ABSTRACT
Objective
To compare the epidemiology of renal replacement therapy (RRT) for end-stage renal disease (ESRD) in Latin America and Europe, as well as to study differences in macroeconomic indicators, demographic and clinical patient characteristics, mortality rates, and causes of death between these two populations.
Methods
We used data from 20 Latin American and 49 European national and subnational renal registries that had provided data to the Latin American Dialysis and Renal Transplant Registry (RLADTR) and the European Renal Association-European Dialysis and Transplant Association (ERA-EDTA) Registry, respectively. The incidence and prevalence of RRT in 2013 were calculated per million population (pmp), overall and by subcategories of age, sex, primary renal disease, and treatment modality. The correlation between gross domestic product and the prevalence of RRT was analyzed using linear regression. Trends in the prevalence of RRT between 2004 and 2013 were assessed using Joinpoint regression analysis.
Results
In 2013, the overall incidence at day 91 after the onset of RRT was 181 pmp for Latin American countries and 130 pmp for European countries. The overall prevalence was 660 pmp for Latin America and 782 pmp for Europe. In the Latin American countries, the annual increase in the prevalence averaged 4.0% (95% confidence interval (CI): 2.5%-5.6%) from 2004 to 2013, while the European countries showed an average annual increase of 2.2% (95% CI: 2.0%-2.4%) for the same time period. The crude mortality rate was higher in Latin America than in Europe (112 versus 100 deaths per 1 000 patient-years), and cardiovascular disease was the main cause of death in both of those regions.
Conclusions
There are considerable differences between Latin America and Europe in the epidemiology of RRT for ESRD. Further research is needed to explore the reasons for these differences.
Keywords: Kidney failure, chronic, dialysis, kidney transplantation, mortality, renal replacement therapy, Latin America, Europe
RESUMEN
Objetivo
Comparar los datos epidemiológicos del tratamiento sustitutivo de la función renal (TSFR) para la nefropatía terminal en América Latina y Europa, así como estudiar las diferencias en cuanto a indicadores macroeconómicos, características demográficas y clínicas de los pacientes, tasas de mortalidad y causas de defunción entre estas dos poblaciones.
Métodos
Utilizamos los datos de 20 registros renales latinoamericanos y 49 europeos, a nivel nacional y subnacional, que le habían proporcionado datos al Registro Latinoamericano de Diálisis y Trasplante Renal (RLADTR) y al Registro de la Asociación Europea Renal–Asociación Europea de Diálisis y Trasplantes (ERA-EDTA, por su sigla en inglés), respectivamente. Se calculó la incidencia y la prevalencia del TSFR en el 2013 por millón de habitantes, en total y por subcategoría (edad, sexo, nefropatía primaria y modalidad de tratamiento). Se analizó la correlación entre el producto interno bruto y la prevalencia de TSFR mediante regresión lineal. Se evaluaron las tendencias en la prevalencia de TSFR entre el 2004 y el 2013 mediante un análisis de regresiones lineales segmentadas.
Resultados
En el 2013, la incidencia general al día 91 después de iniciar el tratamiento sustitutivo de la función renal era de 181 por millón de habitantes en los países latinoamericanos y de 130 en los países europeos. La prevalencia general era de 660 por millón de habitantes para América Latina y de 782 para Europa. En los países latinoamericanos, el aumento anual promedio de la prevalencia fue de 4,0% (intervalo de confianza de 95% [IC]: 2,5%-5,6%) entre el 2004 y el 2013, mientras que los países europeos registraron un aumento anual promedio de 2,2% (IC de 95%: 2,0%-2,4%) durante el mismo período. La tasa bruta de mortalidad fue mayor en América Latina que en Europa (112 defunciones por 1 000 años-paciente, en comparación con 100 defunciones), y las enfermedades cardiovasculares fueron la principal causa de muerte en ambas regiones.
Conclusiones
Hay considerables diferencias entre América Latina y Europa en cuanto a los datos epidemiológicos del tratamiento sustitutivo de la función renal para la nefropatía terminal. Es necesario hacer más investigaciones para explorar las razones de tales diferencias.
Palabras clave: Fallo renal crónico, diálisis, trasplante de riñón, mortalidad, terapia de reemplazo renal, América Latina, Europa (continente)
RESUMO
Objetivo
Comparar o perfil epidemiológico de pacientes com doença renal em estágio final (DREF) em terapia renal substitutiva (TRS) na América Latina e na Europa e examinar as diferenças nos indicadores macroeconômicos, características demográficas e clínicas, taxas de mortalidade e causas de morte entre as duas populações de pacientes.
Métodos
O estudo foi baseado em informação de 20 registros latino-americanos e 49 registros nacionais e subnacionais europeus que haviam fornecido dados ao Registro Latino-Americano de Diálise e Transplante Renal (RLADTR) e Registro da Associação Europeia de Nefrologia e Associação Europeia de Diálise e Transplante (ERA-EDTA), respectivamente. A incidência e a prevalência de TRS em 2013 foram calculadas por milhão de habitantes (pmh), geral e por subcategorias de idade, sexo, doença renal primária e modalidade de tratamento. A correlação entre o produto interno bruto (PIB) e a prevalência de TRS foi analisada com o uso de regressão linear. Tendências na prevalência de TRS entre 2004 e 2013 foram analisadas com o uso de regressão linear segmentada.
Resultados
Em 2013, a incidência geral ao dia 91 do início de TRS foi 181 pmh nos países latino-americanos e 130 pmh nos países europeus. Observou-se uma prevalência geral de TRS de 660 pmh na América Latina e 782 pmh na Europa. No período 2004–2013, o aumento médio anual da prevalência foi de 4,0% (intervalo de confiança de 95% [IC 95%] 2,5%–5,6%) nos países latino-americanos, enquanto que houve um aumento médio anual de 2,2% (IC 95% 2,0%–2,4%) nos países europeus. A taxa de mortalidade bruta foi maior na América Latina que na Europa (112 versus 100 óbitos por 1.000 pacientes-anos) e doença cardiovascular foi a principal causa de morte em ambas as regiões.
Conclusões
Existem diferenças consideráveis entre a América Latina e a Europa no perfil epidemiológico dos pacientes com DREF em TRS. Outras pesquisas devem ser realizadas para investigar mais a fundo estas diferenças.
