Abstract
Background:
Medial ulnar collateral ligament (UCL) reconstruction is a common procedure performed among Major League Baseball (MLB) pitchers. The etiology of UCL injury is complex and is not entirely understood.
Hypothesis:
To better understand risk factors for requiring UCL reconstruction, we hypothesized that pitchers who eventually undergo the procedure will exhibit different throwing mechanics as measured by pitch-tracking data points, such as velocity and release location.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
Pitch-tracking and demographic data were gathered for 140 MLB pitchers who had undergone UCL reconstruction between the 2010 and 2017 seasons. Pitch type, release location, and velocity were compared between the surgical cohort and a matched-control cohort.
Results:
When compared with controls, the mean pitch release location for pitchers who required UCL reconstruction was 12.2 cm more lateral in the year immediately preceding surgery (P = .001). Furthermore, within the surgical cohort, the horizontal release location was 3.4 cm more lateral immediately preceding surgery compared with 2 years earlier (P = .036). Binary logistic regression indicated an odds ratio of 0.51, suggesting a roughly 5% increased odds of UCL reconstruction for every 10 cm of increased lateral release location (P = .048). Both the surgical and the control cohorts threw similar rates of fastballs and had similar mean pitch velocity and fastball velocity. Control pitchers displayed a significant decrease over time in mean pitch velocity (P = .005) and mean fastball velocity, while pitchers in the UCL reconstruction cohort did not (P = .012).
Conclusion:
Pitch tracking indicates that the mean release point is more lateral in pitchers preceding UCL reconstruction as compared with controls, suggesting that a more lateral pitch release location is an independent risk factor for UCL injury and reconstruction.
Keywords: MLB, pitchers, Tommy John surgery, UCL, pitch tracking
Medial ulnar collateral ligament (UCL) reconstruction (UCLR) is a common procedure performed for elite-level baseball pitchers, with up to 25% of Major League Baseball (MLB) pitchers requiring this procedure at some point during their careers.7,20 In recent years, there have been increasing rates of UCLR at both the professional and the amateur levels, including increased rates among high school–age athletes.16 Numerous studies have demonstrated return-to-play rates between 79% and 87% after UCLR,4,5,8,13,15,17,19–21,28 although a previous study questioned whether this high of a return to competition is sustained for >1 year.21 Pitchers’ performance after UCLR has in general been comparable with that of their noninjured peers and their preinjury baseline levels with regard to innings pitched, earned run average, WHIP (walks plus hits per inning pitched), and pitch velocity.8,13,15,21
Pitch-tracking technology is presently available in every MLB ballpark and is used by all MLB organizations. It is highly accurate, using high-speed cameras to track ball trajectory from release to home plate within 1.02 cm of the ball’s precise location. Each MLB pitcher’s data are publicly available, and they have revolutionized our ability to analyze pitching-specific metrics. In a previous study, we used pitch-tracking data to report that pitch release location is more medial following UCLR.21
Other studies have evaluated pitching biomechanics10,11 and mechanics of the healthy pitcher to understand the pitching motion in general and to identify the portions most associated with high valgus stress.1,2,9,11,24–26 Peak elbow stress loads up to 120 N·m have been found during the pitching motion.25 Anz et al2 found external rotation at the shoulder and valgus torque at the elbow, specifically during the late-cocking phase of the pitching motion, to be most strongly associated with elbow injury among MLB pitchers. Aguinaldo and Chambers1 found that increased elbow extension, sidearm delivery, and early trunk rotation were all associated with increased valgus torque among MLB pitchers. Even more recent studies have suggested the possibility of preinjury structural differences related to UCL injury.3,18
There has been considerable effort undertaken to determine the causes of this injury. While no consensus has been reached, several risk factors have been identified through various study methods: overuse27; mean pitch velocity6,27; fastball percentage14; peak fastball velocity6; pitcher demographics such as age, height,27 weight, body mass index6; and previous success, which may be tied to velocity and usage as well as horizontal release location.27 The purpose of this study was to use publicly available pitch-tracking technology (PITCHf/x; SportsVision) to compare the preinjury release point of MLB pitchers who required UCL reconstructive surgery with that of pitchers who have never undergone UCLR.
Methods
All data in this study were accessed through publicly available resources; thus, no institutional review board approval was necessary.
