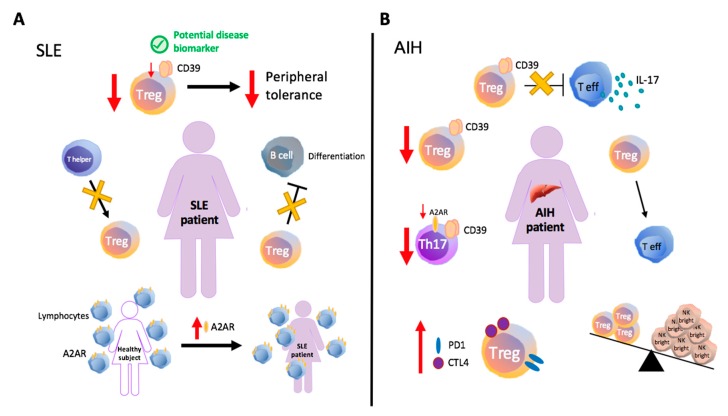
Figure 1.
Immune and purinergic dysregulation in systemic lupus erythematosus (SLE) and autoimmune hepatitis (AIH). (A) In SLE, defects in ENTPD1/CD39 expression and impaired Treg function have been associated with loss of peripheral tolerance. Studies conducted in active SLE patients have indicated impaired suppression of B-cell differentiation and identified the abnormal generation of regulatory T-cells (Treg) as result of limited transition from inducer/helper to suppressor phenotype. Upregulation of A2AR is detectable in SLE patients, likely being linked to activation of compensatory pathways. (B) In type 1 autoimmune hepatitis (AIH-1), CD39+ Treg cells display impaired suppression of IL-17 production by CD4+ effectors. Acute AIH patients present a low ratio between Tregs and NK bright cells, a specific NK subset with activated effector phenotype. Activated memory phenotype and signs of exhaustion, including increased CTLA-4 and PD-1 levels are also typical of AIH Tregs. Reduced CD39+ Treg and CD39+ Th17-cell frequencies positively correlate with the disease progression and might result from cell instability upon pro-inflammatory challenge, with increased rate of conversion into effector lymphocytes. The reduction in CD39+ Th17-cell numbers, also associates with lower A2AR expression (see text below).