Abstract
Iron deficiency (ID) is a common and ominous comorbidity in heart failure (HF) and predicts worse outcomes, independently of the presence of anaemia. Accumulated data from animal models of systemic ID suggest that ID is associated with several functional and structural abnormalities of the heart. However, the exact role of myocardial iron deficiency irrespective of systemic ID and/or anaemia has been elusive. Recently, several transgenic models of cardiac-specific ID have been developed to investigate the influence of ID on cardiac tissue. In this review, we discuss structural and functional cardiac consequences of ID in these models and summarize data from clinical studies. Moreover, the beneficial effects of intravenous iron supplementation are specified.
Keywords: Iron deficiency, Myocardial iron deficiency, Heart failure, Iron supplementation
Introduction
Iron is one of the most important microelements in the body as it is involved in diverse metabolic processes, including transport of oxygen, synthesis of deoxyribonucleic acid (DNA) and oxidative energy production within the electron transport chain (ETC) [1]. With regard to its redox-based properties, iron is an integral part of Fe-S metalloproteins—key players in cellular energetics, which can be found in the nucleus, cytosol and mitochondria [2]. The optimal iron supply is critical particularly for the proper functioning of high-energy demand cells, specifically cardiomyocytes and skeletal myocytes [3, 4]. It is well established that either iron overload or ID unfavourably affect human condition and in particular, the role of disordered iron homeostasis in heart failure (HF) has been elucidated in several papers [5–9]. This review will focus on structural and functional abnormalities occurring in the heart as consequences of systemic or cardiac-specific ID with the strong emphasis on molecular evidence.
Systemic iron deficiency and its consequences for heart
ID is one of the most common nutrition deficiencies worldwide [10] and untreated may lead to ID related anaemia (IDA). The effects of systemic ID on cardiac function have been evaluated in several animal studies. Acute and chronic models of systemic ID have been developed in animals by bleeding or by feeding a low-iron diet, respectively [11–17]. The results have shown that ID with concomitant anaemia resulted in cardiomegaly, left ventricular (LV) hypertrophy, cardiac fibrosis and symptomatic HF [9, 14, 18, 19], leading in severe cases to hypervolemia and pulmonary congestion [14, 20, 21].
In animal models, dietary iron restriction causes a significant decrease of total heart iron [22] and numerous structural and ultrastructural aberrations in heart, specifically cardiomyocyte enlargement, degeneration of myofilaments, irregular sarcomere organization and mitochondrial swelling, with the latter two being accompanied by elevated expression of endothelial and inducible nitric oxygen synthase (eNOS and iNOS, respectively) and several stress-related protein molecules [16, 23]. Interestingly, the oxidative/nitrosative stress which is associated with elevated generation of reactive oxygen species (ROS) and/or reactive nitrogen species (RNS) is increasingly being recognized as one of the pathophysiological mechanisms of LV remodelling responsible for HF progression [24]. Additionally, Dong et al. have shown that ID in rats upregulated an expression of apoptosis-promoting protein caveolin-1 in myocardium and also triggered mitochondrial-to-cytosolic translocation of cytochrome c, which constitutes both an indicator of mitochondrial damage and the major pre-apoptotic mitochondrial phenomenon [23, 25, 26]. Further, in myocardium, ID also contributes to the impaired mitochondrial oxidative energy production within ETC, as the activities of the respiratory chain enzymes such as Complexes I-II and IV, succinic cytochrome c reductase (SCCR) and NADH ferricyanide oxidoreductase are reduced as well as mitochondrial oxygen uptake is lower [27]. Importantly, there is a study reporting that intravenous (i.v.) iron sucrose treatment of dietary iron-restricted mice reversed LV remodelling and prevented cardiac fibrosis, despite the fact that it did not fully correct IDA. Furthermore, i.v. iron reduced nitrosative and oxidative stress and attenuated inflammation in the heart [13].
