Abstract
This analysis uses network and spatial data to identify optimal individuals to target with overdose prevention interventions in rural Appalachia. Five hundred and three rural persons who use drugs were recruited to participate in the Social Networks among Appalachian People Study (2008–2010). Interviewer-administered surveys collected information on demographic characteristics, risk behaviors (including overdose history), network members, and residential addresses. We restricted the sample to individuals with at least one confirmed relationship to another study participant (N = 463). Using dyadic analyses (N = 1428 relationships), we identified relationship-level correlates of relationships with network members who have previously overdosed. We then examined individual- and network-level factors associated with (1) having at least one first-degree alter (i.e., network member) with a prior overdose and (2) each additional network member with a prior overdose (N = 463 study participants). Overall, 28% of the sample had previously overdosed and 57% were one-degree away from someone who previously overdosed. Relationships with those who had overdosed were characterized by closer residential proximity. Those with at least one network member who previously overdosed were more geographically central and occupied more central network positions. Further, the number of network members with an overdose history increased with decreasing distance to the town center, increasing network centrality, and prior enrollment in an alcohol detox program. Because fatal overdoses can be prevented through bystander intervention, these findings suggest that strategies that target more central individuals (both geographically and based on their network positions) and those who have previously enrolled in alcohol detox programs with overdose prevention training and naloxone may optimize intervention reach and have the potential to curb overdose fatalities in this region.
Keywords: Overdose, Rural, Social network analysis, Spatial analysis, Appalachia, Persons who use drugs
Introduction
According to the Centers for Disease Control and Prevention (CDC), unintentional poisoning, primarily from drug overdose, is the leading cause of injury-related death among Americans aged 25–64 [1]. Between 1999 and 2016, age-adjusted overdose mortality rates increased by 300%, with the largest increase between 2014 and 2016 (18% per year) [2]. Over the course of the epidemic, there have been shifts in the geographic areas most impacted by and in the patterns of drugs involved in overdose deaths. For example, overdose death rates were consistently higher in urban areas than in rural areas until 2004 when they converged [3]. After this point, there was a shift in the epidemic from one primarily driven by heroin use in urban settings to one which disproportionately impacted rural areas where prescription opioid use was more prevalent [4, 5]. The rate of overdose deaths involving synthetic opioids (i.e., fentanyl, fentanyl analogs, and tramadol) increased steadily between 1999 and 2006, did not change statistically between 2006 and 2013, and then increased by 88% per year between 2013 and 2016. Overdose death rates involving natural and semisynthetic opioids (i.e., morphine, codeine, hydrocodone, and oxycodone) increased by 440% between 1999 and 2016 with the largest increases between 1999 and 2009 (13% increase per year) [2].
Although morbidity and mortality attributed to prescription opioids have increased in all states, the increased burden in rural areas is disproportionately high [6, 7], even after accounting for population density [8]. For example, CDC overdose fatality data show a persistent and growing overdose epidemic in rural Eastern Kentucky between 1999 and 2016. In 2016, Kentucky’s drug overdose mortality rate was ranked 5th in the nation and its neighboring states West Virginia and Ohio ranked 1st and 2nd, respectively [9]. Between 2000 and 2010, Kentucky’s overdose fatality rate increased by 282%. The mortality rate continued to increase between 2010 and 2016 (23.6 to 33.5 deaths per 100,000 population) [10]. According to the 2017 Overdose Fatality Report published by the Commonwealth of Kentucky, heroin and fentanyl were involved in 22% and 52% of overdose deaths that year, respectively. Other drugs detected included morphine (43%), alprazolam (36%), gabapentin (31%), methamphetamine (29%), oxycodone (14%), and hydrocodone (14%) [11].
Some attribute rural-urban differences to (1) steeper increases in prescription pain medication availability in rural than urban areas, (2) rural-to-urban migration among youth which leads to greater economic deprivation and an increased risk for illicit drug use among young adults who stay, (3) kinship networks which facilitate diversion and distribution, and (4) more stressful environments due to greater economic deprivation and unemployment which increase one’s risk for substance use [12]. The increased availability of prescription opioids in rural parts of Eastern Kentucky is thought to have resulted from more aggressive marketing of prescription opioids to rural Appalachian communities [13] and a higher prevalence of chronic pain conditions indicating treatment with prescription opioids (i.e., an older population due to out-migration of youth and chronic pain conditions resulting from heavy labor occupations common in this region) [12]. This is consistent with findings from analyses using Kentucky Medicaid data which demonstrated that prescription claims for OxyContin® were significantly higher in areas of distressed Appalachia than in other regions of the state [14]. Collectively, the increased prescribing of opioids in the Appalachian states [15], lower density of substance use and mental health facilities in rural areas [16], inadequate access to addiction treatment for prescription drug use disorder [8], and differences in health care use in rural and urban areas [16] contribute to the observed disparities.
Opioid-related overdoses are not instantaneous [17], are frequently witnessed by others [18], and can be reversed by naloxone administration and emergency care. Even in the absence of naloxone, stimulation and rescue breathing performed before emergency medical services arrive can dramatically improve one’s chance of survival [18, 19]. Therefore, targeted training in overdose prevention and distribution of naloxone to those most likely to witness an overdose could effectively reduce the overdose fatality rate. To draw a comparison with herd immunity from the infectious disease literature, the herd immunity threshold is reached when a critical portion of the population becomes immune. In the context of overdose prevention where the “disease” is a fatal overdose, immunity can be thought of as immunity to a fatal overdose. Training in overdose prevention can function similarly to a vaccine, whereby bystanders with training in overdose prevention and access to naloxone can reduce the probability of death for a given overdose. Because overdose events cluster spatially [20–22] and are more common among those with higher risk network members [23], those living in areas where overdoses are more prevalent or who associate with higher risk network members may also be more likely to witness an overdose. Therefore, to create herd immunity, overdose prevention training should target those most likely to witness an overdose (e.g., those living in geographic areas where overdose is more likely and who are socially connected to one or more others at risk for overdose). The goal of this analysis is to use network and spatial data to identify optimal individuals to target with overdose prevention interventions.