Patient Population and Demographics
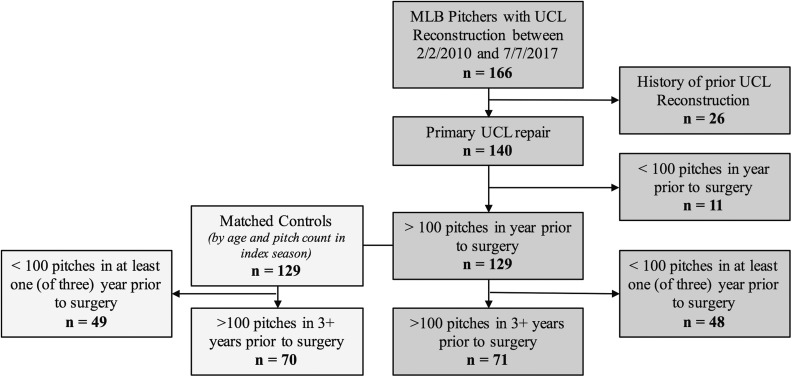
Through a publically available database, we identified 166 MLB pitchers who underwent UCLR between 2010 and 2017.23 Of these pitchers, 26 were excluded for having undergone a previous UCLR and 11 were excluded for having thrown <100 pitches in the calendar year immediately preceding the surgery date (Figure 1). Player demographics, including date of birth, height, weight, throwing arm, and draft slot, were obtained with 2 publicly available online resources (fangraphs.com and baseball-reference.com).
Figure 1.
Study flow outlining exclusion criteria and number of pitchers excluded. A significant percentage of pitchers who underwent UCL reconstruction (37%) and control pitchers (38%) were excluded because they did not have complete data for all 3 years prior to surgery. MLB, Major League Baseball; UCL, ulnar collateral ligament.
Pitch-Tracking Data
Beginning in the 2007 season, the MLB has compiled pitch-tracking data for every pitch thrown in all MLB ballparks with high-speed cameras to follow the baseball along its trajectory from release to home plate to within 1.02 cm of the ball’s precise location.27 The MLB switched technologies from SportsVision’s PITCHf/x to Statcast’s Trackman in the 2017 season, although the overall systems work similarly, with algorithms based on ball speed, spin, and movement to classify each pitch that a pitcher throws into known categories for pitch types. The data are compiled by www.brooksbaseball.net, among other online resources, for analysis. The time ranges for the UCL cohort data collection period were not individual seasons; rather, they were based on the calendar year of the recorded date of surgery. Preinjury year 3 was defined as 1 to 365 days prior to surgery (ie, the year immediately prior to surgery); preinjury year 2 was 366 to 730 days prior to surgery; and preinjury year 1 was 731 to 1095 days prior to surgery.
We evaluated the pitch frequencies for the following pitch types: 4-seam fastballs, sinkers (ie, 2-seam fastballs), changeups, curveballs, and sliders. The pitch release location was collected as a pair of horizontal and vertical coordinates measured in feet (and converted to meters) from the center and top of the mound. The horizontal release location collected for left-handed pitchers was normalized to that of a right-handed pitcher. The total distance from the center of the mound was calculated for each pitcher via the horizontal and vertical release locations. Because release location and velocity are recorded by individual pitch types, each pitcher’s mean release location and mean pitch velocity were then calculated with a weighted mean of all the pitches thrown during the collected period. Only pitchers with >100 pitches in each study year were considered for individual analysis.
Control Group
An age- and pitch count–matched control group was selected for comparison with the UCL cohort. Other variables, such as height, weight, and fastball velocity, were specifically not selected as matching characteristics because they were previously shown to be risk factors for UCLR.6,27 To better understand the potential impact of these other variables, they were included in our regression analysis. First, the season during which a pitcher in the UCL cohort underwent surgery was selected (with the exclusion of the 2017 season, as it was not completed at the time of data collection). Matched controls were selected first by age and then by the most comparable number of pitches in that given season. Individuals with a history of UCLR were excluded from the control group. Demographic and PITCHf/x data for these pitchers were collected in the same way as for the UCL group.
Fastball Percentage, Fastball Velocity, and Pitch Frequencies
Fastball percentages and fastball velocities were collected from fangraphs.com in the same periods used for data collection as PITCHf/x for other variables. The pitch frequency of each pitch type was calculated as the total percentage of pitches thrown among pitchers who threw that individual pitch type.
Position-Specific Statistics
Pitchers who started in ≥50% of their total games played during all 3 seasons were identified as starting pitchers. Pitchers who started in <50% of their total games played for all 3 seasons were identified as relief pitchers. If a pitcher had ≥50% of starts in 1 season and <50% in another, he was not included in either group. Pitches per game were calculated as the quotient of total pitches in a given season divided by the total games played.
Statistical Analysis
All data analysis was performed in Excel for Mac (v 15.14; Microsoft) and SPSS (v 21; IBM). One-way analysis of variance with correlated samples was used to compare data from different years within a given cohort. Paired t tests (2-tailed) were then used if analysis of variance revealed significant differences. Nonpaired t tests and chi-square goodness-of-fit tests were used to compare means and proportions, respectively, between cohorts. P < .05 was considered significant with the added criterion of Bonferroni correction in the case of t tests done after a positive analysis of variance test. Binary logistic regression in SPSS to identify independent risk factors for UCLR was based on the following variables: age, height, weight, fastball velocity, fastball percentages, mean horizontal and vertical release location, and the 3-year changes in the fastball velocity, percentage, and mean horizontal and vertical release locations. All pitch type–specific variables from PITCHf/x were disregarded for this analysis because the regression model required complete data and not all pitchers threw each pitch type.