Cardiac-specific iron deficiency
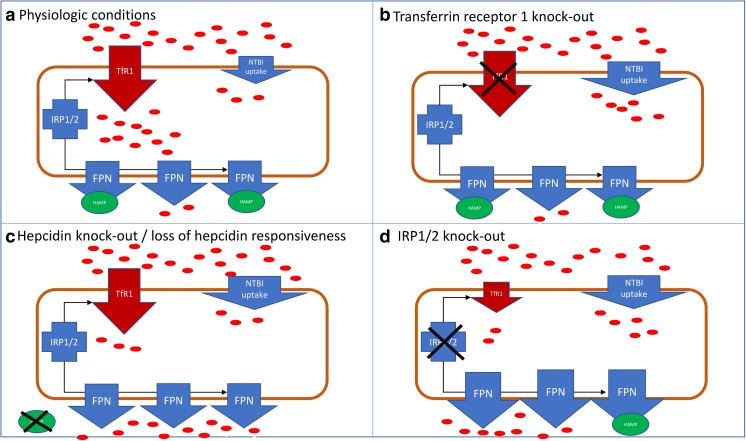
Although the dietary iron restriction studies provided evidence on abnormalities in the heart muscle induced by systemic ID, it was extremely difficult to define the actual functional implications of myocardial iron deficiency (MID) independent of systemic ID and/or anaemia. Currently, there is a considerable interest in developing animal models of cardiac-specific ID in the absence of anaemia in order to circumvent the ambiguity in interpretation. In this paragraph, we discuss different approaches applied to induce cardiac-specific ID and present recent findings in this field (Fig. 1).
Fig. 1.
Molecular elements of intracellular iron metabolism in cardiomyocytes in different transgenic models of cardiac specific ID. a Physiologic conditions, b TfR1 knock-out, c Hepcidin knock out/loss of hepcidin responsiveness, d IRP 1/2 knock-out.  iron; TfR1–transferrin receptor 1; IRP1/2–iron regulatory proteins 1 and 2; FPN–ferroportin; HAMP–hepcidin; NTBI–non-transferrin-bound iron
iron; TfR1–transferrin receptor 1; IRP1/2–iron regulatory proteins 1 and 2; FPN–ferroportin; HAMP–hepcidin; NTBI–non-transferrin-bound iron
Cardiomyocyte-specific Tfr1 knock-out
Ubiquitously expressed transferrin receptor 1 (Tfr1) is a membrane glycoprotein that serves as a gatekeeper in regulating cellular uptake of iron from transferrin [28, 29]. Total Tfr1 knockout embryos were abnormal and died before embryonic day 12.5 with oedema and diffuse necrosis in all tissues consistent with anaemia and hypoxia. However, they presented no anatomical defects in the embryonic heart, suggesting that cardiac structures did not require Tfr1 to development [30].
To determine the importance of TfR1 in the heart, Xu et al. disrupted Tfr1 using a heart-specific promoter [31]. Tissue non-haemic and total iron concentration in Tfr1hrt/hrt hearts was decreased at birth and did not change substantially during the post-natal period. Mice died by post-natal day 11 with cardiac hypertrophy and cardiomegaly. Tfr1hrt/hrt hearts showed left ventricular dilatation, decreased fractional shortening, enlarged cardiomyocytes and significantly increased cardiac hypertrophy biomarkers, indicating that cardiomyocyte-specific TfR1 knockout leads to the phenotype of dilated cardiomyopathy. Fe-S cluster biogenesis, estimated by decreased expression of Dpyd and Ppat proteins [32], was compromised due to ID or mitochondrial dysfunction. Mitochondria from Tfr1hrt/hrt hearts were also severely disrupted and enlarged, and expression and activity of ETC mitochondrial complexes (I-IV, where iron is necessary [33]) were significantly decreased. Notably, non-iron-containing Complex V expression and activity remained unchanged. Moreover, mitochondria-encoded mRNA levels were decreased, indicating fewer mitochondria or mitochondria unable to normal gene expression. mRNA expression profile also showed downregulation of genes associated with peroxisome proliferator-activated receptor signalling (PRAR) and PGC1-a (stimulator of mitochondrial biogenesis), myogenesis and insulin signalling as well as upregulation of hypoxia-inducible targets, Myc targets and glycolytic enzymes. Tfr1hrt/hrt hearts also showed metabolic changes, increased apoptosis in addition to impaired mitophagy.
The survival of Tfr1hrt/hrt mice has been prolonged by cardiac iron repletion via intravenous (i.v.) treatment with iron dextran, but mice still died at 4–5 weeks with severe cardiomegaly. However, iron-supplemented Tfr1hrt/hrt mice assimilated and used given iron which was reflected by the fact that at day 10, Fe-S proteins (Dpyd and Ppat) as well as ETC proteins were at the similar level compared to WT mice. Moreover, heart-to-body weight ratios in iron-treated Tfr1hrt/hrt mice after 10 days were similar to WT littermates. Notably, the administration of a second dose of dextran delayed the pathological changes and consequent death up to 13 weeks.