Methods
Sample
The data for this analysis were collected through baseline assessments for the Social Networks among Appalachian People (SNAP) study, an ongoing, longitudinal study of 503 persons who use drugs in rural Eastern Kentucky. SNAP methods are described in detail elsewhere [24]. In brief, participants were recruited through respondent-driven sampling between 2008 and 2010 [25]. The protocol was approved by the Institutional Review Board at the University of Kentucky and a Certificate of Confidentiality was obtained.
Individual Data
Participants completed interviewer-administered surveys which collected residential addresses, demographic characteristics, risk behaviors (including overdose history), and information about recent (past 6-month) drug co-usage, sex, and social support network members. From the individual-level data, we created a variable, “transportation access,” which was defined as having a valid driver’s license and access to an automobile. Of note, public transportation is not available in this region. Overdose history was a binary variable created based on the response to the question, “Have you ever overdosed?” (yes vs. no).
Network Data
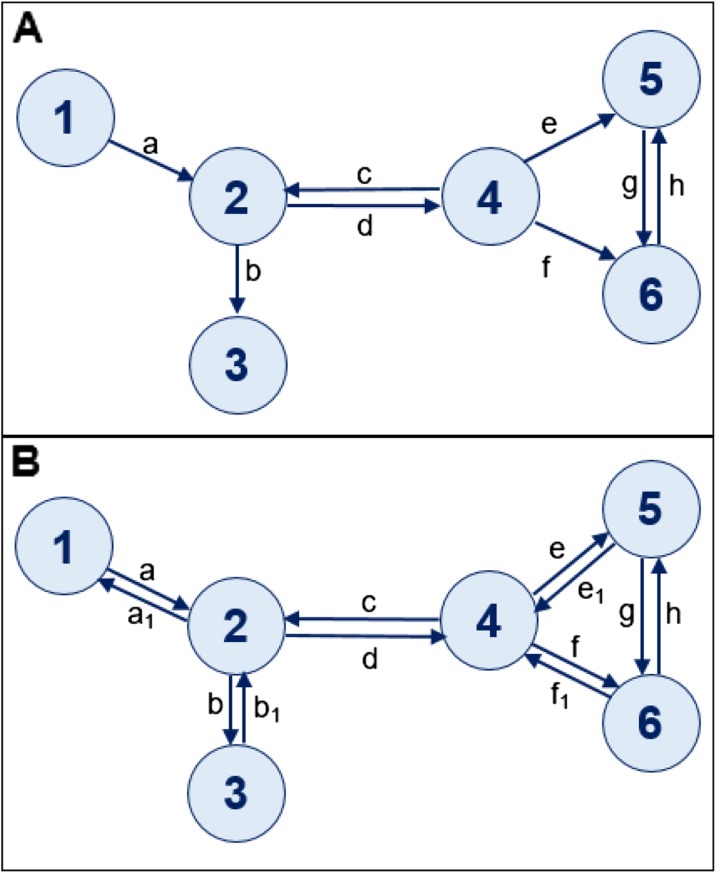
Participants provided the first name and first letter of the last name for up to 24 different individuals with whom they had sex, used drugs, or counted on for emotional, financial, material, or informational support [26, 27]. Demographic characteristics and relational data (i.e., duration of the relationship in months, trust in the network member listed (ordinal scale from 0 to 10, with 10 indicating the highest level of trust), and whether the network member was a relative (and if so, an immediate or distant relative)) were also collected about each network member named. Network member names and demographic characteristics were cross-referenced with those of study participants and network members named by other study participants to construct a network comprised of all confirmed relationships between study participants. If at least one individual indicated a relationship with another participant, a relationship was considered to be present. More detail on the network building process is provided elsewhere [28]. This resulted in 897 relationships (183 reciprocated and 531 non-reciprocated) and 1428 first-degree ties (i.e., 714 one-degree paths in both directions). An example of how the network data were derived for this analysis is provided in Fig. 1.
Fig. 1.