Results
Participant Demographics
After excluding those who threw <100 pitches in 1 or more of the 3 years before UCLR, the study cohort consisted of 71 pitchers, who were matched with 70 pitchers in the control cohort. The mean age of included pitchers at the date of UCLR was 29.7 years, as compared with 29.2 years for the index year in the control group. The mean number of pitches thrown in the index year was 1267 for all pitchers of the UCL cohort and 1489 for the control group. There were no significant differences between groups in age (P = .402), height (P = .188), weight (P = .152), or body mass index (P = .478). There was no difference in handedness (P = .635) or draft position (P = .420) between the groups (Table 1).
TABLE 1.
UCL and Control Cohort Demographicsa
| Variable | UCL (n = 71) | Control (n = 70) | P |
|---|---|---|---|
| Age, y | 29.65 ± 3.92 [23.44-48.04] | 29.17 ± 3.54 [23.89-42.63] | .402 |
| Pitches, index season | 1267 ± 880 [103-3341] | 1489 ± 941 [135-3576] | .163 |
| Height, cm | 190.5 ± 4.8 [178-201] | 189.0 ± 5.4 [178-201] | .188 |
| Weight, kg | 100.2 ± 7.8 [84-123] | 97.5 ± 9.5 [79-125] | .152 |
| Body mass index | 27.59 ± 2.08 [23.73-33.75] | 27.31 ± 2.38 [21.96-36.96] | .478 |
| Left:right-handed | 19:53 (26.4) | 21:49 (30.0) | .635b |
| Position | .420b | ||
| Starter | 30 (42.3) | 29 (41.4) | |
| Relief | 34 (47.9) | 28 (40.0) | |
| Combination | 7 (9.9) | 12 (17.1) | |
| Draft positionc | 204 ± 235 [1-922] | 262 ± 297 [5-1290] | .154 |
aValues are presented as mean ± SD [range] or n (%).. UCL, ulnar collateral ligament.
bChi-square goodness-of-fit test for proportion of left- and right-handers.
cFifty-three of 71 pitchers in the UCL group and 53 of 70 pitchers in the control group were drafted in the Rule 4 Amateur Draft.
Pitch Selection and Velocity
The percentage of pitchers in the UCL and control cohorts who threw 4-seam fastballs, sinkers, sliders, curveballs, and changeups and their 3-year frequency means are reported in Table 2. There was no significant difference between cohorts for the percentages of pitchers who threw each pitch type (P = .374), nor were there any significant differences in pitch selection between the cohorts for the 4-seam fastball, sinker, slider, and changeup (P > .05). The UCL cohort had a higher frequency of curveballs thrown among those who threw them (P = .020). The control pitchers displayed a significant decrease in mean pitch velocity (P = .005) and mean fastball velocity (P = .012), whereas the UCL group did not show a similar decline (P = .064 and .153, respectively) (Table 3).
TABLE 2.
Pitch Selectiona
| UCL Cohort | Control Cohort | ||||||
|---|---|---|---|---|---|---|---|
| Pitch Type | n | Pitchers, % | Frequency, % | n | Pitchers, % | Frequency, % | P b |
| 4-seam | 65 | 91.5 | 45.4 ± 17.5 | 64 | 91.4 | 40.9 ± 18.7 | .169 |
| Sinker | 41 | 57.7 | 31.3 ± 18.9 | 43 | 61.4 | 31.8 ± 17.9 | .911 |
| Slider | 42 | 59.2 | 24.5 ± 9.9 | 40 | 57.1 | 21.6 ± 7.9 | .158 |
| Curve | 42 | 59.2 | 17.2 ± 9.5 | 44 | 62.9 | 13.0 ± 6.9 | .020 |
| Change | 32 | 45.1 | 12.2 ± 7.6 | 41 | 58.6 | 14.9 ± 7.4 | .142 |
aFrequency values are presented as mean ± SD. Bold indicates statistically significant between-group difference. UCL, ulnar collateral ligament.
bBetween-cohort 2-tailed nonpaired t tests.
TABLE 3.
