/assembling of data and provided statistical expertise. Melissa Moodley, Elaine Melander, Cinzia Marano, Laurence De Moerlooze and Hans Nothdurft performed/supervised the analysis.
Funding
This work was supported by GlaxoSmithKline Biologicals SA and for the development of the manuscript. GlaxoSmithKline Biologicals SA was involved in all stages of the study conduct and analysis and paid all costs associated with developing and publishing the manuscript.
Conflict of interest: C.M. is an employee of GSK and own restricted shares in GSK as a part of her employee remuneration. L.M.D. was an employee of GSK at the time the study was conducted and is now employed by Takeda. M.M., E.M. and H.N. have no conflict of interest to disclose.
Previous presentations in conferences/congresses
Cinzia Marano, Melissa Moodley, Laurence De Moerlooze, Hans Nothdurft. Risky Travel? Travellers’ Awareness of Rabies and Tick-borne Encephalitis and Factors Influencing Their Health Choices. Poster presentation, 15th conference of the International Society of Travel Medicine (CISTM15), Barcelona, Spain, 14–18 May 2017.
References
- 1. Hampson K, Coudeville L, Lembo T et al. . Estimating the global burden of endemic canine rabies. PLoS Negl Trop Dis 2015; 9:e0003709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hampson K, Dushoff J, Cleaveland S et al. . Transmission dynamics and prospects for the elimination of canine rabies. PLoS Biol 2009; 7:e53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization WHO Expert Consultation on Rabies. Second report. World Health Organ Tech Rep Ser. 2013:1–139. [PubMed]
- 4. Rabies vaccines : WHO position paper, April 2018. Wkly Epidemiol Rec. 2018;93:201–20.
- 5. Glaesser D, Kester J, Paulose H, Alizadeh A, Valentin B. Global travel patterns: an overview. J Travel Med 2017; 24(4), doi: 10.1093/jtm/tax007 [DOI] [PubMed] [Google Scholar]
- 6. UNWTO World Tourism Barometer and Statistical Annex, June 2018. https://www.e-unwto.org/doi/abs/10.18111/wtobarometereng.2018.16.1.3 (12 July 2018, date last accessed).
- 7. Tarantola A, Mey C, Ly S et al. . A confirmed rabies case in a French resident in Cambodia, June 2015. J Travel Med 2016; 23(2), doi: 10.1093/jtm/tav012 [DOI] [PubMed] [Google Scholar]
- 8. Piyaphanee W, Kittitrakul C, Lawpoolsri S et al. . Risk of potentially rabid animal exposure among foreign travelers in Southeast Asia. PLoS Negl Trop Dis 2012; 6:e1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mani RS, Sundara Raju YG, Ramana PV, Anand AM, Prakash BB. Human rabies following a non-human primate bite in India. J Travel Med 2016; 23(3), doi: 10.1093/jtm/taw007 [DOI] [PubMed] [Google Scholar]
- 10. Gautret P, Parola P. Rabies in travelers. Curr Infect Dis Rep 2014; 16:394. [DOI] [PubMed] [Google Scholar]
- 11. Angelin M, Evengard B, Palmgren H. Travel and vaccination patterns: a report from a travel medicine clinic in northern Sweden. Scand J Infect Dis 2011; 43:714–20. [DOI] [PubMed] [Google Scholar]
- 12. Buhler S, Ruegg R, Steffen R, Hatz C, Jaeger VK. A profile of travelers—an analysis from a large Swiss travel clinic. J Travel Med 2014; 21:324–31. [DOI] [PubMed] [Google Scholar]
- 13. Christiansen AH, Rodriguez AB, Nielsen J, Cowan SA. Should travellers to rabies-endemic countries be pre-exposure vaccinated? An assessment of post-exposure prophylaxis and pre-exposure prophylaxis given to Danes travelling to rabies-endemic countries 2000–12. J Travel Med 2016; 23(4), doi: 10.1093/jtm/taw022 [DOI] [PubMed] [Google Scholar]
- 14. Wieten RW, van der Schalie M, Visser BJ, Grobusch MP, van Vugt M. Risk factors and pre-travel healthcare of international travellers attending a Dutch travel clinic: a cross-sectional analysis. Travel Med Infect Dis 2014; 12:511–24. [DOI] [PubMed] [Google Scholar]
- 15. Dolan SB, Jentes ES, Sotir MJ et al. . Pre-exposure rabies vaccination among US international travelers: findings from the global TravEpiNet consortium. Vector Borne Zoonotic Dis 2014; 14:160–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Altmann M, Parola P, Delmont J, Brouqui P, Gautret P. Knowledge, attitudes, and practices of French travelers from Marseille regarding rabies risk and prevention. J Travel Med 2009; 16:107–11. [DOI] [PubMed] [Google Scholar]
- 17. Lammert SM, Rao SR, Jentes ES et al. . Refusal of recommended travel-related vaccines among U.S. international travellers in Global TravEpiNet. J Travel Med 2016; 24(1), doi: 10.1093/jtm/taw075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ross RS, Wolters B, Viazov SO, Roggendorf M. Awareness of rabies risks and knowledge about preventive measures among experienced German travel health advisors. J Travel Med 2006; 13:261–7. [DOI] [PubMed] [Google Scholar]
- 19. Dahlgren AL, DeRoo L, Steffen R. Prevention of travel-related infectious diseases: knowledge, practices and attitudes of Swedish travellers. Scand J Infect Dis 2006; 38:1074–80. [DOI] [PubMed] [Google Scholar]
- 20. Gautret P, Parola P. Rabies vaccination for international travelers. Vaccine 2012; 30:126–33. [DOI] [PubMed] [Google Scholar]
- 21. Piyaphanee W, Shantavasinkul P, Phumratanaprapin W et al. . Rabies exposure risk among foreign backpackers in Southeast Asia. Am J Trop Med Hyg 2010; 82:1168–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.