Palavras-chave: Falência renal crônica, diálise, transplante de rim, mortalidade, terapia de substituição renal, América Latina, Europa (continente)
The incidence and prevalence of renal replacement therapy (RRT) for end-stage renal disease (ESRD) in a country are influenced by various factors, including the distribution of the primary causes of kidney failure, the progression of chronic kidney disease (CKD), the mortality rate, resource availability, and national wealth (1-5). In Latin America, the Latin American Dialysis and Renal Transplant Registry (RLADTR) has since 1991 collected data annually on patients receiving RRT, via national and subnational registries. The European Renal Association-European Dialysis and Transplant Association (ERA-EDTA) Registry has collected these data since 1964 in Europe. Latin America and Europe have different social and cultural conditions, health and health care policies, and economic situations (6, 7). Comparing epidemiological data from these two international RRT registries allows us to determine differences and similarities that will help us understand the burden of this disease in these two parts of the world, and that could form a basis for future collaborative international studies. To the best of our knowledge, this is the first study to investigate differences in the epidemiology of RRT between Latin America and Europe.
The aim of this study was therefore to compare the incidence and prevalence of RRT for ESRD in Latin America and Europe. In addition, we looked at differences in macroeconomic indicators, demographic and clinical patient characteristics, RRT modalities, and causes of death between these two populations.
SUBJECTS AND METHODS
General population data
National macroeconomic data, life expectancy, and educational level corresponding to the year 2013 were collected from the World Bank DataBank (8) and from the World Health Organization (WHO) (9). The following indicators were collected for each country: life expectancy at age 65 years (the number of years an individual aged 65 years would be expected to live), gross domestic product (GDP) per capita based on purchasing power parity (PPP) expressed in US dollars, prevalence of diabetes mellitus and hypertension in the general population, public health expenditure as a percentage of GDP expressed in US dollars (percentage of GDP spent on public health care), and net enrollment rate for secondary school (total number of students in the theoretical age group for secondary education enrolled at that level) expressed as a percentage of the total population in that age group.
Latin American Dialysis and Renal Transplant Registry
The RLADTR collected data on incident and prevalent patients undergoing RRT in 2013 through an annual survey, which was completed by 20 national or subnational renal registries in Latin America. While 12 of these renal registries collected individual patient data, the dataset provided to RLADTR consisted of aggregated data for each of the countries. The data used for this article were made available by the RLADTR Registry Committee. Data on kidney transplantation were collected in collaboration with the Latin American and Caribbean Transplant Society (STALYC) (10).
European Renal Association-European Dialysis and Transplant Association Registry
In 2015, the ERA-EDTA Registry received the 2013 data from 49 national and subnational renal registries in 34 countries in Europe or bordering the Mediterranean Sea (e.g., Israel, Tunisia). Datasets comprising individual patient data were received from 31 national or subnational renal registries in 17 countries, whereas 18 national renal registries contributed data in an aggregated form (11). Midyear population data for the contributing countries and country subregions were derived from Eurostat (12), the respective national bureau of statistics, or the respective national or subnational renal registry.
Definitions and calculations
The incidence of RRT was defined as the number of patients starting RRT in one year (2013). and the prevalence of RRT was expressed as the number of patients alive and receiving RRT on 31 December 2013. Incidence and prevalence per million population (pmp) and per million age-related population (pmarp) were calculated by dividing the observed count by the midyear population.
For both international registries, the incidence and prevalence of RRT were calculated overall and by subcategories of age (< 65 and ≥ 65 years), sex, primary renal disease, and treatment modality. The different treatment modalities considered were hemodialysis (defined as in-center hemodialysis, home hemodialysis, hemofiltration, and hemodiafiltration), peritoneal dialysis (defined as continuous ambulatory or automated and intermittent ambulatory or automated) and kidney transplantation (defined as kidney transplanted from a related or unrelated living donor, deceased donor, or an unknown type of donor) (11).
There were subtle differences in the coding systems used for primary renal diseases and causes of death between the two registries. To be able to compare the data from the two registries, we regrouped the primary renal diseases into the following five categories: glomerulonephritis, diabetes mellitus, hypertension/renal vascular disease, other, and unknown (Supplementary Table S1). The causes of death were regrouped into the following seven categories: cardiovascular, cerebrovascular, infection, malignancy, suicide/treatment refusal/treatment withdrawal, miscellaneous, and unknown (Supplementary Table S2). The category of cardiovascular causes included myocardial ischemia and infarction, heart failure, and cardiac arrest. An overview of the availability of data for each country is provided in Supplementary Table S3. Data for the whole of Spain was used when available, but otherwise the analyses included data from the separate regions in Spain. For both of the international registries, data on treatment modality was recorded on day 91 after the onset of RRT.
Statistical analysis
Linear regression models were used to explore the correlation between the GDP and the prevalence of RRT in the countries in Europe and Latin America.
For those countries that had data available on the prevalence of RRT for the period from 2004 to 2013 (Supplementary Table S3), we examined trends over time in the prevalence, using Joinpoint regression analysis. These analyses were based on Poisson regression and were performed using the Joinpoint 4.0.4 software (13). The trends over time are presented as annual percentage change (APC) with 95% confidence interval (CI). Causes of death were analyzed for those countries reporting less than 50% of the causes missing or unknown.
With the exception of the Joinpoint regression analysis, the statistical analyses were performed using SPSS version 21 software (IBM Corporation, Armonk, New York, United States of America).
RESULTS
General population data
The data from 20 countries/subregions in Latin America covered 80% of the Latin American general population, while the 49 countries/subregions in Europe represented 79% of the European general population. The median life expectancy at the age of 65 years was 9 years for the Latin American countries and 14 years for the European countries. The GDP per capita was twice as high in the European countries as in the Latin American countries. The prevalence of diabetes mellitus in the general population was lower in Europe than in Latin America, whereas the prevalence of hypertension was higher in Europe (Table 1).