Pitch Velocitya
| Preinjury Year | P b | |||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| Mean pitch velocity, mph | ||||
| UCL cohort | 89.04 ± 3.23 | 88.99 ± 3.12 | 88.74 ± 3.22 | .064 |
| Control cohort | 89.00 ± 2.64 | 88.84 ± 2.50 | 88.56 ± 2.57 | .005 |
| P valuec | .928 | .760 | .711 | |
| Fastball velocity, mphd | ||||
| UCL cohort | 92.13 ± 2.79 | 92.04 ± 2.80 | 91.89 ± 2.94 | .153 |
| Control cohort | 91.87 ± 2.33 | 91.71 ± 2.40 | 91.49 ± 2.45 | .012 |
| P valuec | .559 | .457 | .392 | |
aBold indicates statistically significant within-group difference. UCL, ulnar collateral ligament.
bWithin-cohort P values were calculated with 1-way analysis of variance with correlated samples.
cNonpaired 2-tailed t tests were calculated between cohorts, with P = .0167 used for significance.
dFastball velocity accessed via fangraphs.com.
Pitch Release Location
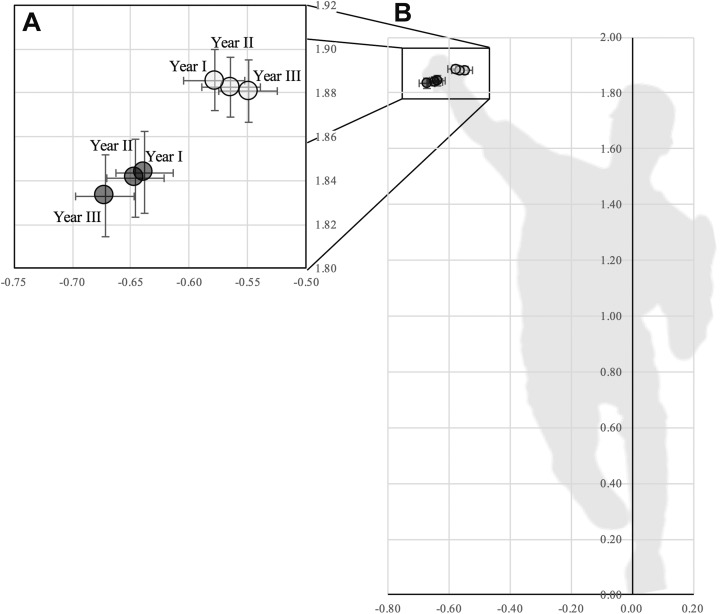
The mean pitch release location in the UCL cohort was more lateral than in the control cohort in preinjury year 2 by 8.1 cm (P = .023) and in preinjury year 3 by 12.2 cm (P = .001), as shown in Figure 2 and Table 4. The vertical release location in preinjury year 3 was 4.8 cm lower in the UCL cohort than in the control cohort (P = .045). The mean release location in the UCL cohort was 3.4 cm more lateral in preinjury year 3 than in preinjury year 1 (P = .036), and there were no significant time-based changes in the control cohort. There was no difference between cohorts in the total release point distance from the center of the mound in all 3 years (P > .05 for all).
Figure 2.
Pitch release location (measured in meters from the center of the mound) as viewed from home plate, with error bars indicating SEM. Negative numbers on the horizontal axis indicate a more lateral release. The ulnar collateral ligament reconstruction cohort is shown in dark gray, with the most lateral data point indicating preinjury year 3. The control cohort is shown in light gray, with the most medial data point indicating preindex year 3. (A) A closer view of (B) the main graph is labeled with corresponding data year.
TABLE 4.
Pitch Release Locationa
| Preinjury Year | P b | |||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| Horizontal release locationc | ||||
| UCL cohort | –0.64 ± 0.21 | –0.65 ± 0.21 | –0.67 ± 0.21 | .068 |
| Control cohort | –0.58 ± 0.22 | –0.57 ± 0.21 | –0.55 ± 0.21 | .129 |
| P valued | .101 | .023 | .001 | |
| Vertical release locationc | ||||
| UCL cohort | 1.84 ± 0.16 | 1.84 ± 0.15 | 1.83 ± 0.16 | .224 |
| Control cohort | 1.89 ± 0.12 | 1.88 ± 0.11 | 1.88 ± 0.12 | .620 |
| P valued | .077 | .072 | .045 | |
| Total distance from center of moundc | ||||
| UCL cohort | 1.95 ± 0.26 | 1.95 ± 0.26 | 1.95 ± 0.26 | .887 |
| Control cohort | 1.97 ± 0.25 | 1.97 ± 0.24 | 1.96 ± 0.25 | .035 |
| P Valued | .326 | .513 | .762 | |
aBold indicates statistically significant within- or between-group difference. UCL, ulnar collateral ligament.
bWithin-cohort P values were calculated with 1-way analysis of variance with correlated samples.
cAll distances were measured from the center of the mound in meters on x- and y-axes.
dNonpaired 2-tailed t tests were calculated between cohorts, with P = .0167 used for significance.
