Highlights
-
•
Calcification at the linea aspera is a differential for hip/thigh pain.
-
•
Imaging should commence with plain radiographs, and also include the distal femur.
-
•
Smaller calcific deposits can be obscured on anteroposterior projection, necessitating additional views.
-
•
Calcific tendo-enthesopathy is associated with osteolysis but no soft tissue mass.
Keywords: Calcification, Osteolysis, Tendon, Femur, Imaging
Abstract
This review aims to consolidate the published demographics, clinical and radiological features of calcific tendonitis affecting the linea aspera. Using the PRISMA protocol, 55 clinical cases were extracted from 19 shortlisted papers. In a patient presenting with thigh and/or hip pain, radiologic evaluation should commence with plain radiographs; subsequent cross-sectional imaging, if necessary. Our review of the literature indicates that calcific tendonitis can be safely diagnosed when intratendinous calcification is observed in the region of the linea aspera with cortical erosion but no discrete soft tissue mass.
1. Introduction
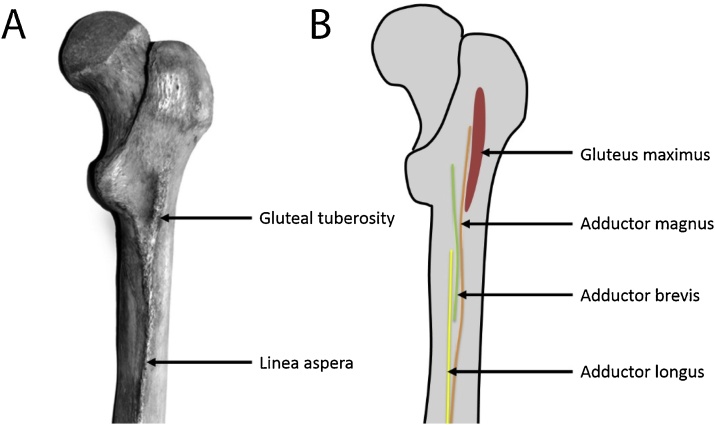
The linea aspera is a fibrous entheseal site for the insertion of the gluteus maximus and adductor muscles [1,2] (Fig. 1). Calcification adjacent to the linea aspera can be caused by calcific tendonitis or a calcific enthesopathy. Calcific tendonitis is a benign, self-limiting pathological process defined by calcium hydroxyapatite crystal deposition in tendons with an unknown aetiology. It is a common disorder predominantly occurring in the tendons around the shoulder with an overall incidence of 3% [3] in the adult population and 7% [4] for radiologically evident disease. It has a peak age of incidence between 30 and 50 years and a female predilection. Calcific tendonitis most commonly affects the shoulder, and in decreasing order of frequency, the hip, elbow, wrist and knee. Calcific tendonitis of structures inserting into the linea aspera, gluteus maximus and the adductor muscles, are much less common. Calcific enthesopathies are often associated with seronegative arthropathies or chronic traction injuries. They can however be idiopathic. The two conditions can be difficult to distinguish with plain radiographs and can appear aggressive on cross-sectional imaging leading to unnecessary interventions.
Fig. 1.
Photograph of the posterior aspect of a cadaveric femur (A) and corresponding line drawing (B) demonstrating the linea aspera as a raised bony ridge with the insertion of the gluteus maximus and adductor muscles.
This review aims to consolidate the published demographics, clinical and radiological features of calcific tendonitis affecting the linea aspera identified through a systematic narrative review.
2. Materials and methods
A systematic review of the literature was performed using the PRISMA protocol.
2.1. Search strategy
Articles were obtained by searching Pubmed, Google and Google Scholar using the following search words “linea aspera”, “calci- adductor”, “calci- glute-”, “calci- tendon-“, “calci- tendin-“, “calci- enthes-”; with “- “referring to the truncated form of the search word. Searches were supplemented by scanning bibliographies of included articles, review articles, and conference proceedings and by contacting an expert in the field.
2.2. Selection criteria
Abstracts were retained if they reported on calcium deposition on the upper thigh or buttock. Full papers were retrieved, independently reviewed by 2 reviewers and shortlisted. The shortlisting criteria were that papers had to be written in English and were case reports or case series reporting on calcification affecting the gluteus maximus and adductor muscles.