Cardiomyocyte-specific HAMP knockout and FPN resistant to HAMP knock-in
Systemic iron homeostasis is regulated by the hepcidin-ferroportin interactions at the sites of iron release into the circulation. At this moment, ferroportin (FPN), also termed as Slc40a1, MTP1 or Ireg1, is the only known mammalian efflux channel for iron, which is localized on the surface of hepatocytes, enterocytes and macrophages—the cells responsible for iron storage, absorption and recycling, respectively [34]. The rate of FPN-mediated iron release depends on the plasma level of iron regulatory hormone hepcidin (HAMP, hepcidin antimicrobial peptide), which is known to inhibit FPN as a part of a homeostatic negative feedback loop [35]. Generated predominantly in liver, hepcidin binds FPN and triggers its endocytosis and subsequent degradation, which results in limited iron efflux into circulation and its lower availability to peripheral tissues [36]. Surprisingly, hepcidin is also expressed in other tissues, such as heart [37], kidney [38], brain [39] and placenta [40]. The exact role of this locally produced hepcidin is still unclear; however, there is some evidence that it may be associated with tissue-specific iron regulation [4, 41].
Lakhal-Littleton et al. have recently discovered expression of FPN in cardiomyocytes, where it was necessary for maintenance of iron homeostasis. Furthermore, the cardiomyocyte-specific deletion of FPN resulted in fatal cardiac iron overload in mice [42]. Given that, they further speculated that cardiac FPN may be under the control of cardiac HAMP and that their interaction may be essential for regulation of local iron homeostasis and proper cardiac function. Having first demonstrated that HAMP is expressed in cardiomyocytes, two novel mouse models were next generated: the one carrying a cardiomyocyte-specific deletion of the Hamp gene (Hampfl/fl;Myh6.Cre+ genotype) [43] and the other with a cardiomyocyte-specific knock-in of Slc40a1 C326Y gene (Slc40a1 C326Yfl/fl;Myh6.Cre+ genotype), which encoded FPN completely resistant to hepcidin inhibition but with preserved iron export function [44, 45].
The results showed that in Hampfl/fl;Myh6.Cre+ mice, the cardiac Hamp mRNA and HAMP protein were almost undetectable, while the liver levels of mRNA and HAMP protein as well as liver iron stores and circulating markers of iron homeostasis remained intact. This is the first evidence that cardiomyocytes are the essential site of hepcidin expression in the heart and that systemic iron homeostasis is not influenced by cardiac hepcidin depletion. Moreover, the hearts of both Hampfl/fl;Myh6.Cre+ and Slc40a1 C326Yfl/fl;Myh6.Cre+ mice developed deadly LV dysfunction characterized by reduced LVEF as well as enlargement of cardiomyocytes in addition to significantly greater mortality when compared to controls. The loss of cardiac HAMP stimulated upregulation of cardiomyocyte FPN in the hearts of both Hampfl/fl;Myh6.Cre+ and Slc40a1 C326Yfl/fl;Myh6.Cre+ mice which in turn resulted in increased iron efflux that finally lead to cardiomyocyte ID. Additional studies revealed the reduced activities of iron-containing metabolic enzymes, signs of mitochondrial failure, significantly greater apoptosis and increased glycolysis in Hampfl/fl;Myh6.Cre+ hearts.
However, the most striking discovery was that all morphological abnormalities and metabolic and contractile dysfunctions were entirely suppressed by intravenous iron treatment [43].
Cardiomyocyte-specific Irp1 and Irp2 knock-out
Maintenance of intracellular iron content is secured by two cytoplasmic iron-regulatory proteins 1 and 2 (IRP1 and IRP2, also known as ACO1 and IREB2) [46]. Cellular ID stimulates binding of IRPs to cis-regulatory iron-responsive elements (IREs) in the 5′ or 3′ untranslated regions of target mRNAs encoding proteins responsible for iron import (transferrin receptor, TfR1; divalent metal transporter 1, DMT1), sequestration (ferritin H- and L-chains; FTH1, FTL, respectively) and export (ferroportin) [47]. IRPs interact with 5′ IRES in ferroportin and ferritin mRNAs to inhibit their translation and with 3′ IREs in TfR1 to increase its stability and to protect from degradation [48]. In that manner, IRPs promote iron efflux and increase its availability for production of haem- and iron-sulphur proteins in cytosol or mitochondria [47]. Conversely, when intracellular iron is in excess, IRP1 loses ability to bind IREs, and instead binds an iron-sulphur cluster to start functioning as an aconitase enzyme, while IRP2 is targeted for proteasomal degradation [49]. IRP activity is significantly reduced in LV tissue in patients with advanced HF and LV tissue ID [50].