TABLE 1. Characteristics of the Latin American Dialysis and Transplant Registry (RLADTR) and the European Renal Association-European Dialysis and Transplant Association (ERA-EDTA) registry, as well as of the general population and the macroeconomic situation in the countries of Latin America and Europe covered by those two registries.
| Indicator | Latin America | Europe |
|---|---|---|
| Registry countries/subregions with individual data (no.) | 0 | 17a |
| Registry countries/subregions with aggregated data (no.) | 20 | 18 |
| General population covered by registry (percent) | 80% | 79% |
| Life expectancy at 65 yearsb; median (IQR)c (years) | 9 (9-12) | 14 (10-16) |
| Prevalence of diabetes mellitus in general populationd (percent) | 8.6% | 5.6% |
| Prevalence of hypertension in general populationd (percent) | 21.8% | 24.0% |
| GDPe per capita, PPP,f in US$,b median (IQR) | 12 520 (8 197 to 19 354) | 26 200 (18 977 to 38 166) |
| Health expenditure, public,b percent of GDP | 4.5% | 6% |
| Net enrollment rate for secondary school, both sexesb (percent) | 74% | 92% |
Source: Prepared by the authors, using study data.
For ERA-EDTA, individual patient data were received from 31 national and subnational registries in 17 countries (Supplementary Table S3).
Data from the World Bank, corresponding to 2013.
IQR = interquartile range.
Data from the World Health Organization.
GDP = gross domestic product.
PPP = purchasing power parity.
Incidence
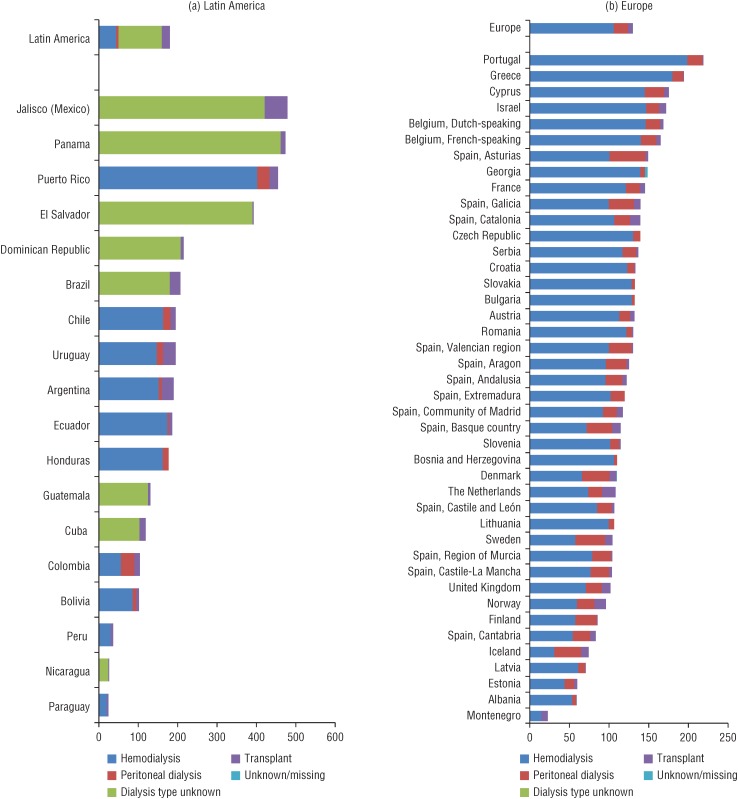
In 2013, a total number of 145 678 patients started RRT for ESRD in the two international registries combined. The overall incidence at day 91 was 181 pmp for Latin America and 130 pmp for Europe. Figure 1 shows that the highest incidence rates were reported by two registries in Latin America, Jalisco (Mexico) and Panama, with 479 pmp and 474 pmp, respectively. Paraguay and Montenegro reported the lowest incidence rates, with less than 25 pmp each. In both Latin America and Europe, the majority of patients were male, 55% (71.7 pmp) and 62% (79.3 pmp), respectively. Of the incident patients in Latin America, 38.3% (695.3 pmarp) were aged over 65 years, and in Europe 56.2% (467.5 pmarp) were aged over 65 years. Nicaragua (112.7 pmarp) and Paraguay (168.4 pmarp) were the countries with the lowest incidence rates among patients older than 65 years, whereas Dutch- and French-speaking Belgium (612 and 628 pmarp, respectively) and Greece (641 pmarp) reported the highest incidence in this age group.
FIGURE 1. Unadjusted incidence rates per million population (pmp) of patients under renal replacement therapy, by treatment modality at day 91 in Latin America (A) and Europe (B).
Source: Prepared by authors, using study data.
Both the unadjusted incidence of patients receiving dialysis and the incidence of kidney transplantation were higher in Latin America than in Europe (Figure 1). The highest transplant rates at day 91 of RRT were found in Jalisco (Mexico) (58 pmp), Uruguay (32 pmp), and Argentina (30 pmp).
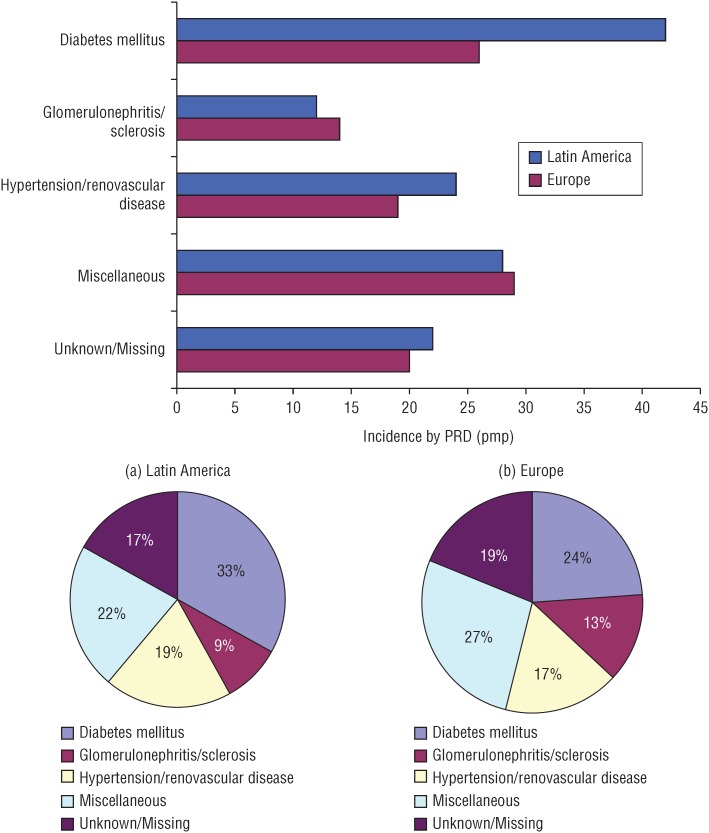
Figure 2 shows the incidence by the primary renal disease (PRD). Diabetes mellitus had the highest incidence rate in both regions, but the incidence rate was almost twice as high in Latin America as in Europe (42 pmp versus 26 pmp). The incidence of other primary renal diseases was similar for Latin America and Europe.