2.3. Data extraction
Data were extracted by a single author, and included patient’s age, gender, location of calcification, clinical presentation, laboratory values, imaging findings, intervention, outcomes (radiologic and clinical) and follow-up length.
3. Results
The search yielded 79 abstracts. Of these, 15 were excluded as they were non-English. Full texts of the remaining 64 papers were obtained. A further 45 were excluded for not meeting the eligibility criteria, leaving 19 papers [[5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23]] in the review on which data extraction was performed. In total, 60 papers were excluded from the review for the following reasons: 15 non-English; 15 reviews of literature; 30 not tendonitis or enthesopathy.
3.1. Patient characteristics
55 clinical cases were extracted from the 19 articles [[5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23]] reviewed. The affected adults were aged between 30 to 68 years. In 52 patients, the gender was known, giving a female to male preponderance of 1.9:1 (Table 1). In 42 patients, the ages of individual patients were known, with a mean age of 52 years (Table 1). 13 patients were excluded from the mean age calculation as their ages were given as a range, instead of a specific value.
Table 1.
Summary of results.
| Patient demographics and characteristics | |
| Age: mean; range | 52 (n = 42)*; 30-68 |
| Sex: % female | 65 (n = 52)* |
| Muscle affected (n = 46)* | |
| Gluteus maximus: % | 93 (n = 43)† |
| Adductor magnus: % | 4 (n = 2)† |
| Adductor longus: % | 0 |
| Adductor brevis: % | 2 (n = 1)† |
| Radiological features | |
| Soft tissue calcification on the plain radiograph: % | 96 (n = 55)* |
| Cortical erosion on CT: % | 75 (n = 32)* |
| Soft tissue oedema: % | 75 (n = 20)* |
| Bone marrow oedema: % | 15 (n = 20)* |
Total number of patients.
Number of patients.
3.2. Clinical presentation
3.2.1. Side and site
In 44 patients, the affected side was known. The right side was affected in 24 while the left was affected in 20 patients. In 46 patients, the specific site was known (Table 1). The gluteus maximus tendon was affected in 43 patients, the adductor magnus in 2 patients and the adductor brevis in 1 patient. In 9 patients, either the gluteus maximus or the adductors was affected, the exact location was not mentioned. The adductor longus was spared.
3.2.2. Clinical symptoms
Of 55 patients, 53 were symptomatic with pain. The location of pain was as follows: 25 thigh pain, 4 hip pain, 2 back pain, 2 buttock pain, 7 thigh and hip pain, 5 thigh or hip pain, 8 non-specific pain.
The duration of symptoms was variable, with an acute onset of a few days to chronic pain lasting years. Most reports described patients as being systemically well but more acute presentations were accompanied by prodromal symptoms in 2 patients. In 35 patients, where the duration of symptoms was reported, the median was 2 months (range: 3 days to 2 years).
Regardless of whether the calcification is in the distal adductor or gluteus maximus attachment, patients usually presented with hip or upper posterior thigh pain that may be accompanied by focal tenderness on palpation (n = 24). Other less common symptom presentation include back or buttock pain (n = 4) with palpation tenderness (n = 1) or hip stiffness (n = 1).
3.2.3. Clinical signs
24 out of 30 patients reported local tenderness on palpation (over the gluteal tubercle; posterior and lateral thigh; along sciatic nerve). The range of movement was affected in 2 patients while there was both tenderness and movement restriction in 4 patients.
3.3. Imaging characteristics
3.3.1. Plain radiography
The abnormality seen on the radiographs (Fig. 2, Fig. 4, Fig. 6, Fig. 8) was described with the following words “calcification”, “calcific density/ deposit/ lesion/ opacity”, “mineralisation” and “ossification”; with “calcification” being the most common noun used in 33 patients. In 2 patients, the above words were not mentioned as 1 patient’s radiograph showed a focal cortical lucency while the other had a radiograph which was reported as normal (Table 1). In the latter, tendon calcification was later seen on CT; with a corresponding focus of increased uptake on the bone scan.