Functional implications of ID in the heart independently of systemic ID and anaemia were recently investigated by Haddad et al. [50]. In the study, cardiomyocyte-specific deletion of Irp1 and Irp2 (Cre-Irp1/2f/f) in mice resulted in significant reduction of iron concentration in LV and also in isolated cardiomyocytes with no evident change in the phenotype under the baseline conditions. Interestingly, under acute dobutamine hemodynamic stress, Cre-Irp1/2f/f mice exhibited functional abnormalities, in particular inability to increase LV systolic function. After induction of myocardial infarction (MI), Irp-targeted mice presented more pronounced LV hypertrophy, greater increase in cardiomyocyte size and higher expression of embryonic marker genes. Additionally, LV dilatation and systolic dysfunction were more evident than in control mice. Furthermore, Cre-Irp1/2f/f mice exhibited symptoms of ongoing HF failure, such as pulmonary congestion, accumulation of serous fluid in the chest cavity and increased mortality. Considering cardiomyocyte mitochondria, there were no significant differences between IRP-targeted mice and controls. However, the activity of ETC Complex I was significantly decreased, while the activity of complex IV was not affected. The oxygen consumption rate (OCR) in cardiomyocytes was not remarkably different in baseline conditions, showing that ATP production was comparable in both Cre-Irp1/2f/f and control mice. However, upon maximal respiration, OCR increase in IRP1/2-deficient mice was strongly weakened when compared to the control mice. At baseline conditions, glycolytic activity of IRP-targeted mice was not affected; however, in maximal respiration, it increased to a smaller extent compared to control. In vivo cardiac energy metabolism study by 31P-magnetic resonance spectroscopy did not show any differences in PCr/ATP ratio in LV between Cre-Irp1/2f/f and control. Nevertheless, after dobutamine stress, PCr/ATP ratio fell down significantly only in Cre-Irp1/2f/f, indicating limitation of high-energy phosphate deposits in IRP cardiomyocyte-knockout.
Noteworthy, cardiomyocyte single IRP1- or single IRP2-targeted mice did not develop MID and did not exhibit any of aforementioned symptoms.
Intravenous ferric carboxymaltose (FCM) injection restored both iron concentration in IRP-targeted left ventricle and OCR in maximal respiration in Cre-Irp1/2f/f cardiomyocytes as well as restituted systolic function in dobutamine-stimulated Cre-Irp1/2f/f mice. Moreover, i.v. iron treatment additionally prevented from increased hypertrophy after MI. FCM treatment in post-infarct IRP-targeted mice also improved LV systolic function and attenuated LV dilatation.
Iron homeostasis and deficiency in the failing human heart
In patients with HF, the role of ID in pathophysiology is highly pronounced and deeply investigated. Accordingly to the broad definition of ID (serum ferritin < 100 μg/l or serum ferritin 100–300 μg/l in combination with TSAT < 20%), up to 50% of chronic HF patients suffer from ID (57% of anaemic and 32% of non-anaemic) [7, 51]. ID is more prevalent in women sex and in those with advanced NYHA class, higher serum levels of N-terminal pro-type B natriuretic peptide (NT-pro-BNP) and higher serum concentrations of C-reactive protein (CRP) [51]. ID is considered as a predictor of unfavourable outcome and is associated with impaired exercise capacity, independently of the presence of anaemia [6–8, 51]. In acute HF, where ID is also highly prevalent [52], ID was found as a predictor of increased mortality in both anaemic and non-anaemic patients [5, 53].
Recently, Melenovsky et al. performed a direct tissue analysis of myocardial iron content and mitochondrial function in HF [54]. As it has been showed before [18, 55], iron content in LV tissue was significantly decreased in failing human hearts compared to HF-free organ donors, independently of anaemia [54]. MID was associated with more pronounced coronary disease and lower beta-blocker usage compared with non-MID HF patients. Except that, MID in HF was accompanied by reduced activity of aconitase and citrate synthase as well as reduced expression of reactive oxygen species (ROS)-protective enzymes (catalase, glutathione peroxidase and superoxide dismutase 2), indicating that MID may contribute to worsening of mitochondrial dysfunction that exists in HF [54]. These findings are consistent with the recent research from Hoes et al., who demonstrated reduced energy production and contractile dysfunction in iron-deficient human cardiomyocytes [56]. Cells treated with iron chelator deferoxamine (DFO) exhibited reduced activity of iron-sulphur containing mitochondrial complexes (I, II, III) and also displayed significantly lower level of cellular ATP and reduced contractile force. Interestingly, supplementation of transferrin-bound iron reversed all functional and morphological abnormalities. Additionally, our recent research showed that intracellular iron depletion is detrimental for functioning of cardiomyocytes and skeletal myocytes and leads to increased apoptosis and reduces cell viability [57, 58].