Pitcher Usage by Position
Overall, 30 of the 71 pitchers in the UCL group and 28 of the 70 controls were identified as starting pitchers by the criteria outlined earlier, and 34 and 29 were identified as relief pitchers, respectively, with the remainder not included in either group. The starting pitchers in the UCL and control cohorts started a similar number of games per year on average—22.9 and 23.0, respectively—and had similar a number of pitchers per game, at 93.7 and 92.6 (Table 5). The relief pitchers of the UCL cohort threw fewer pitches per outing (P = .046) on average in the 3-year period but did not have a significant difference in the game appearances per season: 51.7 in the UCL cohort versus 46.3 in the control cohort. In the season immediately prior to surgery, the relief pitchers in the UCL group appeared in only 39.7 games on average, as compared with their 3-year mean of 51.7 games.
TABLE 5.
Pitcher Usage by Positiona
| Preinjury Year 3 Only | 3-y Mean | |||||
|---|---|---|---|---|---|---|
| Pitchers | UCL (n = 30) | Control (n = 28) | P | UCL (n = 30) | Control (n = 28) | P |
| Starting | ||||||
| Games started | 21.8 ± 6.7 | 22.0 ± 9.2 | .913 | 22.9 ± 7.1 | 23.0 ± 7.3 | .944 |
| Pitches/game | 93.2 ± 10.7 | 92.3 ± 10.7 | .690 | 93.7 ± 8.0 | 92.6 ± 8.5 | .640 |
| UCL (n = 34) | Control (n = 29) | UCL (n = 34) | Control (n = 29) | |||
| Relief | ||||||
| Games played | 39.7 ± 18.8 | 46.7 ± 20.2 | .167 | 51.7 ± 16.1 | 46.3 ± 15.6 | .193 |
| Pitches/game | 17.1 ± 6.4 | 20.8 ± 11.9 | .130 | 16.9 ± 4.7 | 20.4 ± 8.4 | .046 |
aValues are presented as mean ± SD. Bold indicates statistically significant between-group difference. UCL, ulnar collateral ligament.
Regression Model and Prediction Rule
Of the 11 variables used for the binary logistic regression model, only a more lateral horizontal release location was identified as a significant risk factor (P = .048), with an odds ratio of 0.51 (95% CI, 0.26-0.99) (Table 6). The unit used in the regression model for release location was meters; thus, this 0.51 odds ratio equates to an added odds risk of UCLR of 4.9% for every 10-cm increase in lateral release location. The model created a prediction rule based on those 11 variables with a statistical accuracy of 66.7% (Table 7).
TABLE 6.
Binary Logistic Regressiona
| Beta (SE) | Odds Ratio (95% CI) | P | |
|---|---|---|---|
| Age | 0.028 (0.056) | 1.028 (0.343-3.082) | .610 |
| Height | 0.103 (0.107) | 1.108 (0.899-1.367) | .337 |
| Weight | 0.009 (0.011) | 1.009 (0.988-1.031) | .424 |
| Fastball velocity | 0.122 (0.085) | 1.130 (0.956-1.335) | .151 |
| Change in fastball velocity | –0.015 (0.169) | 0.985 (0.707-1.372) | .931 |
| Fastball percentage | –2.715 (2.139) | 0.066 (0.001-4.382) | .204 |
| Change in fastball percentage | 1.788 (2.399) | 5.977 (0.054-658.5) | .456 |
| Horizontal release location | –0.671 (0.339) | 0.511 (0.263-0.993) | .048 |
| Change in horizontal release location | –0.725 (0.495) | 0.484 (0.184-1.278) | .143 |
| Vertical release location | –0.606 (0.497) | 0.546 (0.206-1.445) | .223 |
| Change in vertical release location | 1.003 (1.225) | 2.726 (0.247-30.08) | .424 |
aBold indicates statistical significance. UCL, ulnar collateral ligament.
TABLE 7.
Prediction Rulea
| Predicted, n | |||
|---|---|---|---|
| Actual | Control | UCL | Correct, % |
| Control | 46 | 24 | 65.7 |
| UCL | 23 | 48 | 67.6 |
| Overall | 66.7 | ||
aUCL, ulnar collateral ligament.
Discussion
The purpose of this study was to identify, using preoperative pitch-tracking data, potential risk factors for eventual UCLR among MLB pitchers. Our analysis revealed that a more lateral release point was associated with an increased risk for UCLR. In this study, pitchers who eventually required UCLR started with similar horizontal release locations as control pitchers. As they approached UCL rupture, the mean release location moved to a more lateral release location. Both findings suggest that pitch tracking may allow for surveillance of current injury-free pitchers. If pitchers exhibit pitching mechanic changes, including a more lateral release point, they may be at risk for requiring UCLR. Given that all active MLB pitchers have up-to-date pitch-tracking data, ball clubs can monitor release points, among other statistics, in real time for all active pitchers and can modify pitching mechanics to aid in injury prevention.