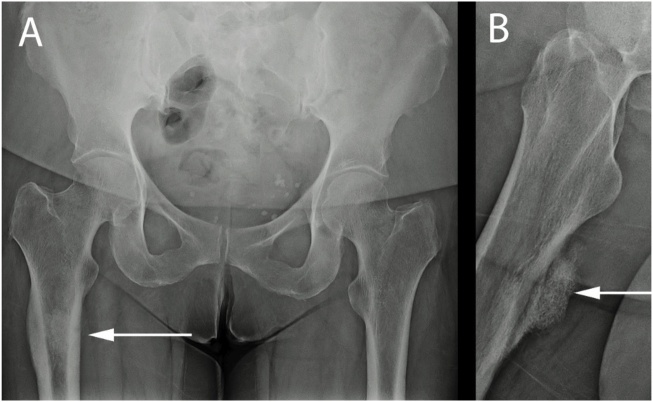
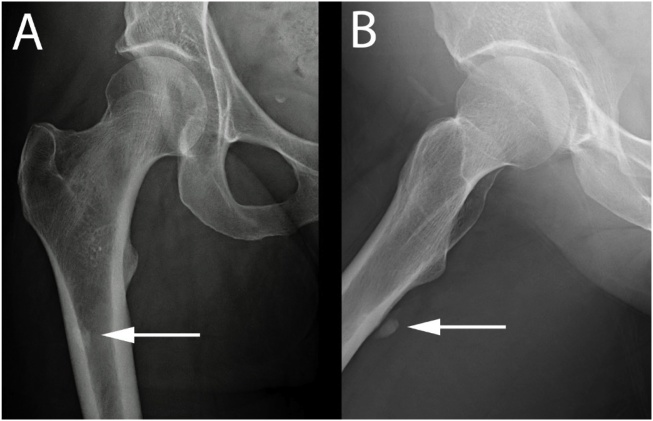
Fig. 2.
Anteroposterior radiograph of the pelvis (A) and lateral radiograph of the right hip (B) in a 62 year old female, with gradually increasing right thigh pain, demonstrate thickening of both medial and lateral femoral cortices in the diametaphyseal junction, with a 4.5 cm partly mineralised lesion arising from the anterior aspect of the proximal femur with periosteal thickening.
Fig. 4.
Anteroposterior (A) and lateral radiographs of the left hip (B) in a 67 year old male, with left hip pain and stiffness, demonstrate a lobulated area of calcification (partially seen in (B)) overlying the posterior aspect of the proximal femoral diametaphysis with no periosteal reaction.
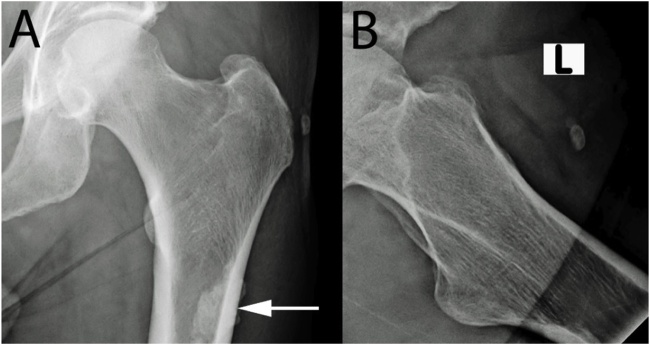
Fig. 6.
Anteroposterior (A) and lateral radiographs of the right hip (B) in a 61 year old female, with pain in the posterior aspect of the right proximal femur, demonstrate amorphous calcification in the proximal femur posteriorly, better visualised on the lateral radiograph.