Example network data for this analysis. a Eight directed ties. Of these, 4 are reciprocal ties (c, d, g, and h) and 4 are unreciprocated, or one-directional ties (a, b, e, and f). For the analyses presented in this paper, we assumed that a relationship between two individuals existed if at least one person in the pair indicated knowing the other person in the pair. For example, in a, individual 1 reported knowing individual 2, but individual 2 did not report knowing individual 1. b The symmetrized or undirected version of (a). For the dyadic analyses, which focused on relationships, we assumed (as shown in b) that if at least one individual reported a relationship to another, that the tie was reciprocated. Thus, b shows two arrows between these individuals (a and a1). The dyadic analysis in this example would therefore consists of 12 ties and an individual-level analysis would include 6 individuals. As displayed in b, this means that there are two one-degree paths (i.e., one in either direction) between all connected nodes in the network. Dyadic analyses require that there be information on the relationship between the two individuals. In cases like the relationship between individual 2 and individual 4, each individual provided information about the relationship with the other and this information may not agree. For example, the relationship information reported by individual 2 (represented by tie d) and by individual 4 (represented by tie c) may be different. We therefore used information reported about the relationship between 4 and 2 by individual 4 (represented by tie c) for analyses interested in the directed path between 4 and 2; and information about the relationship reported by 2 (represented by tie d) for the directed path between 2 and 4. In scenarios where only one individual in the pair reported knowing the other (i.e., the tie represented by a between individuals 1 and 2), we used the information about the relationship reported by individual 1 for the path represented by both a and a1 in (b). For the egocentric analyses, we assumed that individuals 1 and 3 had only one first-degree network member, individuals 5 and 6 had two first-degree network members, and individuals 2 and 4 had 3 first-degree network members
Spatial Data
Participants’ residential addresses and the address of the study storefront were geo-coded in ArcGIS. Using the network analyst extension in ArcGIS 10.1 and the North America Detailed Streets Layer Package [29], we computed the shortest road-network distance in miles between each pair of participants in the data set and between each participant and the study storefront. Because the study storefront is located in the center of town, we used this location as a proxy for the town center, which is more densely populated than other regions of the study area. Because the distance variable was not normally distributed, we used the log-transformed variable for model building, but retained the untransformed variable in the unadjusted analyses to aid with interpretation. Of note, only the log-transformed distance variable was considered for inclusion in the adjusted model.
Network Analysis
The network data for this analysis included only those who listed (or were listed as a network member by) at least one other person in the study sample (N = 463). A directed network (i.e., like the example shown in Fig. 1a) indicates the direction of each relationship. Using the directed network (n = 897 ties), we computed in-degree (i.e., number of times an individual has been nominated by others in the sample), out-degree (i.e., number of other individuals in the sample a person nominates), and betweenness centrality (i.e., extent to which an individual lies on the shortest path between two other individuals in the sample) for each individual using UCINET [30]. In order to compute first-degree ties (i.e., individuals who are directly connected to one another), we symmetrized the network data set (see example in Fig. 1b) and assumed all relationships were reciprocal if at least one member of the pair reported knowing the other (n = 1428 ties; 714 one-way paths in each direction). In other words, any tie between two individuals (reciprocated or unreciprocated) counts as two one-way relationships between the connected individuals. This assumption of symmetric connections is common in the social sciences [31]. In this context, it is reasonable to assume that if one person lists another person as a sex partner, drug partner, or person who provides him/her with some type of support, that the two individuals know one another. For the 183 reciprocated relationships, we used relationship-level information (i.e., relationship duration, trust level, and whether the network member was a relative (and if so, an immediate relative)) provided by each ego about the dyad even if the responses provided by the pair did not agree with one another (366 one-degree paths). For the 531 unreciprocated pairs (1062 one-degree paths), we used the relationship-level information provided by the one member of the pair who reported knowing the other, for both pairs. For example, if person A reported knowing person B for 10 years and person B did not report knowing person A, we assumed that A and B knew one another and that the relationship duration for A ➔ B and B ➔ A were both 10 years (See example in Fig. 1). Using dyadic analyses that clustered on egos using generalized estimating equations (GEE), we identified relationship-level correlates of ties to alters with a history of overdose (N = 1428 ties) in STATA 14 [32]. The final dyadic model was built using variables that were statistically significant at an alpha level of 0.05 in the unadjusted analyses and which retained statistical significance after adjusting for personal overdose history. We also conducted a sensitivity analysis where we did not assume reciprocal relational characteristics, and instead only used information reported by each ego about his/her relationships with each alter listed (n = 897 ties).
We then examined individual- and network-level factors associated with (1) having ≥ 1 first-degree alter (referred to as “network member,” hereafter) with a prior overdose and [2] each additional first-degree alter (i.e., “network member”) with a prior overdose. Of note, overdose history was self-reported. The final individual-level model was built using variables that were statistically significant at an alpha level of 0.05 in the unadjusted analyses and which retained statistical significance after adjusting for other significant covariates.
The sample size for dyadic analyses was 1428 ties (the sensitivity analysis had a restricted sample size of 897 ties) and the sample size for the individual-level analysis was 463 individuals.
Results
Baseline characteristics have been previously described [24–27, 33–35]. In the sample used for this analysis, 28.3% of individuals had previously overdosed and 57.2% were one-degree away from someone who had previously overdosed (i.e., listed or were listed by another person in the confirmed network sample who self-reported at least one prior overdose in their lifetime). Of the 131 people in the sample who previously overdosed, the average person reported 2.4 prior overdoses in their lifetime (median = 2; interquartile range (IQR) 1–3). The median sample age was 31 years (IQR 26–38), the median number of years living in Eastern Kentucky was 29 (IQR: 23–35), and 94% of the sample were white and 56% were male.
On average, individuals had 3.08 network members, of whom an average of 0.83 self-reported at least one prior overdose. The average person lived 5.7 miles from the town center and those who had previously overdosed or who had at least one network member who had previously overdosed lived significantly closer to the town center (4.5 miles and 4.8 miles, respectively). Further, as the number of network members with a prior overdose increased, so did average residential proximity to the town center (i.e., 6.9 miles for 0 alters, 5.1 miles for 1 alter, 4.3 miles for 2 alters, 3.6 miles for 3 alters, and 1.4 miles for 4 or more alters with an overdose history; p = 0.002). The proportion of alters who had previously overdosed was also higher for those living closer to the town center. Further, the average distance between first-degree network members in the sample was 3.9 miles and was shorter between pairs where at least one individual had previously overdosed (3.2 miles between pairs with at least one member who had previously overdosed vs. 4.1 miles between pairs where neither had previously overdosed).