This study is the first of its kind to quantify preinjury release location changes among pitchers who undergo UCLR. In the year immediately prior to surgery, the mean release location of pitchers in the UCL group was 12.2 cm more lateral and 4.8 cm lower than that of the control pitchers. In comparison with 2 years earlier in their MLB careers, pitchers in the UCL group threw 3.4 cm more laterally in the year immediately prior to surgery. Both aforementioned differences were statistically significant, and we believe them to be clinically significant as well, given that they may provide MLB organizations with insight to UCLR risk among their athletes over time.
In a previous study analyzing UCLR outcomes via PITCHf/x, we found that the mean release location of pitchers in the UCL group moved medially after surgery, which we theorized to be a protective mechanism to reduce valgus stress after UCLR.21 Our data suggest that there may be a critical point at which a wide arm slot increases the valgus stress at the elbow enough to cause UCL failure. Others have reported that sidearm pitchers and the associated increased elbow extension put these players at greater risk for UCL injury.1,26 This finding further substantiates the idea that a more medial release after surgery may be protective. Werner et al26 found that elbow extension was a key contributor to valgus torque during the pitching motion, which ultimately makes it a contributor to UCL failure. Our study measured only the release location, which is a complex function of a number of factors, including trunk tilt, shoulder abduction, and elbow flexion. We posit that elbow flexion may be one of the important variables in this function that links increased valgus stress in the elbow with the increased risk associated with a lateral release location.
Whiteside et al27 conducted the only study that revealed a more lateral release location to be protective in the context of UCLR. Their study, which used data and methods similar to ours, found that pitchers who underwent UCLR had, on average, a more lateral release location: 34% of the pitcher’s height versus 32% of the pitcher’s height—or, for a pitcher whose height is 2 m, about 4-cm difference, which is similar to our finding of 6 to 12 cm in the same direction. As in our study, the authors normalized horizontal release location to that of a right-handed pitcher, which should yield negative raw data values but report horizontal release location as positive values. In their regression model, they found a significant negative beta coefficient associated with horizontal release location, which was interpreted as a negative relationship between release location and risk of UCLR. This led to their conclusion that a more lateral release location was protective. Thus, it is possible that the data from Whiteside et al27 were misinterpreted because of this lack of consistency with negative integers. That would explain why our study’s regression model reflected a similarly negative beta coefficient for release location but with an opposite interpretation to Whiteside et al.27 It is also possible that their statistical model was interpreted correctly despite the mean release locations being similar to those in our study, but we believe that this is statistically less likely.
Although previous studies13,14 identified increased mean pitch and fastball velocity in pitchers who required UCLR, we did not find a statistically significant difference between groups in our study. Chalmers et al6 used similar methods to identify that peak velocity and mean velocity are associated with increased risk of UCLR. One key difference in our previous21 and current studies is that we used age-matched controls, whereas they used a population-based sample. Their pre-UCL cohort was significantly younger than the control cohort, suggesting that age and MLB experience may be confounding variables contributing to the velocity differences. In this study, we found that pitch velocity decreased over time for our control pitchers and that this change was less pronounced in the UCL cohort; however, these changes were all <1 mph, so the clinical significance is unclear.
In addition to pitch velocity, we examined pitch selection differences between cohorts, and unlike Keller et al,14 we did not find a significant difference in fastball percentages between cohorts. We did, however, see that the control pitchers had a significant decline in their fastball and total pitching velocity over the 3 years, adding to the evidence that MLB experience contributes to changes in pitching tendencies. Additionally, our study identified that pitchers in the UCL group threw more curveballs compared with the control group, although all other frequencies were similar. While some previous literature has shown that curveballs cause increased risk of arm pain, particularly for the adolescent pitcher,29 a recent study found no correlation between pitch type and UCLR risk,22 and a recent review found limited biomechanical or epidemiologic data showing that curveballs are more damaging than fastballs.12
This study also identified that relief pitchers who undergo UCLR might be used differently than relief pitchers in the control cohort. Three complicating factors made this analysis difficult, however. First, there is no literature consensus on the definition of a relief pitcher. Second, the control cohort was not explicitly matched to assess position-specific differences. Third, over the years studied, many pitchers’ positions changed. That being said, the relief pitchers who underwent UCLR in our study threw significantly fewer pitches per game and subsequently had more games played per year compared with relief pitchers in the control cohort. Overall, these data support the findings of Whiteside et al27 in that fewer days’ rest between appearances was associated with higher injury risk. Hence, increased game appearances for relief pitchers might predispose them to UCL injury.