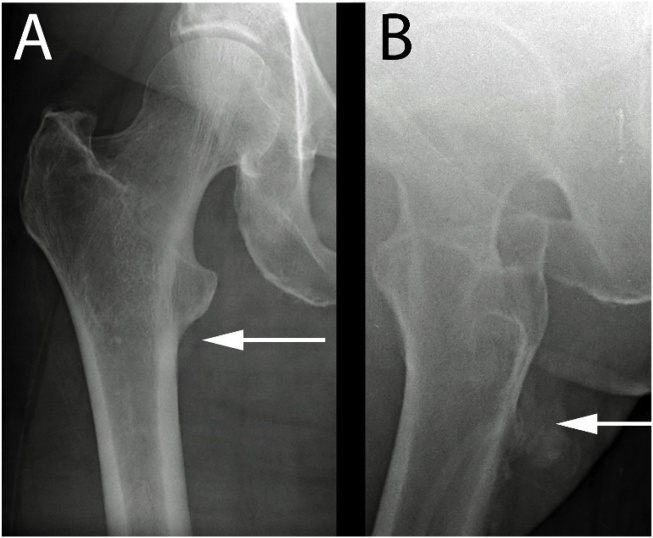
Fig. 8.
Anteroposterior (A) and lateral radiographs of the right hip (B) in a 57 year old female, with right posterior thigh pain that is worse on pressure, demonstrate new bone formation/ calcification in the proximal femur posteriorly.
Cortical changes at the site of the calcification were reported in 12 cases. These changes were reported as “cortical lucency/cystic change” in 3, “cortical erosion” in 7, “cortical irregularity” in 1 and “cortical thickening” in 1.
The radiographic location of the abnormality in respect to the proximal femur was reported in 37 cases. In respect to the proximal femur, the abnormality was being described as “anterior” in 1, “posterior” in 22, “lateral” in 4, “posterolateral” in 9 and “posteromedial” in 1. The abnormality which was reported as being anterior to the proximal femur was later confirmed on cross-sectional imaging to be posteromedial.
3.3.2. Cross-sectional imaging
32 out of 43 patients had at least 1 additional form of imaging other than the plain radiograph. CT was the most popular cross-sectional examination (n = 32), followed by MRI (n = 20) and then radionuclide bone scintigraphy (n = 17).
The abnormality was seen in all patients who had a CT (Fig. 3, Fig. 5, Fig. 7). It was described with the following words “calcification”, “mineralisation”, “ossification” and “enthesophyte”; with calcification being the most common noun used in 26 patients. The nature of the calcification was further characterised as being “amorphous”, “inhomogeneous”; with a “punctate”, “globular”, “rounded”, “plurilobulated”, “comet-tail”, “flame-like” appearance; within the soft tissues of the “muscle”, “tendon”, “enthesis”.
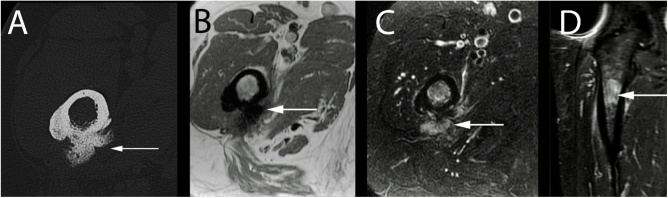
Fig. 3.
Axial CT (A); axial T1-weighted (B), axial (C) and coronal T2-weighted fat suppressed (D) MRI of the right proximal thigh in a 62 year old female, with gradually increasing right thigh pain, demonstrate focal bony proliferation with peri-osseous oedema and mild bone marrow oedema, with no features of a neoplastic process.
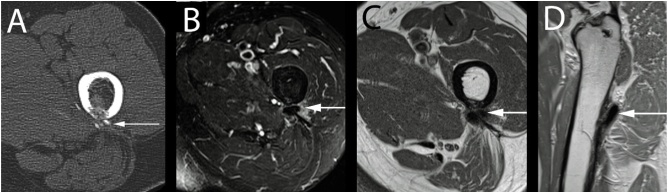
Fig. 5.
Axial CT (A) in a 67 year old male, with left hip pain and stiffness, demonstrates cortical involvement adjacent to calcification arising from the muscular septum between the vastus lateralis and gluteus maximus at the insertion to the linea aspera. Axial T2-weighted fat suppressed (B), axial T1-weighted (C) and sagittal T1-weighted (D) MRI sequences of the left proximal thigh in the same patient demonstrate the focal calcification adjacent to the linea aspera as previously described with perilesional soft tissue oedema.