As seen in Table 1, individuals who had previously overdosed were more likely to have one-degree relationships to others with a history of overdose (p = 0.044). Prior to adjustment, relationships to those who self-reported at least one prior overdose were less trusting and more geographically proximal relationships. After adjusting for personal overdose history, residential proximity was the only remaining statistically significant correlate of relationships to network members with a prior overdose.
Table 1.
Dyadic analysis: unadjusted and adjusted relationship-level correlates of first-degree relationships to network members with a history of overdose (N = 1428)
| Bivariate statistics | Multivariable GEE model | |||||
|---|---|---|---|---|---|---|
| ALL (N = 1428) | Network member who previously overdosed (N = 384) | Network member who did not previously overdose (N = 1044) | Odds ratio for having a network member with vs. without a prior overdose | |||
| N (%) | N (%) | N (%) | P value1 | AOR | 95% CI | |
| Relationship-level variables (past 6 months) | ||||||
| Social support | 545 (38.17) | 143 (37.24) | 402 (38.51) | 0.661 | ||
| Exchange of financial support | 311 (21.78) | 85 (22.14) | 226 (21.65) | 0.844 | ||
| Co-usage of drugs | 1288 (90.20) | 351 (91.41) | 937 (89.75) | 0.334 | ||
| Sex partner | 385 (25.96) | 105 (27.34) | 280 (26.82) | 0.846 | ||
| Drug co-usage and sexual partner | 311 (21.78) | 87 (22.66) | 224 (21.46) | 0.627 | ||
| Family member | 433 (30.32) | 122 (31.77) | 311 (29.79) | 0.469 | ||
| Immediate family member2 | 274 (19.19) | 84 (21.88) | 190 (18.20) | 0.124 | ||
| Trust (1 = do not trust at all; 10 = trust with your life), median (IQR) | 7 (5–9.5) | 6(4–9) | 8 (5–10) | 0.002 | ||
| Relationship duration in years, median (IQR) | 10 (4–23) | 10 (4–24.5) | 10 (3.5–23) | 0.128 | ||
| Distance between ego and alter (miles)3, median (IQR) | 1.70 (0.16–5.36) | 1.34 (0.06–4.84) | 1.83 (0.20–5.44) | 0.013 | ||
| Log of the distance between ego and alter (miles)3,4, median (IQR) | .53 (−1.84–1.68) | 0.29 (−2.82–1.58) | 0.60 (−1.63–1.69) | 0.005 | 0.95 | 0.91–0.99 |
| Individual level | ||||||
| Personal history of overdose | 384 (26.89) | 118 (30.73) | 266 (25.48) | 0.044 | 1.30 | 1.00–1.68 |
1P values are generated with generalized estimating equations which cluster on the ego
2Immediate family includes the following: father, mother, daughter/son, sister/brother, step-mother/step-father, and husband/wife
3N = 1382
4Because 182 lived in the same building, their distance was 0 and the Log(0) is undefined. We therefore took the log of 0.00189394 miles, or the equivalent of 10 ft
To further explore the dyadic finding that relationships to others who had previously overdosed were more spatially proximal (i.e., individuals in the relationship resided closer to one another) than relationships to others who had not previously overdosed, we sought to determine if this could be due to the increased population density in the central area of this small town, which is characterized both by more overdoses and more people. As seen in Table 2, those living closer to the town center were more likely to have at least one network member who had previously overdosed. For example, those with relationships to others with a history of overdose lived a median of 2.5 miles from the town center, while those without network members with a history of overdose lived a median of 5.5 miles outside of the town center. Further, those who had previously overdosed lived closer to the town center than those who had not previously overdosed (median distance 2.42 miles vs. 3.84 miles; mean distance 4.48 miles vs. 6.15 miles, respectively; p = 0.01). Both the proportion and the number of network members who previously overdosed increased significantly as the distance to the center of town decreased (p values = 0.012 and 0.002, respectively). As those living closer to the town center were more likely to have previously overdosed and had more network members (as measured by both the number and proportion) who had previously overdosed, this additional analysis similarly suggests that the findings from our dyadic analysis may be partially explained by the increased population density and overdose prevalence near the town center.
Table 2.