There are several important limitations to this study. First, the data were gathered from internet sources and are thus only as accurate as these sources. Although a limitation, data obtained in this manner are increasingly prevalent in peer-reviewed studies.6,13,14,21,27 Second, pitch tracking estimates only the ball’s release location and does not determine the exact joint angles at the shoulder and elbow, nor does it account for body position on the mound or the posture and delivery mechanics of the arm, shoulder, or trunk. Third, our analysis did not control for potentially confounding variables, such as height, body positioning on the mound, and varying delivery mechanics, but rather attempted to elucidate their true effects by including them in the logistic regression model. In the future, formal biomechanical analysis is needed to better elucidate if release location is a surrogate of arm slot. Finally, the selection of our control group is susceptible to lead-time bias, although any error caused by this would reduce any true differences that we found. Despite these limitations, our findings suggest that differences in pitch release locations do exist between those who require UCLR and those who do not. Further evaluation of pitchers’ release point and joint angles is necessary to clearly define the impact that they have on the risk of UCL injury and the need for subsequent reconstruction.
Conclusion
Lateral release location and progressive lateralization of release point were significant risk factors for the eventual need for UCLR among MLB pitchers. Pitch selection and pitch velocity were similar between pitchers at risk for UCLR and control pitchers. Powerful modern technology, such as PITCHf/x and Trackman, allows for accurate monitoring of potential risk factors, including arm position. We believe horizontal pitch release location to be a surrogate measure of elbow extension and one that can be feasibly assessed given the current MLB pitch-tracking infrastructure. This information could potentially be used to better identify pitchers at risk for UCL injury.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: M.D.S. is a consultant for Becton Dickinson and Company, Medacta, Tornier, and Wright Medical; has received honoraria from Encore Medical; has received educational support from Medwest and Tornier; and receives royalties from Tornier and Wright Medical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was not sought for the present study.
References
- 1. Aguinaldo AL, Chambers H. Correlation of throwing mechanics with elbow valgus load in adult baseball pitchers. Am J Sports Med. 2009;37(10):2043–2048. [DOI] [PubMed] [Google Scholar]
- 2. Anz AW, Bushnell BD, Griffin LP, Noonan TJ, Torry MR, Hawkins RJ. Correlation of torque and elbow injury in professional baseball pitchers. Am J Sports Med. 2010;38(7):1368–1374. [DOI] [PubMed] [Google Scholar]
- 3. Atanda A, Jr, Buckley PS, Hammoud S, Cohen SB, Nazarian LN, Ciccotti MG. Early anatomic changes of the ulnar collateral ligament identified by stress ultrasound of the elbow in young professional baseball pitchers. Am J Sports Med. 2015;43(12):2943–2949. [DOI] [PubMed] [Google Scholar]
- 4. Azar FM, Andrews JR, Wilk KE, Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med. 2000;28(1):16–23. [DOI] [PubMed] [Google Scholar]
- 5. Cain EL, Jr, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38(12):2426–2434. [DOI] [PubMed] [Google Scholar]
- 6. Chalmers PN, Erickson BJ, Ball B, Romeo AA, Verma NN. Fastball pitch velocity helps predict ulnar collateral ligament reconstruction in Major League Baseball pitchers. Am J Sports Med. 2016;44(8):2130–2135. [DOI] [PubMed] [Google Scholar]
- 7. Conte SA, Fleisig GS, Dines JS, et al. Prevalence of ulnar collateral ligament surgery in professional baseball players. Am J Sports Med. 2015;43(7):1764–1769. [DOI] [PubMed] [Google Scholar]
- 8. Erickson BJ, Gupta AK, Harris JD, et al. Rate of return to pitching and performance after Tommy John surgery in Major League Baseball pitchers. Am J Sports Med. 2014;42(3):536–543. [DOI] [PubMed] [Google Scholar]
- 9. Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23(2):233–239. [DOI] [PubMed] [Google Scholar]
- 10. Fleisig GS, Leddon CE, Laughlin WA, et al. Biomechanical performance of baseball pitchers with a history of ulnar collateral ligament reconstruction. Am J Sports Med. 2015;43(5):1045–1050. [DOI] [PubMed] [Google Scholar]