It is also worth to notice that MID in human failing heats not only reflects reduced iron availability due to systemic iron deficiency but might also be influenced by a dysregulation of cardiomyocyte iron homeostasis, e.g. downregulation of TfR1 [18] and IRP inactivation [50]. Restoring myocardial iron content may be considered as a strategy to improve substrate utilization and myocardial energetics.
Clinical options to non-invasive detection of MID are strongly limited. Leszek et al. showed that out of all serum markers, only sTfR correlated with the depletion of myocardial iron (r = − 0.44, p = 0.03 for right ventricle and r = − 0.38, p = 0.07 for left ventricle) [55]. However, cardiac T2* magnetic resonance imaging has shown recently a potential utility for evaluating myocardial iron deficiency [59–61].
Beneficial effects of intravenous iron supplementation in human hearts
Clinical research into a treatment of ID and anaemia in HF lead to a conclusion that the administration of erythropoiesis-stimulating agents together with intravenous iron does not yield better clinical outcomes than intravenous iron alone [62]. Further, there is no documented clinical benefit from usage of oral iron preparations [63, 64]. However, two main clinical trials (FAIR-HF and CONFIRM-HF) have proven that intravenous iron supplementation improves quality of life, exercise tolerance and reduces risk of hospitalizations for worsening of HF [65, 66]. Interestingly, the improvement in aforementioned parameters occurred in both anaemic and non-anaemic patients and was equally efficacious [67]. In smaller trials, where HF patients with ID were subjected to i.v. iron supplementation, more beneficial effects have been observed. The favourable changes have been reported in regard to both biochemical parameters such as a reduction in plasma level of NT-proBNP and the echocardiographic measures reflecting myocardial function including an increase in LVEF and attenuation in hypertrophic cardiac remodelling: reduction in LVSD (left ventricular end-systolic dimension), LVDD (left ventricular end-diastolic dimension), LVPW (left ventricular end diastolic posterior wall dimension), IVS (interventricular septal end diastolic dimension thickness), LV mass index, LV end systolic volume and in peak systolic strain rate as well as a decline in E/E0 together with an improvement in S0 and E0 [68–72].
Conclusions
Several animal studies in which ID was induced by low-iron diet or bleeding developed numerous structural and functional cardiac abnormalities. However, because ID and IDA are inseparably related, it was difficult to establish the importance of each of these factors independently.
In this review, we summarized different approaches to induce cardiac-specific ID and discussed most important structural and functional consequences of this state. First of all, transgenic myocardial downregulation of iron import as well as iron export upregulation resulted in intracellular ID. Moreover, in a cardiac-specific TfR1 knock-out, cardiomyocytes were unable to import transferrin-bound iron into cell [31]. Furthermore, both cardiac hepcidin knock-out and loss of hepcidin responsiveness (via cardiac ferroportin knock-in) lead to uncontrolled iron export indicating that cardiac hepcidin controls cardiomyocyte iron homeostasis in an autocrine manner by regulating local ferroportin [43]. Over and above that, IRP1/2-deficient hearts exhibited intracellular ID as a result of simultaneous iron uptake reduction (transferrin receptor downregulation) and an increase in iron export (ferroportin upregulation) [50].
Regarding all transgenic mouse models discussed above, we can observe that most of heart abnormalities induced by systemic ID are also observable in the myocardial-specific ID, independently of anaemia (Table 1). All of these cardiac-specific ID models were characterized by structural aberrations, mitochondrial and metabolic dysfunctions as well as exhibited increased mortality, indicating a strong connection between MID and cardiac dysfunction. Interestingly, the severity of cardiac dysfunction differs in aforementioned animal models. This might be related to the genetic background of the mice, or more importantly to the amount of iron deficiency achieved in the hearts.
Table 1.