Fig. 7.
Axial CT (A); axial T1-weighted (B) and T2-weighted fat suppressed (C) MR sequences of the right hip in a 61 year old female, with pain in the posterior aspect of the right proximal femur, demonstrate patchy linear calcification within the adductor magnus with marked oedema.
Associated cortical abnormalities were reported in 75% (n = 24) of CT examinations (Table 1, Fig. 5). These changes were reported as being focal “cortical thinning”, “cortical erosion”, “cortical defect” or “cystic lesion of the cortex”.
In patients who had an MRI, the findings can be divided into perilesional soft tissue, bone marrow or lesion-based changes. Soft tissue changes were most commonly mentioned in 85% (n = 17) of patients. In a further 88% (n = 15) of these patients, there was high T2 signal within the affected muscle (gluteus maximus, adductors) and spreading into the adjacent muscles (vastus, quadratus femoris), in keeping with soft tissue oedema (Table 1; Fig 5, Fig. 7, Fig. 9). No mass effect or soft tissue mass was identified. The bone marrow changes were only commented on in 40% (n = 8) of patients. 5 patients had a normal bone marrow while 3 had bone marrow oedema, in the region of the abnormality (Table 1, Fig. 3). The lesion was described to be of low to intermediate T1 signal in 6 patients, in keeping with calcification or fibrous tissue (Fig. 5, Fig. 7, Fig. 9) .
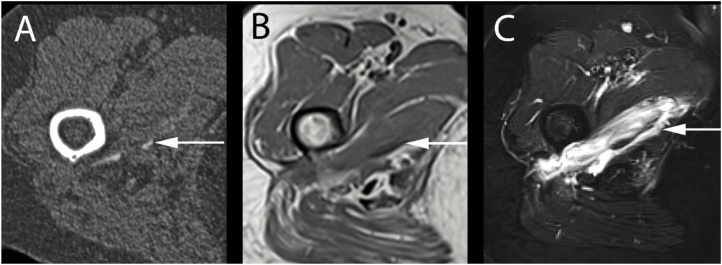
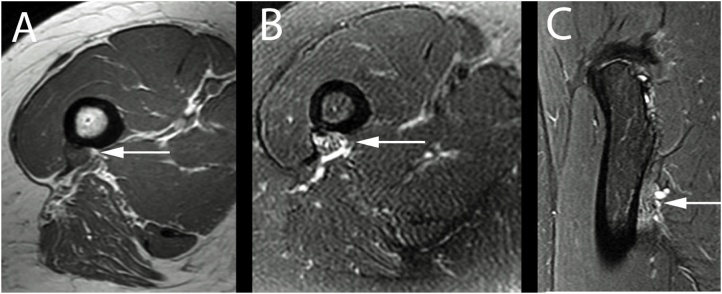
Fig. 9.
Axial T1-weighted (A) and T2-weighted fat suppressed (B) and sagittal T2-weighted fat suppressed (C) MR sequences of the right hip in a 57 year old female, with right posterior thigh pain that is worse on pressure, demonstrate an area of thickening and intermediate T1 signal at the insertion of the gluteus maximus/lateral intramuscular septum on the posterior femur with perilesional oedema. No cortical erosion or bone marrow oedema.
There was focal increased uptake over the region of abnormality in all 17 patients who had a radionuclide study.
3.3.3. Follow up
The follow-up data is limited, only available in 58% (n = 32) of patients with a median length of time of 2 years (range: 2 weeks to 9 years). Seven patients were reported to have had repeat imaging. Radiographic resolution was recorded in 1 patient, with absence of the soft tissue calcification in 2 months. The other 6 demonstrated either stable appearances or some decrease in size of the calcification.
Clinical follow-up was recorded in 41 patients, with complete or near-complete symptom resolution after intervention. 42 patients had some form of clinical intervention which varied from oral anti-inflammatories, steroids or antibiotics; single or multiple, blind or image-guided steroid injections, image-guided or excisional biopsy, to radical excision with allograft. The time taken to notice an improvement in symptoms is subjective and often not recorded. There is also limited information regarding the time to symptom resolution as most authors did not quantify this.