- 11. Glousman RE, Barron J, Jobe FW, Perry J, Pink M. An electromyographic analysis of the elbow in normal and injured pitchers with medial collateral ligament insufficiency. Am J Sports Med. 1992;20(3):311–317. [DOI] [PubMed] [Google Scholar]
- 12. Grantham WJ, Iyengar JJ, Byram IR, Ahmad CS. The curveball as a risk factor for injury: a systematic review. Sports Health. 2015;7(1):19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jiang JJ, Leland JM. Analysis of pitching velocity in Major League Baseball players before and after ulnar collateral ligament reconstruction. Am J Sports Med. 2014;42(4):880–885. [DOI] [PubMed] [Google Scholar]
- 14. Keller RA, Marshall NE, Guest JM, Okoroha KR, Jung EK, Moutzouros V. Major League Baseball pitch velocity and pitch type associated with risk of ulnar collateral ligament injury. J Shoulder Elbow Surg. 2016;25(4):671–675. [DOI] [PubMed] [Google Scholar]
- 15. Keller RA, Steffes MJ, Zhuo D, Bey MJ, Moutzouros V. The effects of medial ulnar collateral ligament reconstruction on major league pitching performance. J Shoulder Elbow Surg. 2014;23(11):1591–1598. [DOI] [PubMed] [Google Scholar]
- 16. Mahure SA, Mollon B, Shamah SD, Kwon YW, Rokito AS. Disproportionate trends in ulnar collateral ligament reconstruction: projections through 2025 and a literature review. J Shoulder Elbow Surg. 2016;25(6):1005–1012. [DOI] [PubMed] [Google Scholar]
- 17. Makhni EC, Lee RW, Morrow ZS, Gualtieri AP, Gorroochurn P, Ahmad CS. Performance, return to competition, and reinjury after Tommy John surgery in Major League Baseball pitchers: a review of 147 cases. Am J Sports Med. 2014;42(6):1323–1332. [DOI] [PubMed] [Google Scholar]
- 18. Meyer CJ, Garrison JC, Conway JE. Baseball players with an ulnar collateral ligament tear display increased nondominant arm humeral torsion compared with healthy baseball players. Am J Sports Med. 2017;45(1):144–149. [DOI] [PubMed] [Google Scholar]
- 19. O’Brien DF, O’Hagan T, Stewart R, et al. Outcomes for ulnar collateral ligament reconstruction: a retrospective review using the KJOC assessment score with two-year follow-up in an overhead throwing population. J Shoulder Elbow Surg. 2015;24(6):934–940. [DOI] [PubMed] [Google Scholar]
- 20. Osbahr DC, Cain EL, Jr, Raines BT, Fortenbaugh D, Dugas JR, Andrews JR. Long-term outcomes after ulnar collateral ligament reconstruction in competitive baseball players: minimum 10-year follow-up. Am J Sports Med. 2014;42(6):1333–1342. [DOI] [PubMed] [Google Scholar]
- 21. Portney DA, Lazaroff JM, Buchler LT, Gryzlo SM, Saltzman MD. Changes in pitching mechanics after ulner collateral ligament reconstruction in Major League Baseball pitchers. J Shoulder Elbow Surg. 2017;26(8):1307–1315. [DOI] [PubMed] [Google Scholar]
- 22. Prodromo J, Patel N, Kumar N, Denehy K, Tabb LP, Tom J. Pitch characteristics before ulnar collateral ligament reconstruction in major league pitchers compared with age-matched controls. Orthop J Sports Med. 2016;4(6):2325967116653946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Roegele J. Tommy John surgery list. https://docs.google.com/spreadsheets/d/1gQujXQQGOVNaiuwSN680Hq-FDVsCwvN-3AazykOBON0/edit#gid=0. Accessed May 2016.
- 24. Seroyer ST, Nho SJ, Bach BR, Bush-Joseph CA, Nicholson GP, Romeo AA. The kinetic chain in overhand pitching: its potential role for performance enhancement and injury prevention. Sports Health. 2010;2(2):135–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Werner SL, Fleisig GS, Dillman CJ, Andrews JR. Biomechanics of the elbow during baseball pitching. J Orthop Sports Phys Ther. 1993;17(6):274–278. [DOI] [PubMed] [Google Scholar]
- 26. Werner SL, Murray TA, Hawkins RJ, Gill TJ. Relationship between throwing mechanics and elbow valgus in professional baseball pitchers. J Shoulder Elbow Surg. 2002;11(2):151–155. [DOI] [PubMed] [Google Scholar]
- 27. Whiteside D, Martini DN, Lepley AS, Zernicke RF, Goulet GC. Predictors of ulnar collateral ligament reconstruction in Major League Baseball pitchers. Am J Sports Med. 2016;44(9):2202–2209. [DOI] [PubMed] [Google Scholar]
- 28. Wymore L, Chin P, Geary C, et al. Performance and injury characteristics of pitchers entering the Major League Baseball draft after ulnar collateral ligament reconstruction. Am J Sports Med. 2016;44(12):3165–3170. [DOI] [PubMed] [Google Scholar]
- 29. Yang J, Mann BJ, Guettler JH, et al. Risk-prone pitching activities and injuries in youth baseball: findings from a national sample. Am J Sports Med. 2014;42(6):1456–1463. [DOI] [PubMed] [Google Scholar]