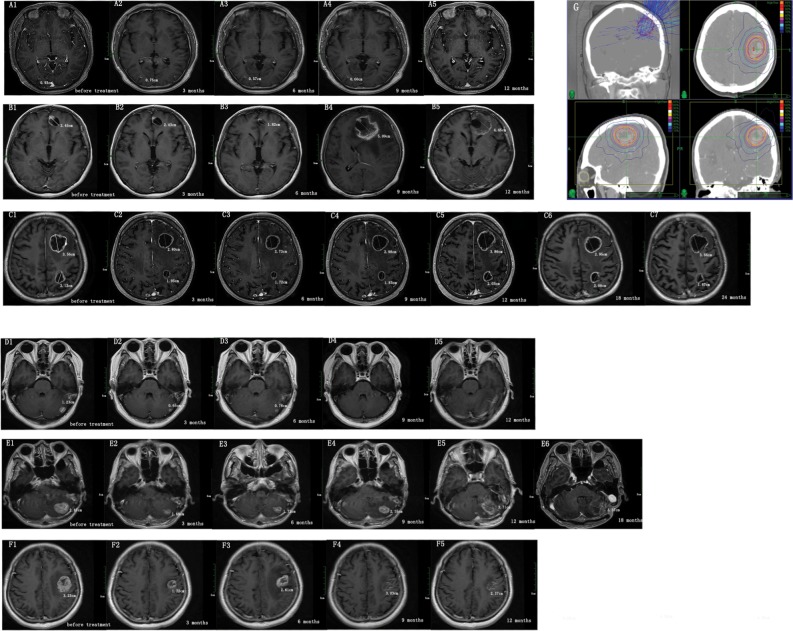
Figure 4.
The volume change in patients with cystic and solid brain metastases after CyberKnife treatment.
Notes: We measured the longest diameter of brain metastases at diagnosis (before treatment) and 3, 6, 9, and 12 months after radiosurgery treatment in axial contrast-enhanced T1-weighted magnetic resonance images. (A–C) Cystic brain metastases images. (D–F) Solid brain metastases images. (A1, B1, C1, D1, E1, F1) Brain metastases images before radiosurgery treatment. The change in volume of brain metastases (A2–A5, B2–B5, C2–C5, D2–D5, E2–E5, F2-F5) over time. (A) A 40-year-old woman with lung cancer received WBRT before radiosurgery treatment. The prescription dose and fraction schedule was 14 Gy/1F. (B) A 44-year-old woman with breast cancer, without prior WBRT. The prescription dose and fraction schedule was 30 Gy/3F. (C) A 74-year-old man with lung cancer, without prior WBRT. The prescription dose and fraction schedule was 32 Gy/4F. (D) A 51-year-old woman with lung cancer, without prior WBRT. The prescription dose and fraction schedule was 20 Gy/1F. (E) A 74-year-old man with lung cancer, without prior WBRT. The prescription dose and fraction schedule was 30 Gy/2F. (F) A 65-year-old woman with endometrial cancer, without prior WBRT. The prescription dose and fraction schedule was 30 Gy/3F. (G) Typical dose distribution images by CyberKnife plans.
Abbreviation: WBRT, whole brain radiotherapy.