Summary of animal models and clinical data investigating consequences of ID on heart structure and functioning
| Animal models | Human Heart Failure | ||||||
|---|---|---|---|---|---|---|---|
| Systemic ID (ID diet) | Cardiomyocyte specific ID | ||||||
| Tfr1 hrt/hrt 31 | Hampfl/fl;Myh6.Cre + or Slc40a1C326Yfl/flMyh6.Cre + 43 | Cre-Irp1/2 f/f 50 | |||||
| Baseline | After MI | ||||||
| Iron concentration in myocardium/cardiomyocytes | ↓22 | ↓ | ↓ | ↓ | ↓ | ↓18, 55, 54 | |
| Anemia | +22, 17, 14, 23, 13 | − | − | − | − | +/−7 | |
| Mortality | ↑ | ↑ | • | ↑ | ↑7 | ||
| Structural changes | Cardiomegaly | +22,17, 23, 13 | + | + | • | ↑ | •54 |
| Cardiac hypertrophy | + 17, 14, 23, 13 | + | + | • | ↑ | •54 | |
| Left ventricle dilatation | + 22,17, 14, 23, 13 | + | + | • | ↑ | •54 | |
| Hypertrophied cardiomyocytes | +14, 23, 13 | + | + | • | ↑ | •54 | |
| Systolic dysfunction | +13 | + | +# | + | •54 | ||
| Mitophagy dysfunction | + | ||||||
| Apoptosis | ↑23 | ↑ | ↑ | ||||
| Mitochondria | Abnormal structure | +23 | + | + | • | ||
| Number | • 23 | ↓ | • | ||||
| Mitochondrial DNA expression | ↓ | • | ↓54 | ||||
| Aberrant mitochondrial respiration | +23 | + | +# | + | +54 | ||
| Electron transport chain | Complex I | ↓27 | ↓ | ↓ | ↓ | •54 | |
| Complex II | ↓27 | ↓ | • | •54 | |||
| Complex III | ↓ | • | •54 | ||||
| Complex IV | ↓27 | ↓ | ↓ | • | •54 | ||
| Aconitase | ↓ | ↓54 | |||||
| Metabolic derangements | Glycolysis | ↑ | ↑ | ↑54 | |||
| Hypoxia inducible genes expression | ↑ 14 | ↑ | |||||
| Recovery by iron supplementation | +13 | + | + | + | +53 | ||
ID iron deficiency, HF heart failure, MID myocardial iron deficiency, empty cells no data, • no differences, # acute dobutamine challenge
Interestingly, benefits of i.v. iron treatment were evident in each of the aforementioned study. Considering one of the most severe phenotype developed by cardiac transferrin receptor 1 knock-out, i.v. iron treatment prolonged the survival of mice up to 13 weeks vs. 9 days without treatment. Additionally, in cardiac hepcidin knock-out, not-binding-hepcidin ferroportin knock-in and IRP1/2 knock-out i.v. iron treatment restored myocardial ID and completely suppressed all morphological changes as well as metabolic and mitochondrial abnormalities, including even these alterations which occurred after myocardial infarction. This in turn may suggest that regardless of decrease in myocardial TfR1 expression, depleted cardiac iron store can be restored throughout i.v. iron treatment via non-transferrin-bound iron (NTBI) uptake. Moreover, continuous iron availability in the Tfr1hrt/hrt knockout mice was accomplished by simultaneous knockout of hemojuvelin, which causes persistent elevation of NTBI (thereby allowing continuous iron uptake via NTBI). This strategy allowed mice to remain healthy until they were sacrificed at 12 months, showing that iron is not only essential to proper cardiac functioning, but also that it must be constantly available. Of note, there are two main potential pathways for NTBI uptake which involve divalent metal transporter 1 (DMT1) [73] and myocardial L-type Ca2+ channel [74] that acts as a compensatory mechanism for TfR1-mediated iron import.
The advantageous effects of iron supplementation have also been reported in clinical studies involving HF patients with ID. According to the recent ESC/HFA 2016 guidelines, all HF patients should be screened for the presence of ID, regardless of the other comorbidities [75]. In symptomatic patients with ID and HFrEF, i.v. iron supplementation should be considered to improve HF symptoms and exercise tolerance as well as quality of life [65, 66] The influence of iron repletion on improvement in morbidity, mortality and outcomes is deeply investigated in the ongoing clinical trials (FAIR-HFpEF; HEART-FID; FAIR-HF2; Affirm-AHF; MYOCARDIAL-IRON).
