Figure 1. Microbial-host meta-organismal pathway linking dietary metabolism, gut microbiota, and cardio-renal disease progression.
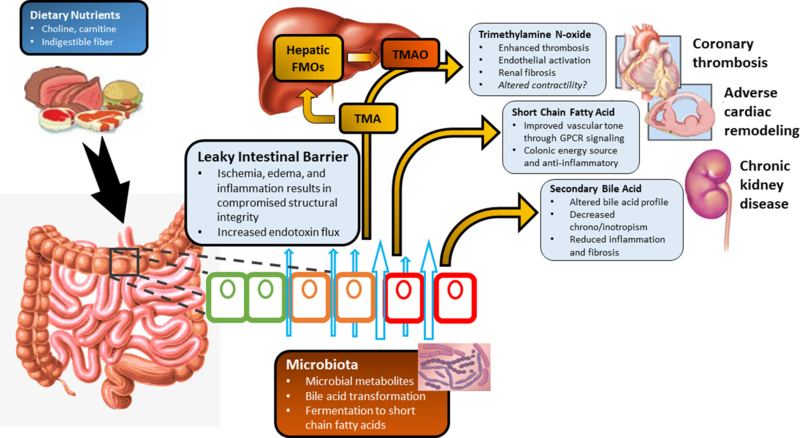
Legend: Poor cardiac output in heart failure results in intestinal ischemia, edema, and inflammation which leads to a “leaky” intestinal barrier. This allows for increased passage of inflammatory bacterial products to enter the bloodstream causing chronic low-grade inflammation. Furthermore, this alters the intestinal environment and impacts both the normal microbial community which resides in the gut and subsequently, the metabolic products from these bacteria. The metabolic pathways include fermentation of indigestible fiber to short chain fatty acids which have protective properties reducing inflammation and improving vascular tone. Dietary sources including choline, phosphatidylcholine, l-carnitine and other methylamine-containing nutrients provide substrates for microbiota mediated production of trimethylamine (TMA). TMA then enters the portal circulation and is converted by the hepatic host flavin-containing monooxygenase (FMO) family of enzymes to trimethylamine n-oxide (TMAO). TMAO can promote the development of atherogenesis, thrombosis, kidney disease, and heart failure. Additionally, the bacterial transformation of bile acids can result in altered bile acid profiles which then can affect systemic inflammatory and fibrotic processes. Collectively, these processes can influence the individual susceptibility, severity of heart failure.