FIGURE 2. Unadjusted incidence rates per million population (pmp) and as a percentage, by primary renal disease (PRD) in Latin America (A) and Europe (B)a.
a For Europe, the figures are based on data from all countries/subregions except for the Czech Republic. For Latin America, the figures are based on data from Argentina, Bolivia, Ecuador, Guatemala, Paraguay, Peru, and Uruguay (Supplementary Table S3).
Source: Prepared by the authors, using study data.
Prevalence
On 31 December 2013, a total of 799 296 patients with ESRD were receiving RRT in all registries reporting to RLADTR and the ERA-EDTA Registry, corresponding to an unadjusted prevalence of 660 pmp for Latin America and of 782 pmp for Europe (Supplementary Table S4). The prevalence was highest in Puerto Rico and Portugal (1 847 and 1 749 pmp, respectively), while the lowest prevalence was found in Paraguay and Ukraine (less than 200 pmp each). Males accounted for 57% of the prevalent RRT patients in Latin America (287 pmp) and 60% in Europe (667 pmp).
In the Latin American countries, hemodialysis was the most common treatment modality (66%, 436 pmp), whereas 10% (67 pmp) were treated with peritoneal dialysis, and 24% (157 pmp) had a functioning kidney transplant. In the European countries, most patients were treated with hemodialysis (58%, 456 pmp) or had a functioning transplant (36%, 281 pmp). The five countries and subregions with the highest prevalence of peritoneal dialysis all belong to Latin America, with Jalisco (Mexico) (487 pmp) in the lead.
The prevalence of diabetes mellitus as a primary cause of ESRD was higher in Latin American countries (147 pmp) than in European countries (114 pmp) (data not shown). Puerto Rico reported the highest prevalence (644 pmp) of diabetes mellitus as a primary renal disease and Ukraine the lowest prevalence (21 pmp).
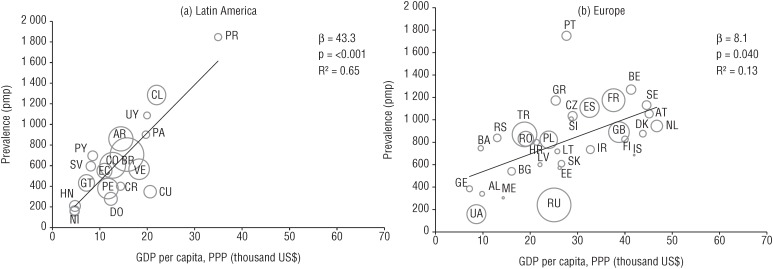
As is shown in Figure 3, we found a positive correlation between GDP per capita (in terms of PPP in US$) and the prevalence of RRT in 2013, with a higher prevalence of RRT in countries with a larger GDP. In Latin America, the RRT prevalence increased by 43 pmp for every US$ 1 000 increase in GDP per capita (95% confidence interval (CI): 28–59). Within Europe, this association was weaker; for each standard deviation increase in GDP per capita, the RRT prevalence increased by 8 pmp (95% CI: 1.0–16).
FIGURE 3. Association between gross domestic product (GDP) per capita and prevalence of renal replacement therapy (RRT) per million population (pmp), in Latin America (A) and Europe (B)a.
a The weighted regression line in this bubble plot displays the univariate association between gross domestic product (GDP) per capita (based on purchasing power parity (PPP) expressed in US dollars) and the RRT prevalence. The size of marker denotes the size of the general population under study. The country abbreviations used are: AL, Albania; AR, Argentina; AT, Austria; BA, Bosnia and Herzegovina; BE, Belgium; BG, Bulgaria; BO, Bolivia; BR, Brazil; CH, Switzerland; CL, Chile; CO, Colombia; CR, Costa Rica; CU, Cuba; CZ, Czech Republic; DK, Denmark; DO, Dominican Republic; EC, Ecuador; EE, Estonia; ES, Spain (18 of 19 regions); FI, Finland; FR, France; GE, Georgia; GR, Greece; GT, Guatemala; HN, Honduras; HR, Croatia; IL, Israel; IS, Iceland; LT, Lithuania; LV, Latvia; ME, Montenegro; NI, Nicaragua; NL, the Netherlands; NO, Norway; PA, Panama; PE, Peru; PL, Poland; PR, Puerto Rico; PT, Portugal; PY, Paraguay; RO, Romania; RS, Serbia; RU, Russia; SE, Sweden; SI, Slovenia; SK, Slovakia; SV, El Salvador; TR, Turkey; UA, Ukraine; UK, United Kingdom; UY, Uruguay; VE, Venezuela.
Source: Prepared by the authors, using study data.
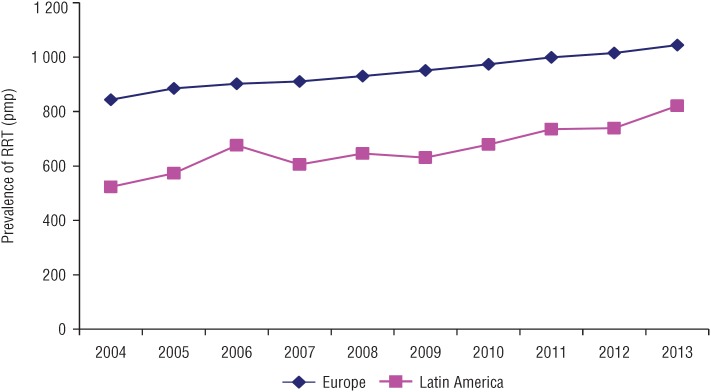
Trends in prevalence over time
We observed a consistent growth in the prevalence of RRT over the 10-year time frame (Figure 4). In the Latin American countries, the annual increase in the prevalence averaged 4.0% (95% CI: 2.5%-5.6%) from 2004 to 2013, while the European countries showed an average annual increase of 2.2% (95% CI: 2.0%-2.4%) for the same time period.