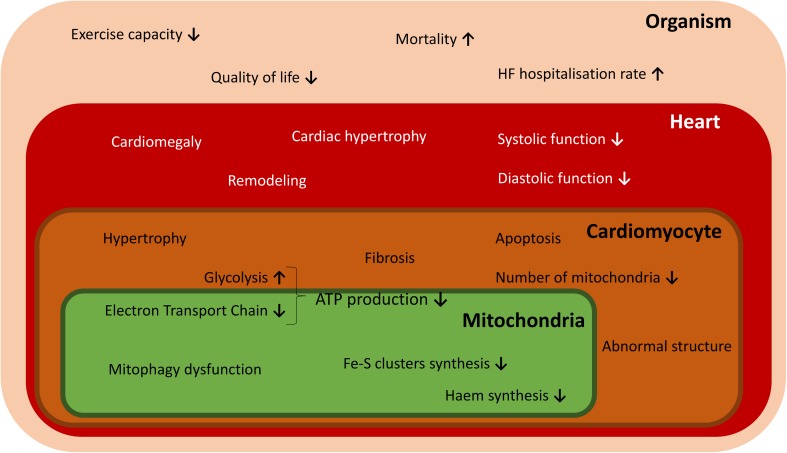
In addition to iron supplementation, other possible therapeutic targets to restore MID in HF could be considered as alternatives. According to data from animal studies presented above, cardiac iron import may be improved by stimulation of NTBI uptake. Another therapeutic concept that is worth to be explored may involve regulation of cardiac hepcidin/ferroportin machinery which may provide blockage of iron export. Further studies investigating the exact role of local iron homeostasis in myocardium and links between ID and malfunctioning of heart are therefore warranted (Fig. 2).
Fig. 2.
Effects of ID on structural and functional abnormalities occurring in mitochondria, cardiomyocyte, heart and the whole organism
Funding information
The present study was financially supported by the National Science Centre (Kraków, Poland; grant no. 2014/13/B/NZ5/03146).
Conflict of Interest
Wrocław Medical University received an unrestricted grant from Vifor Pharma outside the submitted work. Monika Kasztura reports financial support from Vifor Pharma for travel and accommodation for scientific meeting. Waldemar Banasiak reports personal fees from Vifor Pharma, outside the submitted work. Piotr Ponikowski reports personal fees from Vifor Pharma and personal fees from AMGEN, outside the submitted work. Ewa A. Jankowska reports personal fees from Vifor Pharma and FRESENIUS, outside the submitted work.
References
- 1.Abbaspour N, Hurrell R, Kelishadi R. Review on iron and its importance for human health. J Res Med Sci. 2014;19:164–174. [PMC free article] [PubMed] [Google Scholar]
- 2.Stehling O, Lill R. The role of mitochondria in cellular Iron-sulfur protein biogenesis: mechanisms, connected processes, and diseases. Cold Spring Harb Perspect Biol. 2013;5:a011312–a011312. doi: 10.1101/cshperspect.a011312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zannad F. Co-morbidities in heart failure, an issue of heart failure clinics. Elsevier Health Sciences: E-Book; 2014. [Google Scholar]
- 4.Stugiewicz M, Tkaczyszyn M, Kasztura M, Banasiak W, Ponikowski P, Jankowska EA. The influence of iron deficiency on the functioning of skeletal muscles: experimental evidence and clinical implications. Eur J Heart Fail. 2016;18:762–773. doi: 10.1002/ejhf.467. [DOI] [PubMed] [Google Scholar]
- 5.Jankowska EA, Kasztura M, Sokolski M, Bronisz M, Nawrocka S, Oleśkowska-Florek W, Zymliński R, Biegus J, Siwołowski P, Banasiak W, Anker SD, Filippatos G, Cleland JGF, Ponikowski P. Iron deficiency defined as depleted iron stores accompanied by unmet cellular iron requirements identifies patients at the highest risk of death after an episode of acute heart failure. Eur Heart J. 2014;35:2468–2476. doi: 10.1093/eurheartj/ehu235. [DOI] [PubMed] [Google Scholar]
- 6.Jankowska EA, von Haehling S, Anker SD, Macdougall IC, Ponikowski P. Iron deficiency and heart failure: diagnostic dilemmas and therapeutic perspectives. Eur Heart J. 2013;34:816–829. doi: 10.1093/eurheartj/ehs224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klip IT, Comin-Colet J, Voors AA, et al. Iron deficiency in chronic heart failure: An international pooled analysis. Am Heart J. 2013;165:575–582.e3. doi: 10.1016/j.ahj.2013.01.017. [DOI] [PubMed] [Google Scholar]
- 8.Okonko DO, Mandal AKJ, Missouris CG, Poole-Wilson PA. Disordered Iron homeostasis in chronic heart failure. J Am Coll Cardiol. 2011;58:1241–1251. doi: 10.1016/j.jacc.2011.04.040. [DOI] [PubMed] [Google Scholar]