Individual and network correlates of having at least one network member with a history of an overdose, N = 463
| ALL (N = 463) | Had at least one first-degree network member who has ever overdosed (N = 265) | Did not have any first-degree network members who have ever overdosed (N = 198) | P value | |
|---|---|---|---|---|
| Network measures | ||||
| In-degree, median (IQR) | 1 (1–3) | 2 (1–3) | 1 (1–2) | < .0001 |
| Out-degree, median (IQR) | 2 (1–3) | 2 (1–3) | 1 (1–2) | < .0001 |
| Betweenness centrality, median (IQR) | 9 (0–194.5) | 50 (0–310) | 0 (0–48) | 0.0001 |
| Spatial measures | ||||
| Miles to town center, median (IQR) | 3.54 (0.65–7.58)1 | 2.50 (0.53–6.14)2 | 5.53 (1.94–8.89)3 | 0.0039 |
| Log (miles to town center), median (IQR) | 1.26 (−0.43–2.03)1 | 0.92 (−0.62–1.82)2 | 1.71 (0.66–2.18)3 | < .0001 |
| Individual-level demographic characteristics | ||||
| Age, median (IQR) | 31 (26–38) | 31 (26–38) | 31 (25–37) | 0.2072 |
| Years living in Eastern Kentucky, median (IQR) | 29 (23–35) | 29 (23–34) | 28 (22–35) | 0.5672 |
| Months of education completed, median (IQR) | 144 (120–144) | 144 (120–144) | 144 (130–144) | 0.0062 |
| Amount of money received from employment (net income) in past 30 days, median (IQR) | 0 (0–400) | 0 (0–400) | 0 (0–300) | 0.180 |
| Race/ethnicity | 0.238 | |||
| Non-Hispanic White, n (%) | 435 (93.95) | 248 (93.58) | 187 (94.44) | |
| Non-Hispanic Black, n (%) | 18 (3.89) | 13 (4.91) | 5 (2.53) | |
| Other, n (%) | 10 (2.16) | 4 (1.51) | 6 (3.03) | |
| Male, n (%) | 260 (56.16) | 157 (59.25) | 103 (52.02) | 0.121 |
| Transportation access, n (%) | 167 (36.07) | 73 (27.55) | 94 (47.47) | < .0001 |
| Individual-level risk behaviors | ||||
| Ever overdosed, n (%) | 131 (28.29) | 79 (29.81) | 52 (26.26) | 0.402 |
| Any opiate use (past 6 months), n (%) | 462 (99.78) | 265 (100) | 197 (99.49) | 0.247 |
| Ever enrolled in drug treatment, n (%) | 258 (55.72) | 148 (55.85) | 110 (55.56) | 0.950 |
| Ever enrolled in drug detox, n (%) | 164 (35.42) | 102 (38.49) | 62 (31.31) | 0.110 |
| Ever enrolled in alcohol detox, n (%) | 40 (8.64) | 32 (12.08) | 8 (4.04) | 0.002 |
| Ever arrested, n (%) | 405 (87.47) | 240 (90.57) | 165 (83.33) | 0.020 |
1N = 452
2N = 217
3N = 235
With respect to individual-level network measures, those with higher out-degrees (i.e., more reported relationships to others in the sample), in-degrees (i.e., more other individuals reporting relationships to him/her), and betweenness centralities (i.e., on the shortest path between more pairs of individuals in the confirmed network) were more likely to have at least one network member who had previously overdosed. At the individual level, correlates of having at least one network member with an overdose history included (a) residing closer to the town center, (b) fewer years of education, (c) decreased transportation access, (d) prior enrollment in an alcohol detox program, and (e) a prior arrest.
As seen in Table 2, the median out-degree and in-degree in the sample were 2 and 1, respectively. As seen in Table 3, (1) the odds of having at least one network member who previously overdosed increased for each unit increase in out-degree (OR = 1.46; 95%CI 1.25–1.72), in-degree (OR = 1.61; 95%CI 1.38–1.87), and betweenness centrality (OR = 1.00; 95%CI 1.00–1.00); and (2) the risk associated with each additional network member with a history of overdose increased with increasing out-degree (RR = 1.26; 95%CI 1.19–1.33), in-degree (RR = 1.25; 95%CI 1.20–1.31), and betweenness centrality (RR = 1.00; 95%CI 1.00–1.00).
Table 3.
Individual, network, and spatial correlates of (a) having at least one first-degree network member with a history of an overdose and (b) each additional first-degree network member with a history of overdose, N = 463
| Had at least one first-degree network member who previously overdosed vs. had no first-degree members who have ever overdosed | Each additional first-degree network member with a history of overdose | |||
|---|---|---|---|---|
| OR | 95%CI | RR | 95%CI | |
| Individual-level demographics | ||||
| Age | 1.01 | 0.99–1.04 | 1.01 | 1.00–1.02 |
| Years living in Eastern Kentucky | 1.00 | 0.99–1.02 | 1.00 | 1.00–1.01 |
| Months of education completed | 0.99 | 0.98–1.00 | 1.00 | 0.99–1.00 |
| Amount of money received from employment (net income) in the past 30 days | 1.00 | 1.00–1.00 | 1.00 | 1.00–1.00 |
| Male | 1.34 | 0.93–1.94 | 1.16 | 0.99–1.38 |
| Transportation access | 0.42 | 0.29–0.62 | 0.71 | 0.60–0.84 |
| Individual-level risk behaviors | ||||
| Ever overdosed | 1.19 | 0.79–1.80 | 1.10 | 0.92–1.33 |
| Ever enrolled in drug treatment | 1.01 | 0.70–1.47 | 1.07 | 0.91–1.27 |
| Ever enrolled in drug detox | 1.37 | 0.93–2.03 | 1.27 | 1.07–1.50 |
| Ever enrolled in alcohol detox | 3.26 | 1.47–7.25 | 1.82 | 1.36–2.43 |
| Ever arrested | 1.92 | 1.10–3.35 | 1.22 | 0.95–1.57 |
| Network measures | ||||
| In-degree | 1.61 | 1.38–1.87 | 1.25 | 1.20–1.31 |
| Out-degree | 1.46 | 1.25–1.72 | 1.26 | 1.19–1.33 |
| Betweenness centrality | 1.00 | 1.00–1.00 | 1.00 | 1.00–1.00 |
| Spatial measures | ||||
| Log (miles to town center) | 0.75 | 0.66–0.86 | 0.89 | 0.85–0.94 |
Higher centrality scores (in-degree, out-degree, and betweenness), living closer to the town center, decreased transportation access, fewer years of education, and prior enrollment in an alcohol detox program were significantly associated with both the binary and continuous outcomes, prior to adjustment. A history of arrest was only associated with the binary outcome in the unadjusted models and prior enrollment in a drug detox program was only associated with the continuous outcome, prior to adjustment.