FIGURE 4. Trends in the prevalence of renal replacement therapy (RRT) per million population (pmp) in Europe and Latin America between 2004 and 2013a.
a Only data from registries that provided prevalence data from 2004 to 2013 were included (Supplementary Table S3).
Source: Prepared by authors, using study data.
Mortality rate and causes of death
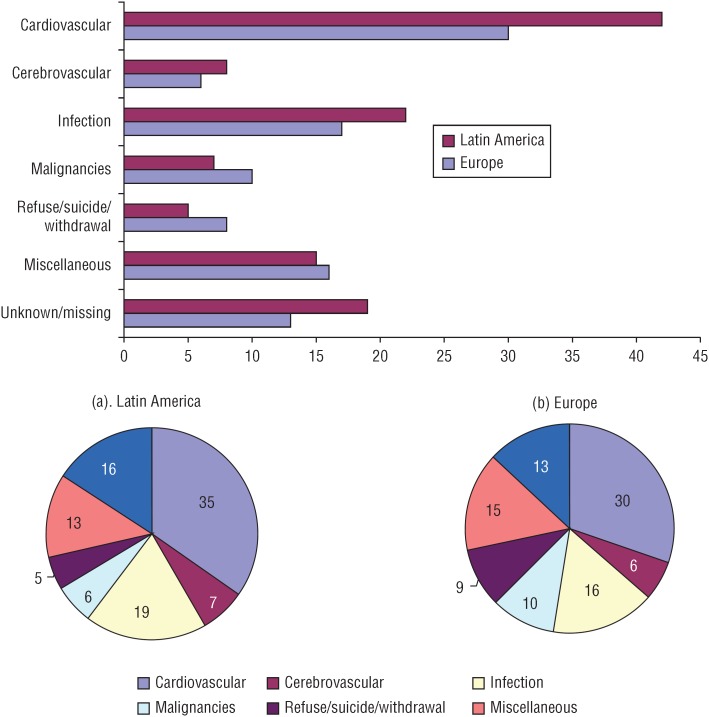
In 2013, the mortality rate was 112 deaths per 1 000 patient-years in Latin America and 100 deaths per 1 000 patient-years in Europe. Cardiovascular disease was the leading cause of death in both regions, representing 35% of the deaths in Latin America and 30% of the deaths in Europe, followed by infectious diseases and unknown causes (Figure 5).
FIGURE 5. Unadjusted mortality rate by causes of death of patients under renal replacement therapy per 1 000 patient-years and as a percentage in Latin America (A) and Europe (B)a.
a The values for Latin America are based on data from Argentina, Chile, Ecuador, Guatemala, and Uruguay; for Europe, the values are based on data from Austria, Belgium, Bosnia and Herzegovina, Denmark, Finland, Greece, Iceland, the Netherlands, Norway, Romania, Scotland, Serbia, Slovenia, Spain, and Sweden (Supplementary Table S3).
Source: Prepared by the authors, using study data.
DISCUSSION
Our results show that there are profound differences in the incidence and prevalence of RRT for ESRD between Latin America and Europe. We found a higher overall incidence of RRT in Latin America than in Europe. Although the subregion and the territories with the highest incidence (Jalisco (Mexico), Panama, and Puerto Rico) have not yet extended their health insurance coverage to 100% of the population, they do have programs for timely detection and treatment of CKD. However, there is no data available on important variables, such as age at the onset of RRT, primary renal disease, and mortality. This lack of data makes it difficult to explain the extremely high incidence rates in these particular territories/subregions. While a high prevalence of CKD stage 4 could potentially explain this finding, only a few countries in both the regions have data available on the stages of CKD before reaching ESRD. Colombia and Chile reported a prevalence of 1.0% and 0.3%, respectively, for CKD stage 4 (14-15). Moreover, investigators from Brazil recently published results from the ELSA cohort, including a prevalence of 4.8% for CKD stages 3, 4, and 5 combined in their country (16). Similarly, various European countries (Italy, Norway, Spain, Switzerland, and Turkey) reported a prevalence below 1% for CKD stage 4 (17-21). In order to perform reliable comparisons of the prevalence of CKD stage 4, more detailed data from a greater number of countries is needed.
In contrast, the incidence of RRT in patients above the age of 65 years is lower in Latin America than in Europe; the lower overall life expectancy in Latin America may play an important role in this difference. In addition, not all patients in Latin America may have access to dialysis treatment, while European nephrologists might be increasingly willing to start RRT in older patients. This means that the reported incidence of RRT may be an underestimation of the incidence of ESRD in Latin America, increasing the difference with Europe even further.
Kidney transplantation is more common in Europe, although this treatment modality is feasible and available in all Latin American countries. Nevertheless, hemodialysis is by far the most common RRT modality in Latin America. The difference between the two regions could be partly explained by a potential underestimation of patients with a functioning allograft in Latin America (10), due to underreporting of transplant procedures and/or the prevalence of functioning grafts.
In both regions, diabetes mellitus is the most common primary renal disease. However, the incidence of diabetes mellitus as a cause of ESRD in Latin America is almost twice as high as the incidence in Europe, probably because diabetes is more prevalent within the general population in Latin America. Furthermore, obesity is more prevalent in Latin America (9), which could lead to a higher incidence of diabetes. Conversely, in Latin America, the incidence of glomerulonephritis as a cause of renal failure is lower than in Europe. Glomerulonephritis may be underdiagnosed in the Latin American countries due to late referral to nephrologists, which in turn limits the possibility of performing a kidney biopsy (10). The proportion of patients with an unknown primary renal disease was higher in Latin America than in Europe. A lower frequency of kidney biopsy and the introduction of a new entity called Mesoamerican nephropathy might play a role. This disease predominantly affects young male agricultural workers from communities along the Pacific coast, especially those working in sugarcane fields (22-25). The cause of this disorder is still unknown.
