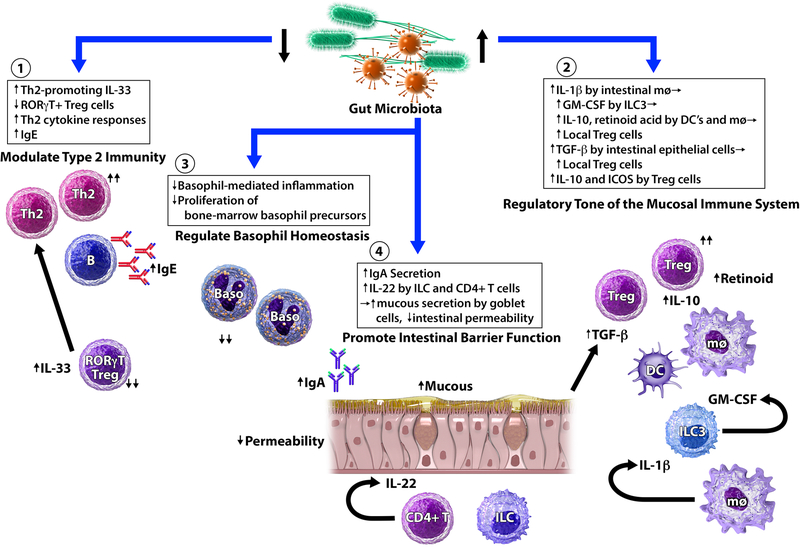
Figure 1. Mechanisms by which gut microbiota may affect food allergy susceptibility.
Murine models of food allergy have shown that gut microbiota interact with multiple aspects of the intestinal mucosa, innate immunity, and adaptive immunity. (1) Gut microbiota modulate type 2 immunity. In germ-free mice, expression of Th2-promoting cytokine IL-33 by epithelial cells is increased. In contrast, Th2-inhibiting RORγt+ Treg cells are profoundly reduced in both germ-free and antibiotic-treated mice. As a result, Th2-associated pathology is exacerbated and IgE levels are elevated in the absence of key microbial signals. (2) Gut microbiota influence immune development and tolerance. Microbial colonization promotes the expansion of Treg cells. Microbial signals promote IL-1β secretion by intestinal macrophages (mφ), which leads to GM-CSF release by type 3 innate lymphoid cells (ILC3). As a result, IL-10 and retinoid acid secretions by dendritic cells (DC) and mφ are elevated, which leads to the expansion of local Treg cells. Strain-specific Clostridia colonization of gnotobiotic mice stimulates the secretion of TGF- β from intestinal epithelial cells, leading to the expansion of colonic Treg cells. Strain-specific Clostridia colonization also induces key anti-inflammatory molecules (IL-10 and ICOS) in Treg cells. (3) Gut microbiota regulate basophil populations. Circulating basophil levels increase in antibiotic-treated mice. Conversely, the presence of microbial signals limits the proliferation of bone-marrow basophil precursors, and reduces basophil-mediated allergic inflammation. (4) Gut microbiota promote intestinal barrier function. Selective colonization of germ-free mice with certain strains of Clostridia and Bacteroides promotes intestinal IgA secretion, which can contribute to immune exclusion and reduce allergen uptake. Strain-specific Clostridia colonization of germ-free mice also induces IL-22 production by innate lymphoid cells (ILC) and CD4+ T cells. IL-22, in turn, promotes mucous secretion by goblet cells and reduces intestinal permeability to dietary allergens. Adapted from Ho and Bunyavanich, Curr Allergy Asthma Rep. 2018 Apr 5;18(4):27.