Table 4 presents the adjusted associations. After adjustment, correlates of having at least one network member with an overdose history included (a) higher out-degree, (b) higher in-degree, (c) living closer to the town center, and (d) decreased transportation access. After adjustment, correlates of having additional network members who have previously overdosed included (a) higher out-degree, (b) higher in-degree, (c) living closer to the town center, (d) decreased transportation access, and (e) prior enrollment in an alcohol detox program.
Table 4.
Multivariable models assessing individual, network, and spatial correlates of (1) having at least one first-degree network member with a prior overdose and (2) each additional first-degree network member with a prior overdose (N = 452)1
| Had at least one first-degree network member who has ever overdosed vs. had no first-degree alters who have ever overdosed | Each additional first-degree network member with a history of overdose | |||
|---|---|---|---|---|
| AOR | 95% CI | ARR | 95% CI | |
| Out-degree | 1.36 | 1.14–1.63 | 1.18 | 1.15–1.25 |
| In-degree | 1.54 | 1.31–1.80 | 1.20 | 1.15–1.25 |
| Log (miles to town center) | 0.80 | 0.69–0.92 | 0.94 | 0.89–0.98 |
| Transportation access | 0.47 | 0.30–0.72 | 0.81 | 0.69–0.93 |
| Ever enrolled in an alcohol detox program | – | – | 1.51 | 1.17–1.94 |
1The sample size for the final models was reduced from 463 to 452 because spatial information was only available for 452 of the 463 study participants
Discussion
Using a variety of social network-based approaches, we sought to identify correlates of being in close social proximity to someone who self-reported at least one prior overdose in their lifetime. In this analysis, social proximity was defined as a relationship between two individuals in the sample which was reported by one or both members of the dyad. Regardless of whether or not the prior overdose was witnessed by the network member (i.e., overdoses are self-reported and could have occurred at any point in their lifetime), the person remains at increased risk for witnessing an overdose in the future, given that most individuals in the sample who reported a prior overdose reported multiple prior overdoses, and may therefore be more likely to also experience an overdose in the future.
Even though only slightly more than a quarter of the sample had previously overdosed, more than half had a first-degree relationship with someone who had previously overdosed. Further, those who had at least one relationship with someone who had previously overdosed had on average 1.45 relationships with others who had previously overdosed (median = 1; IQR 1–2). Consequently, targeting overdose prevention interventions at individuals who have more contacts with a history of overdose may optimize overdose prevention efforts and reduce future fatalities.
At the relationship level, our analyses show that relationships to others who have overdosed previously were more spatially proximal relationships (i.e., those who resided closer to one another). This finding may be partially explained by the findings from our individual-level analyses, which show that those living closer to the town center were more likely to (1) have personally overdosed in the past and (2) have relationships with others who had previously overdosed.
Our analyses also identified individual, network, and spatial correlates of having at least one relationship to someone with an overdose history and correlates of having additional relationships to those with an overdose history. Based on the adjusted model, those occupying more central network positions (in-degree and out-degree), who reside closer to the town center, and who had decreased transportation access were more likely to have at least one relationship to someone who previously overdosed. The same factors were associated with each additional relationship to a person with an overdose history, but with one addition. While prior enrollment in an alcohol detox program did not remain in the final model for the binary outcome (i.e., at least one network member who had overdosed in the past), it retained its statistical significance in the model for the continuous outcome (i.e., number of network members who have previously overdosed). While prior enrollment in an alcohol detox program was positively associated with both outcomes, it only retained statistical significance in the final model for the continuous version of the outcome. Thus, compared to those who had not previously enrolled in an alcohol detox program, those who had previously enrolled in an alcohol detox program had significantly more first-degree network members with an overdose history, on average. This suggests that providing overdose prevention training and naloxone access to those enrolled in alcohol detoxification programs may equip those at increased risk for witnessing an overdose in the future with the tools and training to intervene. We also found that those living closer to the town center were more likely to be in relationships with others who had previously overdosed, which suggests that overdose prevention efforts (i.e., naloxone distribution, overdose prevention trainings) should target those residing within 5 miles of the town center.
Limitations
One of the limitations of this analysis is that the sociometric network analysis was restricted to include only those individuals who named or were named by at least one other person in the sample. Thus, it is possible that some of the individuals removed from our sample due to the absence of reported and confirmed relationships with other SNAP participants may have been connected to others in the study population or even in the study sample, but these connections were not reported. Our analytic approach also assumed that a relationship between two individuals existed if at least one of the two members of the pair named the other as a network member. This is a reasonable assumption, as our name-generating questions elicited the names of sex partners, drug partners, and those who provided some form of social support. For these types of relationships, the acknowledgement of a relationship between person A and person B but not between person B and person A most likely means that a relationship exists that was only reported by one member of the pair. For example, if person A lists person B as someone with whom he/she uses drugs and person B does not similarly list person A, it is more likely that person B forgot to mention or intentionally omitted person A than it is that the two are not connected. Forgetting ties is frequently discussed in the literature [36–38] and our approach is consistent with the approach used in other published research on risk networks [26, 28].