In contrast with incidence, the prevalence of RRT for ESRD is higher in the European countries. This might in part be explained by somewhat lower crude mortality rates and the decades-long tradition of kidney transplantation in Europe. The size of the difference in patient survival between the two regions could be demonstrated by performing survival analyses while adjusting for potential confounders. However, it was not possible to perform these analyses because individual patient data was unavailable for the Latin American countries and was only available for some European countries. Previous studies have shown a relationship between the prevalence of RRT for ESRD and the number of nephrologists in a country (26, 27). Although data on the number of nephrologists per country was not available, lower numbers of nephrologists in Latin American countries could contribute to the difference in prevalence.
Hemodialysis was the most prevalent treatment of first choice in the Latin American countries, whereas in European countries the most common were kidney transplantation or hemodialysis. Peritoneal dialysis, although still underutilized, has a higher prevalence in the Latin American countries than in the European countries, possibly because many patients live further away from their treatment center (26-28). For these patients, a home-based dialysis treatment is preferred. In addition, the presumed reduced need for trained medical staff, lower costs, and minimal requirement for technical support may play a role in the popularity of peritoneal dialysis in Latin America.
GDP per capita and public health expenditure as a percent of GDP are both higher in the European countries. Various reasons may account for this difference. For example, in the Latin American countries, an association remains between GDP and the availability of specialized medical care (29). An additional explanation may be the mixed model of the health care system (private and public health insurance) in many of these countries.
Cardiovascular disease is the leading cause of death in the countries included in both registries, although in Latin America the rate of mortality due to cardiovascular disease is higher (41.9 versus 29.9 per 1 000 patient-years). This is probably due to a higher prevalence of diabetes mellitus as a cause of ESRD in these patients. Also, in the Latin American countries, there is a higher prevalence of diabetes, which is associated with increased risk of cardiovascular mortality.
Finally, this study has some strengths and limitations that should be recognized. The most important strength is that this is the first study comparing the epidemiology of RRT for ESRD between Latin America and Europe. The collaboration between two large international registries led to an extremely large number of patients who could be included in this study. However, there were also some limitations. First, not all of the national/subnational registries collect individual patient data, and in some countries part of the data was not available or was incomplete. As a consequence, adjustment for age was not possible, which hampers an unbiased comparison of the incidence, prevalence, and mortality rates between the two regions. The observed differences would probably be even larger after adjustment for age. We also had to reclassify the primary renal diseases and the causes of death. Although the differences were subtle, there is a possibility of misclassification in the categories of “others” or “miscellaneous.”
Conclusions
This study shows that there are considerable differences in the epidemiology of RRT for ESRD between Latin America and Europe. In 2013, the incidence of RRT was higher in Latin America, while Europe had a higher prevalence of RRT. In both Europe and Latin America, there was a positive association between GDP and the prevalence of RRT, but for Latin America a larger percentage of this increase could be explained by a rise in the GDP than was true for Europe. Finally, the mortality rates were higher in Latin America than in Europe, whereas cardiovascular disease was the most common cause of death in both regions.
Some of the results found could be explained by cultural differences, health and health care policies, and economic conditions. However, we were unable to perform a complete analysis due to the wide variation in the availability of data. For this reason, we recommend training nephrologists in the creation of renal registries in those countries that do not yet have them, and supporting members of existing renal registries in improving the quality of the data obtained.
Acknowledgments and funding
This paper was written by Rosario Luxardo et al. as part of the 2015–2016 ERA-EDTA/SLANH Registries fellowship. The ERA-EDTA Registry is funded by the European Renal Association-European Dialysis and Transplant Association (ERA-EDTA) and is an official body of the ERA-EDTA. We would like to thank the patients and staff of all the dialysis and transplant units that have contributed data via their national and subnational renal registries. In addition, we would like to thank all persons and organizations that have contributed to the work of the RLADTR and ERA-EDTA registries.
Footnotes
Suggested citation Luxardo R, Kramer A, González-Bedat MC, Massy ZA, Jager KJ, Rosa-Diez G, et al. The epidemiology of renal replacement therapy in two different parts of the world: the Latin American Dialysis and Transplant Registry versus the European Renal Association-European Dialysis and Transplant Association Registry. Rev Panam Salud Publica. 2018;42:e87. https://doi.org/10.26633/RPSP.2018.87
Disclaimer. Authors hold sole responsibility for the views expressed in the manuscript, which may not necessarily reflect the opinion or policy of the RPSP/PAJPH or PAHO.