4. Discussion
The results of this study allow us to describe the demographic, clinical and radiological characteristics of reported cases of calcific enthesopathy around the linea aspera; an uncommon condition with variable descriptors.
Involvement of the gluteus maximus is more commonly reported than the adductor muscles. Similar to calcific tendonitis of the shoulder, this condition was most often reported in middle-aged females. Patients were generally systematically well and presented with thigh or hip pain, which may be accompanied by focal tenderness on palpation and reduced range of movement. Initial radiographs of the hip demonstrate calcification posterior to the proximal femur with associated cortical changes seen in about a quarter of cases. CT was the most common cross-sectional imaging used to confirm the abnormality and also to provide further detail on the nature of the calcification. CT was reported to demonstrate calcification more commonly than plain radiographs however as there is usually an interval between the two tests this might account for some of the increased conspicuity. MRI demonstrated perilesional soft-tissue oedema extending into the adjacent bone marrow with low to intermediate T1 signal of the lesion. Radionuclide bone scintigraphy demonstrated focal increased uptake over the lesion.
The reports in this study span a period of three decades and yet are limited to single case reports or short case series. This suggests that this is an uncommon condition although the true prevalence is not known. It may be a more commonly occurring condition than the rarity of these reports suggest if it is underdiagnosed. Calcific enthesitis tends to be a cyclical phenomenon with periods where there is no calcification and yet the patients are symptomatic and vice versa and therefore radiographs may be normal and the diagnosis missed. Alternatively the calcification may be misinterpreted as a benign enostosis or enchondroma if lateral views are not available. A further reason for underdiagnosing the condition may lie with the margins of a conventional hip radiograph. The linea aspera extends some way distally along the femoral diaphysis and may not be included in a routine hip radiograph where the inferior margin often lies just distal to the lesser trochanter. This excludes the mid to distal length of the linea aspera where the adductor muscles also attach. These distal calcifications will not be observed unless additional full femoral views are obtained. Calcification of the linea aspera on an anteroposterior projection is usually seen below the greater trochanter, overlying the femoral cortex and a portion of the medullary cavity. Larger deposits project laterally into the soft tissues and are easily visualised whereas smaller deposits can be obscured by the femur on an anteroposterior projection. Therefore an additional lateral or frog-lateral view may be required to complete an adequate radiographic examination.
This study has demonstrated that the terminology used in the published literature is variable. An explanation for part of this variability is that there are probably two distinct pathological processes that are presenting with similar clinical and radiological features.
The first is primary inflammation of the enthesis, caused most commonly by chronic traction injuries or seronegative arthropathies, presenting on radiographs as cortical erosion and reactive sclerosis, which may be accompanied by the formation of irregular enthesophytes. The second process is calcific tendinosis, where hydroxyapatite crystals accumulate in a relatively avascular portion of the tendon, and is separate from the adjacent cortex. However this avascular portion of the tendon is close to the enthesis and as the crystalline deposits lead to necrosis, loss of fibrous structure and surrounding inflammatory changes [24], these can produce secondary changes in the nearby bone via the enthesis. In these cases it may be more difficult to differentiate an enthesopathy from calcific tendonitis. Both conditions involve the tendon-entheseal-bone complex and are not necessarily confined to the enthesis or the tendon as their names imply. Soft tissue calcification or ossification without cortical involvement can be assumed to be a calcific tendinopathy rather than an enthesopathy but the results of this study suggest that this is often not possible.
The gluteus maximus muscle is the more commonly reported affected muscle compared to the adductor muscles. However, there is room for inaccuracy here because of the close proximity of the various muscle groups inserting into the linea aspera, combined with extensive inflammation which makes precise muscle identification difficult even on cross-sectional imaging. This probably does not matter very much as knowledge of the exact anatomical location of the disease need not affect the diagnosis or management of the patient.