For the dyadic analysis, we also assumed that the relationship characteristics reported by A about B could be applied to the relationship between B and A when B did not list A as a network member. This assumption is likely to be valid for the following relationship characteristics: co-usage of drugs, sex partner, sex partner and co-usage of drugs, familial tie, immediate family member, and relationship duration. However, the direction in which support is provided and the perceived trust in the relationship may differ from each person’s perspective. To determine the sensitivity of our dyadic analysis to this assumption, we re-ran the analysis with relationship information for only the 897 relationships where the ego reported knowing the alter. In this restricted analysis, the direction of the relationships and effect sizes for all variables examined were consistent with those presented in Table 1. There was only one minor deviation with respect to statistical significance, which may have resulted from the reduced sample size and diminished statistical power: the trust variable was statistically significant in the unadjusted but not the adjusted analysis presented in Table 1 but was not statistically significant in the restricted analysis (p = 0.110). The final models with and without this assumption included the same variables and the effect sizes were almost identical across the two models.
Conclusion
Findings from this study suggest novel strategies for expanding coverage of overdose prevention trainings and naloxone distribution in rural Eastern Kentucky through network-based approaches (i.e., individuals who report knowing more people), spatially targeted approaches (i.e., those living closer to the town center), and to those enrolled in alcohol detoxification programs. Through these combined strategies, we may be able to better equip those at the highest risk of witnessing an overdose with the resources and education to intervene and reduce the fatality rate among future overdoses in this region. Of note, because our analysis focused on individuals who were socially connected to others in the sample, our conclusions are most applicable to people who use drugs with others. Different strategies may be needed to effectively reach those who use drugs alone or who are more socially isolated.
Acknowledgements
Funding was provided by the National Institute of Health grant numbers R01 DA024598 & R01 DA033862 (PI: Havens, JR), K01 DA033879 (PI: Rudolph, AE), and R21 AI131979 (PI: Rudolph, AE).
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Injury Prevention & Control: Data & Statistics (WISQARSTM) 2014 (Available at: http://www.cdc.gov/injury/images/lc-charts/leading_causes_of_injury_deaths_unintentional_injury_2014_1040w740h.gif). Accessed March 7, 2016. http://www.cdc.gov/injury/images/lc-charts/leading_causes_of_injury_deaths_unintentional_injury_2014_1040w740h.gif.
- 2.Centers for Disease Control and Prevention. Drug overdose deaths in the United States, 1999-2016. National Center for Health Statistics 2017. Available at::https://www.cdc.gov/nchs/products/databriefs/db294.htm. Accessed 21 Dec 2017.
- 3.Centers for Disease Control and Prevention. CDC reports rising rates of drug overdose deaths in rural areas. CDC 24/7: Saving Lives, Protecting People 2017. Available at: https://www.cdc.gov/media/releases/2017/p1019-rural-overdose-deaths.html. Accessed 19 Oct 2018.
- 4.Martins SS, Sampson L, Cerdá M, Galea S. Worldwide prevalence and trends in unintentional drug overdose: a systematic review of the literature. Am J Public Health. 2015;105(11):e29–e49. doi: 10.2105/AJPH.2015.302843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warner M, Chen LH, Makuc DM. Increase in fatal poisonings involving opioid analgesics in the United States, 1999-2006. NCHS Data Brief. 2009;(22):1–8. [PubMed]
- 6.Paulozzi LJ, Xi Y. Recent changes in drug poisoning mortality in the United States by urban-rural status and by drug type. Pharmacoepidemiol Drug Saf. 2008;17(10):997–1005. doi: 10.1002/pds.1626. [DOI] [PubMed] [Google Scholar]
- 7.Havens JR, Oser CB, Leukefeld CG, Webster JM, Martin SS, O’Connell DJ, Surratt HL, Inciardi JA. Differences in prevalence of prescription opiate misuse among rural and urban probationers. Am J Drug Alcohol Abuse. 2007;33(2):309–317. doi: 10.1080/00952990601175078. [DOI] [PubMed] [Google Scholar]
- 8.Wunsch MJ, Nakamoto K, Behonick G, Massello W. Opioid deaths in rural Virginia: a description of the high prevalence of accidental fatalities involving prescribed medications. Am J Addict. 2009;18(1):5–14. doi: 10.1080/10550490802544938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Drug overdose mortality by state: 2016. 2016.
- 10.Centers for Disease Control and Prevention Drug Overdose Death Data. 2017; https://www.cdc.gov/drugoverdose/data/statedeaths.html. Accessed 7 Oct 2018.
- 11.Tilley JC, Ingram V. 2017 Overdose fatality report. 2017. Available at: https://odcp.ky.gov/Documents/2017%20Kentucky%20Overdose%20Fatality%20Report%20%28final1%29.pdf. 19 Oct 2018.