Article collaborators. The persons who collaborated on this article, and their respective affiliation, are: Guillermo A. Alvarez Estevez, Sociedad Dominicana de Nefrología, República Dominicana; Patrice M. Ambühl, Swiss Dialysis Registry, Renal Division, Stadtspital Waid Zürich, Zurich, Switzerland; Anton M. Andrusev, Department of Peritoneal Dialysis, City Hospital #52, Moscow, Russian Federation; Emma Arcos Fuster, Catalan Renal Registry, Catalan Transplant Organization, Health Department, Generalitat of Catalonia, Barcelona, Spain; Federico E. Arribas Monzón, Departamento de Sanidad de Aragón, Dirección General de Asistencia Sanitaria, Zaragoza, Spain; Myftar Barbullushi, Service of Nephrology, University Hospital Center Mother Teresa, Tirana, Albania; Susana Barreto, Sociedad Paraguaya de Nefrología, Paraguay; Jadranka Buturovic-Ponikvar, Department of Nephrology, University Medical Centre Ljubljana, Slovenia; Julio Boj, Asociación Guatemalteca de Nefrología, Guatemala; Jose L. Cangiano, Sociedad de Nefrología e Hipertensión de Puerto Rico, Puerto Rico; Fergus J. Caskey, UK Renal Registry, Southmead Hospital, Bristol, United Kingdom; Pablo Castro de la Nuez, Sistema de Información de la Coordinación Autonómica de Trasplantes de Andalucía (SICATA), Andalucía, Spain; Harijs Cernevskis, Department of Internal Medicine, Riga Stradins University, Riga, Latvia; Frederic Collart, French-Belgian End Stage Renal Disease Registry, Brussels, Belgium; Cécile Couchoud, The Renal Epidemiology and Information Network Registry, Agence de la biomédecine, Saint-Denis La Plaine, France; Susana Elgueta, Sociedad Chilena de Nefrología, Chile; Guillermo García García, Asociación Nacional de Nefrólogos de México, México; Ramón García Trabanino, Asociación Salvadoreña de Nefrología e Hipertensión, El Salvador; Liliana Garneata, Carol Davila University of Medicine and Pharmacy, Department of Internal Medicine and Nephrology, Dr. Carol Davila Teaching Hospital of Nephrology, Bucharest, Romania; Eliezer Golan, Department of Nephrology and Hypertension, Meir Medical Center, Kfar-Saba and Sackler Faculty of Medicine, Tel Aviv, Israel; Rafael A. Gomez Acevedo, Asociación Colombiana de Nefrología e Hipertensión, Colombia; Marc H. Hemmelder, Dutch Renal Registry Renine, Nefrovisie Foundation, Utrecht, the Netherlands; Agualuz Hernandez, Asociación Guatemalteca de Nefrología, Guatemala; Fabio Hernandez, Asociación Costarricense de Nefrología, Costa Rica; Kyriakos Ioannou, Nephrology Department, Apollonion Private Hospital, Nicosia, Cyprus; Mykola Kolesnyk, National Register of Chronic Kidney Disease and Acute Kidney Injury Patients, State Institute of Nephrology, National Academy of Medical Sciences of Ukraine, Kiev, Ukraine; Myrto Kostopoulou, Nephrology Department, General Hospital of Athens G. Gennimatas, Athens, Greece; Frantisek Lopot, General University Hospital, Department of Medicine, Prague - Strahov, Czech Republic; Fernando Macario, Portuguese Society of Nephrology, Nephrology Department, University Hospital of Coimbra, Coimbra, Portugal; Beatriz Mahillo-Duran, Spanish Renal Disease Patients Registry (REER), Organización Nacional de Trasplantes (ONT), Madrid, Spain; Natasa Maksimovic, Institute of Epidemiology, Faculty of Medicine, University of Belgrade, Belgrade, Serbia; Sergio Marinovich, Sociedad Argentina de Nefrología, Buenos Aires, Argentina; Orleans Mendez, Sociedad Venezolana de Nefrología, Venezuela; Pedro Orduñez, Pan American Health Organization, Washington, D.C., United States of America; Fabian Ortiz, Sociedad Ecuatoriana de Nefrología, Ecuador; Mireya Ortiz, Sociedad Chilena de Nefrología, Chile; Runolfur Palsson, Division of Nephrology, Landspítali (National University Hospital of Iceland), Reykjavik, Iceland; Ülle Pechter, Department of Internal Medicine, Tartu University, Tartu, Estonia; Carlos Pereda, Sociedad Peruana de Nefrologia, Peru; Jorge Perez-Oliva, Sociedad Cubana de Nefrología, Cuba; Maria Pippias, European Renal Association-European Dialysis and Transplant Association Registry, Department of Medical Informatics, Academic Medical Center, University of Amsterdam, Amsterdam Public Health Research Institute, Amsterdam, the Netherlands; Hugo Poblete, Sociedad Chilena de Nefrología, Chile; Marina Ratkovic, Nephrology and Hemodialysis, Clinical Center of Montenegro, Podgorica, Montenegro; Halima Resic, Clinic for Hemodialysis, Clinical Center University of Sarajevo, Sarajevo, Bosnia and Herzegovina; Gaspar Rodriguez, Sociedad Hondureña de Nefrología, Honduras; Boleslaw Rutkowski, Polish Renal Registry, Department of Nephrology, Transplantology and Internal Medicine, Medical University, Gdansk, Poland; Carmen Santiuste de Pablos, Registro de Enfermos Renales de la Región de Murcia, Servicio de Epidemiología, Consejería de Sanidad, Instituto Murciano de Investigación Biosanitaria-Arrixaca, Murcia, Spain; Ricardo Sesso, Sociedade Brasileira de Nefrologia, São Paulo, Brasil; Nica Silva, Asociación Nacional de Nefrólogos de México, México; Viera Spustova, Slovak Medical University, Bratislava, Slovakia; Jamie Traynor, The Scottish Renal Registry, Information Services Division, Glasgow, Scotland, United Kingdom; Regulo Valdez, Asociación Panameña de Nefrología e Hipertensión, Panamá; Jose Luis Valencia, Sociedad Boliviana de Nefrología, Bolivia; Bård E Waldum-Grevbo, Department of Nephrology, Oslo University Hospital Ullevål, Oslo, Norway; Edita Ziginskiene, Lithuanian Nephrology, Dialysis and Transplantation Association, Kaunas, Lithuania.
REFERENCES
- 1.Caskey FJ, Jager KJ. A population approach to renal replacement therapy epidemiology: lessons from the EVEREST study. Nephrol Dial Transplant. 2014;29(8):1494–1499. doi: 10.1093/ndt/gft390. [DOI] [PubMed] [Google Scholar]
- 2.Cusumano A, Garcia Garcia G, Gonzalez-Bedat M, Marinovich S, Lugon J, Poblete-Badal H, et al. Latin American Dialysis and Transplant Registry: 2008 prevalence and incidence of end-stage renal disease and correlation with socioeconomic indexes. Kidney Int Suppl. 2013;3(2):153–156. doi: 10.1038/kisup.2013.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosa-Diez G, Gonzalez-Bedat M, Pecoits-Filho R, Marinovich S, Fernandez S, Lugon J, et al. Renal replacement therapy in Latin American end-stage renal disease. Clin Kidney J. 2014;7(4):431–436. doi: 10.1093/ckj/sfu039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Just PM, Charro FT, Tschosik EA, Noe LL, Bhattacharyya SK, Riella MC. Reimbursement and economic factors influencing dialysis modality choice around the world. Nephrol Dial Transplant. 2008;(23):2365–2373. doi: 10.1093/ndt/gfm939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liyanage T, Ninomiya T, Jha V, Neal B, Patrice HM, Okpechi I, et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. 2015;385:1975–1982. doi: 10.1016/S0140-6736(14)61601-9. [DOI] [PubMed] [Google Scholar]
- 6.Boerma T, Mathers C, AbouZahr C, Chatterji S, Hogan D, Stevens G, et al. Health in 2015: from MDGs, Millennium Development Goals to SDGs, Sustainable Development Goals. Geneva: World Health Organization; 2015. [Google Scholar]
- 7.Caskey F, Kramer A, Elliott R, Stel VS, Covic A, Cusumano A, et al. Global variation in renal replacement therapy for endstage renal disease. Nephrol Dial Transplant. 2011;26:2604–2610. doi: 10.1093/ndt/gfq781. [DOI] [PubMed] [Google Scholar]
- 8.World Bank DataBank. [Accessed on 1 April 2016]. Available from: http://databank.worldbank.org/data/home.aspx.