CT was the most commonly reported second line imaging modality. CT has an advantage over MRI in confirming the presence and location of soft tissue calcifications and evaluating the underlying cortex. MRI is more sensitive to inflammatory changes but most importantly can be used to exclude the presence of a soft tissue mass and evaluate the bone marrow when there are aggressive cortical changes. Increased radionuclide uptake on the bone scintigraphy was present on all reported nuclear medicine studies but contributed little to the diagnosis demonstrating increased bone turnover that could represent a range of benign to malignant causes.
The main limitations of this study relate to the nature of the published material available. The submission and publication of cases reports and case series is not a systematic process and therefore is open to selection bias. The summary data from this study reflects the published material available but does not necessarily reflect the true prevalence of the disease and its radiological features. However as this appears to be an uncommon condition large systematic case series are unlikely and therefore this study summarizes the best available evidence for this condition in a narrative review, which is appropriate to the nature of the evidence.
The linea aspera has not been reported as a site that is commonly involved in the musculoskeletal manifestations of systemic diseases such as spondyloarthritis, acromegaly, hyper and hypoparathyroidism, or fluorosis. Nor was there any mention of any such underlying diseases in the medical histories of the cases listed. Therefore an assumption of this study is that in the cases reviewed the calcification of the linea aspera was an isolated clinical occurrence.
In conclusion, calcification at the linea aspera insertion of the gluteus maximus or adductor muscles may be present in patients who presents with hip or thigh pain. Cortical erosion is a common finding on plain radiography or CT. MRI can demonstrate the site of inflammation and the absence of tumour. Confirming the diagnosis of a calcific enthesopathy can obviate the need for unnecessary diagnostic interventions. Enthesopathies and calcific tendinopathies can be difficult to differentiate at the tendon-enthesis-bone complex.
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ejro.2018.12.002.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Mann R.W., Hunt D.R. 3rd ed. Charles C Thomas Publisher; 2013. Photographic Regional Atlas of Bone Disease: A Guide to Pathologic and Normal Variation in the Human Skeleton. [Google Scholar]
- 2.Apostolakos J., Durant T.J., Dwyer C.R., Russell R.P., Weinreb J.H., Alaee F. The enthesis: a review of the tendon-to-bone insertion. Muscles Ligaments Tendons J. 2014;4:333–342. [PMC free article] [PubMed] [Google Scholar]
- 3.Bosworth B. Calcium deposits in the shoulder and subacromial bursitis. A survey of 12,122 shoulders. JAMA. 1941:2477–2482. [Google Scholar]
- 4.Welfling J., Kahn M.F., Desroy M., Paolaggi J.B., de Sèze S. Calcifications of the shoulder. II. The disease of multiple tendinous calcifications. Rev. Rhum. Mal. Ostéo-Articul. 1965;32:325–334. [PubMed] [Google Scholar]
- 5.Choudur H.N., Munk P.L. Image-guided corticosteroid injection of calcific tendonitis of gluteus maximus. J. Clin. Rheumatol. Pract. Rep. Rheum. Musculoskelet. Dis. 2006;12:176–178. doi: 10.1097/01.rhu.0000230457.51606.62. [DOI] [PubMed] [Google Scholar]
- 6.Strokon A., Archer K., Mourad M., Van Der Wall H. Scintigraphy of gluteal tendonopathy. Clin. Nucl. Med. 2003;28:128–129. doi: 10.1097/01.RLU.0000048943.67406.32. [DOI] [PubMed] [Google Scholar]