- 12.Keyes KM, Cerda M, Brady JE, Havens JR, Galea S. Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health. 2014;104(2):e52–e59. doi: 10.2105/AJPH.2013.301709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wininger PJ. Pharmaceutical overpromotion liability: the legal battle over rural prescription drug abuse. Ky LJ. 2004;93:269. [Google Scholar]
- 14.Havens JR, Talbert JC, Robert W, Cynthia L, Leukefeld CG. Trends in controlled-release oxycodone (OxyContin®) prescribing among Medicaid recipients in Kentucky, 1998-2002. J Rural Health. 2006;22(3):276–278. doi: 10.1111/j.1748-0361.2006.00046.x. [DOI] [PubMed] [Google Scholar]
- 15.McDonald DC, Carlson K, Izrael D. Geographic variation in opioid prescribing in the US. J Pain. 2012;13(10):988–996. doi: 10.1016/j.jpain.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang KH, Fiellin DA, Becker WC. Source of prescription drugs used nonmedically in rural and urban populations. Am J Drug Alcohol Abuse. 2014;40(4):292–303. doi: 10.3109/00952990.2014.907301. [DOI] [PubMed] [Google Scholar]
- 17.Sporer KA. Acute heroin overdose. Ann Intern Med. 1999;130(7):584–590. doi: 10.7326/0003-4819-130-7-199904060-00019. [DOI] [PubMed] [Google Scholar]
- 18.Tracy M, Piper TM, Ompad D, Bucciarelli A, Coffin PO, Vlahov D, Galea S. Circumstances of witnessed drug overdose in New York City: implications for intervention. Drug Alcohol Depend. 2005;79(2):181–190. doi: 10.1016/j.drugalcdep.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 19.Dietze P, Cantwell K, Burgess S. Bystander resuscitation attempts at heroin overdose: does it improve outcomes? Drug Alcohol Depend. 2002;67(2):213–218. doi: 10.1016/S0376-8716(02)00063-7. [DOI] [PubMed] [Google Scholar]
- 20.Rowe C, Santos G-M, Vittinghoff E, Wheeler E, Davidson P, Coffin PO. Neighborhood-level and spatial characteristics associated with lay naloxone reversal events and opioid overdose deaths. J Urban Health. 2016;93(1):117–130. doi: 10.1007/s11524-015-0023-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rossen LM, Khan D, Warner M. Hot spots in mortality from drug poisoning in the United States, 2007–2009. Health Place. 2014;26:14–20. doi: 10.1016/j.healthplace.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Klimas J, O’reilly M, Egan M, Tobin H, Bury G. Urban overdose hotspots: a 12-month prospective study in Dublin ambulance services. Am J Emerg Med. 2014;32(10):1168–1173. doi: 10.1016/j.ajem.2014.07.017. [DOI] [PubMed] [Google Scholar]
- 23.Latkin CA, Hua W, Tobin K. Social network correlates of self-reported non-fatal overdose. Drug Alcohol Depend. 2004;73(1):61–67. doi: 10.1016/j.drugalcdep.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 24.Young AM, Jonas AB, Mullins UL, Halgin DS, Havens JR. Network structure and the risk for HIV transmission among rural drug users. AIDS Behav. 2012;17(7):2341–2351. doi: 10.1007/s10461-012-0371-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Young AM, Rudolph AE, Quillen D, Havens JR. Spatial, temporal and relational patterns in respondent-driven sampling: evidence from a social network study of rural drug users. J Epidemiol Community Health. 2014;68(8):792–798. doi: 10.1136/jech-2014-203935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rudolph AE, Young AM, Havens JR. Examining the social context of injection drug use: social proximity to persons who inject drugs versus geographic proximity to persons who inject drugs. Am J Epidemiol. 2017;186(8):970–978. doi: 10.1093/aje/kwx162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Young AM, Rudolph AE, Havens JR. Network-based research on rural opioid use: an overview of methods and lessons learned. Curr HIV/AIDS Rep. 2018:1–7. [DOI] [PMC free article] [PubMed]
- 28.Young AM, Rudolph AE, Su AE, King L, Jent S, Havens JR. Accuracy of name and age data provided about network members in a social network study of people who use drugs: implications for constructing sociometric networks. Ann Epidemiol. 2016;26(11):802–809. doi: 10.1016/j.annepidem.2016.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Environmental Systems Research Institute (ESRI). North America detailed streets. 2007; http://www.arcgis.com/home/item.html?id=f38b87cc295541fb88513d1ed7cec9fd. Accessed September 1, 2013.
- 30.Borgatti SP, Everett MG, Freeman LC. Ucinet for Windows: software for social network analysis. 2002.
- 31.Keeling MJ, Eames KT. Networks and epidemic models. J R Soc Interface. 2005;2(4):295–307. doi: 10.1098/rsif.2005.0051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stata Statistical Software: Release 14 [computer program]. College Station, TX StataCorp LP.; 2015.
- 33.Stephens DB, Havens JR. Predictors of alcohol use among rural drug users after disclosure of hepatitis C virus status. J Stud Alcohol Drugs. 2013;74(3):386–395. doi: 10.15288/jsad.2013.74.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jonas AB, Young AM, Oser CB, Leukefeld CG, Havens JR. OxyContin® as currency: OxyContin® use and increased social capital among rural Appalachian drug users. Soc Sci Med. 2012;74(10):1602–1609. doi: 10.1016/j.socscimed.2011.12.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Havens JR, Oser CB, Knudsen HK, Lofwall M, Stoops WW, Walsh SL, Leukefeld CG, Kral AH. Individual and network factors associated with non-fatal overdose among rural Appalachian drug users. Drug Alcohol Depend. 2011;115(1):107–112. doi: 10.1016/j.drugalcdep.2010.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brewer DD. Forgetting in the recall-based elicitation of personal and social networks. Soc Networks. 2000;22(1):29–43. doi: 10.1016/S0378-8733(99)00017-9. [DOI] [Google Scholar]
- 37.Brewer DD, Webster CM. Forgetting of friends and its effects on measuring friendship networks. Soc Networks. 2000;21(4):361–373. doi: 10.1016/S0378-8733(99)00018-0. [DOI] [Google Scholar]
- 38.Marin A. Are respondents more likely to list alters with certain characteristics?: implications for name generator data. Soc Networks. 2004;26(4):289–307. doi: 10.1016/j.socnet.2004.06.001. [DOI] [Google Scholar]