- 9.World Health Organization Global Health Observatory data repository. Risk factors. [Accessed on 1 April 2016]. Available from: http://apps.who.int/gho/data/node.main.A867?lang=en.
- 10.Gonzalez-Bedat M, Rosa-Diez G, Pecoits-Filho R, Ferreiro A, Garcia-Garcia G, Cusumano A, et al. Burden of disease: prevalence and incidence of ESRD in Latin America. Clin Nephrol. 2015;83(Suppl 1):3–6. doi: 10.5414/cnp83s003. [DOI] [PubMed] [Google Scholar]
- 11.ERA-EDTA Registry . ERA-EDTA Registry annual report 2013. Amsterdam: Academic Medical Center, Department of Medical Informatics; 2015. [Google Scholar]
- 12.Eurostat Eurostat. [Accessed on 1 April 2016]. Available from http://ec.europa.eu/eurostat.
- 13.U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute [Accessed on 1 April 2016];Joinpoint trend analysis software. Version 4.0.4 - May 2013. Available from: https://surveillance.cancer.gov/joinpoint/download.
- 14.Fondo Colombiano de Enfermedades de Alto Costo . Situación de la enfermedad renal crónica en Colombia. Bogotá: Fondo Colombiano de Enfermedades de Alto Costo; 2015. [Google Scholar]
- 15.Zuniga SMC, Muller OH, Flores OM. [Prevalence of chronic kidney disease in subjects consulting in urban primary care clinics] Rev Med Chil. 2011;139(9):1176–1184. [PubMed] [Google Scholar]
- 16.Barreto SM, Ladeira RM, Duncan BB, Schmidt MI, Lopes AA, Benseñor IM, et al. Chronic kidney disease among adult participants of the ELSA-Brasil cohort: association with race and socioeconomic position. J Epidemiol Community Health. 2016;70(4):380–389. doi: 10.1136/jech-2015-205834. [DOI] [PubMed] [Google Scholar]
- 17.Otero A, de Francisco A, Gayoso P, García F, EPIRCE Study Group Prevalence of chronic renal disease in Spain: results of the EPIRCE study. Nefrologia. 2010;30(1):78–86. doi: 10.3265/Nefrologia.pre2009.Dic.5732. [DOI] [PubMed] [Google Scholar]
- 18.Hallan SI, Ovrehus MA, Romundstad S, Rifkin D, Langhammer A, Stevens PE, et al. Long-term trends in the prevalence of chronic kidney disease and the influence of cardiovascular risk factors in Norway. Kidney Int. 2016;90(3):665–673. doi: 10.1016/j.kint.2016.04.012. [DOI] [PubMed] [Google Scholar]
- 19.Gambaro G, Yabarek T, Graziani MS, Gemelli A, Abaterusso C, Frigo AC, et al. Prevalence of CKD in northeastern Italy: results of the INCIPE study and comparison with NHANES. Clin J Am Soc Nephrol. 2010;5(11):1946–1953. doi: 10.2215/CJN.02400310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suleymanlar G, Utas C, Arinsoy T, Ates K, Altun B, Altiparmak MR, et al. A population-based survey of Chronic REnal Disease In Turkey--the CREDIT study. Nephrol Dial Transplant. 2011;26(6):1862–1871. doi: 10.1093/ndt/gfq656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ponte B, Pruijm M, Marques-Vidal P, Martin PY, Burnier M, Paccaud F, et al. Determinants and burden of chronic kidney disease in the population-based CoLaus study: a cross-sectional analysis. Nephrol Dial Transplant. 2013;28(9):2329–2339. doi: 10.1093/ndt/gft206. [DOI] [PubMed] [Google Scholar]
- 22.Correa-Rotter R, Wesseling C, Johnson RJ. CKD of unknown origin in Central America: the case for a Mesoamerican nephropathy. Am J Kidney Dis. 2014;63(3):506–520. doi: 10.1053/j.ajkd.2013.10.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wesseling C, Crowe J, Hogstedt C, Jakobsson K, Lucas R, Wegman DH, et al. Resolving the enigma of the Mesoamerican nephropathy: a research workshop summary. Am J Kidney Dis. 2014;63(3):396–404. doi: 10.1053/j.ajkd.2013.08.014. [DOI] [PubMed] [Google Scholar]
- 24.Garcia-Trabanino R, Hernandez C, Rosa A, Domínguez Alonso J. [Incidence, mortality, and prevalence of endstage chronic renal disease in the Bajo Lempa region of El Salvador: a ten-year community registry] Nefrologia. 2016;36(5):517–522. doi: 10.1016/j.nefro.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 25.Wesseling C, van Wendel de Joode B, Crowe J, Rittner R, Sanati NA, Hogstedt C, et al. Mesoamerican nephropathy: geographical distribution and time trends of chronic kidney disease mortality between 1970 and 2012 in Costa Rica. Occup Environ Med. 2015;72(10):714–721. doi: 10.1136/oemed-2014-102799. [DOI] [PubMed] [Google Scholar]
- 26.Caskey F, Stel V, Elliott R, Jager KJ, Covic A, Cusumano A, et al. The EVEREST study: an international collaboration. NDT Plus. 2010 Feb;3(1):28–36. doi: 10.1093/ndtplus/sfp146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sharif MU, Elsayed ME, AG S. The global nephrology workforce: emerging threats and potential solutions! Clin Kidney J. 2016;9(1):11–22. doi: 10.1093/ckj/sfv111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jain AK, Blake P, Cordy P, Garg AX. Global trends in rates of peritoneal dialysis. J Am Soc Nephrol. 2012;23:533–544. doi: 10.1681/ASN.2011060607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Slade EP, Anderson GF. The relationship between per capita income and diffusion of medical technologies. Health Policy. 2011;58(1):1–14. doi: 10.1016/s0168-8510(01)00151-8. [DOI] [PubMed] [Google Scholar]