- 7.Thomason H.C., Bos G.D., Renner J.B. Calcifying tendinitis of the gluteus maximus. Am. J. Orthop. Belle Mead NJ. 2001;30:757–758. [PubMed] [Google Scholar]
- 8.Kraemer E.J., El-Khoury G.Y. Atypical calcific tendinitis with cortical erosions. Skeletal Radiol. 2000;29:690–696. doi: 10.1007/s002560000278. [DOI] [PubMed] [Google Scholar]
- 9.Hottat N., Fumière E., Delcour C. Calcific tendinitis of the gluteus maximus tendon: CT findings. Eur. Radiol. 1999;9:1104–1106. doi: 10.1007/s003300050799. [DOI] [PubMed] [Google Scholar]
- 10.Thornton M.J., Harries S.R., Hughes P.M., Whitehouse R., Carradine S. Calcific tendinitis of the gluteus maximus tendon with abnormalities of cortical bone. Clin. Radiol. 1998;53:296–301. doi: 10.1016/s0009-9260(98)80131-1. [DOI] [PubMed] [Google Scholar]
- 11.Ferraro A., Mercuri M., Ruggieri P., Casadei R. Calcific tendinitis of the gluteus maximus. Chir. Organi Mov. 1995;80:335–340. [PubMed] [Google Scholar]
- 12.Mizutani H., Ohba S., Mizutani M., Otake S., Otsuka T., Nakamura T. Calcific tendinitis of the gluteus maximus tendon with cortical bone erosion: CT findings. J. Comput. Assist. Tomogr. 1994;18:310–312. doi: 10.1097/00004728-199403000-00030. [DOI] [PubMed] [Google Scholar]
- 13.Hayes C.W., Rosenthal D.I., Plata M.J., Hudson T.M. Calcific tendinitis in unusual sites associated with cortical bone erosion. AJR Am. J. Roentgenol. 1987;149:967–970. doi: 10.2214/ajr.149.5.967. [DOI] [PubMed] [Google Scholar]
- 14.Wepfer J.F., Reed J.G., Cullen G.M., McDevitt W.P. Calcific tendinitis of the gluteus maximus tendon (gluteus maximus tendinitis) Skeletal Radiol. 1983;9:198–200. doi: 10.1007/BF00352555. [DOI] [PubMed] [Google Scholar]
- 15.Berney J.W. Calcifying peritendinitis of the gluteus maximus tendon. Radiology. 1972;102:517–518. doi: 10.1148/102.3.517. [DOI] [PubMed] [Google Scholar]
- 16.Fritz P., Bardin T., Laredo J.D., Ziza J.M., D’Anglejan G., Lansaman J. Paradiaphyseal calcific tendinitis with cortical bone erosion. Arthritis Rheum. 1994;37:718–723. doi: 10.1002/art.1780370516. [DOI] [PubMed] [Google Scholar]
- 17.Seeger L.L., Butler D.L., Eckardt J.J., Layfield L., Adams J.S. Tumoral calcinosis-like lesion of the proximal linea aspera. Skeletal Radiol. 1990;19:579–583. doi: 10.1007/BF00241280. [DOI] [PubMed] [Google Scholar]
- 18.Tamangani J., Davies A.M., James S.L.J., Christie-Large M. Calcific tendonitis of the adductor brevis insertion. Clin. Radiol. 2009;64:940–943. doi: 10.1016/j.crad.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 19.Hodge J.C., Schneider R., Freiberger R.H., Magid S.K. Calcific tendinitis in the proximal thigh. Arthritis Rheum. 1993;36:1476–1482. doi: 10.1002/art.1780361021. [DOI] [PubMed] [Google Scholar]
- 20.Gong Y., Yang C., Jingyu W., Liu J., Qi X. Calcific tendinitis of the gluteus maximus tendon with sciatic pain. Eur. J. Radiol. Extra. 2010;76:e59–60. [Google Scholar]
- 21.Murphy D. 2011. EURORAD - Radiologic Teaching Files [Internet]. Case 9701 Calcific tendonitis of the gluteus maximus insertion. [cited 2015 Aug 10]. Available from: http://www.eurorad.org/eurorad/case.php?id=9701. [Google Scholar]
- 22.Singh J.R., Yip K. Gluteus maximus calcific tendonosis: a rare cause of sciatic pain. Am. J. Phys. Med. Rehabil. Assoc. Acad. Physiatr. 2015;94(Feb. (2)):165–167. doi: 10.1097/PHM.0000000000000190. [DOI] [PubMed] [Google Scholar]
- 23.Low S.B.L., Toms A. Educational exhibit. European Society of Radiology; Vienna: 2016. Calcific tendonitis affecting the linea aspera: a case series and systematic narrative review. [Google Scholar]
- 24.Resnick D., Niwayama G. Entheses and enthesopathy. Anatomical, pathological, and radiological correlation. Radiology. 1983;146:1–9. doi: 10.1148/radiology.146.1.6849029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.