- 9.van Veldhuisen DJ, Anker SD, Ponikowski P, Macdougall IC. Anemia and iron deficiency in heart failure: mechanisms and therapeutic approaches. Nat Rev Cardiol. 2011;8:485–493. doi: 10.1038/nrcardio.2011.77. [DOI] [PubMed] [Google Scholar]
- 10.McLean E, Cogswell M, Egli I, Wojdyla D, de Benoist B. Worldwide prevalence of anaemia, WHO vitamin and mineral nutrition information system, 1993–2005. Public Health Nutr. 2009;12:444. doi: 10.1017/S1368980008002401. [DOI] [PubMed] [Google Scholar]
- 11.Flanagan PR, Haist J, Valberg LS. Comparative effects of iron deficiency induced by bleeding and a low-iron diet on the intestinal absorptive interactions of iron, cobalt, manganese, zinc, lead and cadmium. J Nutr. 1980;110:1754–1763. doi: 10.1093/jn/110.9.1754. [DOI] [PubMed] [Google Scholar]
- 12.Nagababu E, Gulyani S, Earley CJ, Cutler RG, Mattson MP, Rifkind JM. Iron-deficiency anaemia enhances red blood cell oxidative stress. Free Radic Res. 2008;42:824–829. doi: 10.1080/10715760802459879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Toblli JE, Cao G, Rivas C, Giani JF, Dominici FP. Intravenous iron sucrose reverses anemia-induced cardiac remodeling, prevents myocardial fibrosis, and improves cardiac function by attenuating oxidative/nitrosative stress and inflammation. Int J Cardiol. 2016;212:84–91. doi: 10.1016/j.ijcard.2016.03.039. [DOI] [PubMed] [Google Scholar]
- 14.Naito Y, Tsujino T, Matsumoto M, Sakoda T, Ohyanagi M, Masuyama T. Adaptive response of the heart to long-term anemia induced by iron deficiency. Am J Physiol Heart Circ Physiol. 2009;296:H585–H593. doi: 10.1152/ajpheart.00463.2008. [DOI] [PubMed] [Google Scholar]
- 15.Olivetti G, Quaini F, Lagrasta C, et al (1992) Myocyte Cellular Hypertrophy and Hyperplasia Contribute to Ventricular Wall Remodeling in Anemia-induced Cardiac Hypertrophy in Rats Am J Pathol 141: [PMC free article] [PubMed]
- 16.Tanne Z, Coleman R, Nahir M, Shomrat D, Finberg JPM, Youdim MBH. Ultrastructural and cytochemical changes in the heart of iron-deficient rats. Biochem Pharmacol. 1994;47:1759–1766. doi: 10.1016/0006-2952(94)90303-4. [DOI] [PubMed] [Google Scholar]
- 17.Medeiros DM, Beard JL. Dietary iron deficiency results in cardiac eccentric hypertrophy in rats. Proc Soc Exp Biol Med. 1998;218(4):370–375. doi: 10.3181/00379727-218-44306. [DOI] [PubMed] [Google Scholar]
- 18.Maeder MT, Khammy O, dos Remedios C, Kaye DM. Myocardial and systemic Iron depletion in heart failure: implications for Anemia accompanying heart failure. J Am Coll Cardiol. 2011;58:474–480. doi: 10.1016/j.jacc.2011.01.059. [DOI] [PubMed] [Google Scholar]
- 19.Anand IS, Gupta P. Anemia and Iron deficiency in heart failure. Circulation. 2018;138:80–98. doi: 10.1161/CIRCULATIONAHA.118.030099. [DOI] [PubMed] [Google Scholar]
- 20.Turner LR, Premo DA, Gibbs BJ, Hearthway ML, Motsko M, Sappington A, Walker LA, Mullendore ME, Chew HG. Adaptations to iron deficiency: cardiac functional responsiveness to norepinephrine, arterial remodeling, and the effect of beta-blockade on cardiac hypertrophy. BMC Physiol. 2002;2:1. doi: 10.1186/1472-6793-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duke M, Abelmann WH. The hemodynamic response to chronic anemia. Circulation. 1969;39:503–515. doi: 10.1161/01.CIR.39.4.503. [DOI] [PubMed] [Google Scholar]
- 22.Petering DH, Stemmer KL, Lyman S, et al (1990) Iron deficiency in growing male rats: a cause of development of cardiomyopathy. Ann Nutr Metab 34:(4)232–243. http://www.ncbi.nlm.nih.gov/pubmed/2400205. Accessed September 22, 2017 [DOI] [PubMed]
- 23.Dong F, Zhang X, Culver B, Chew HG, Jr, Kelley RO, Ren J. Dietary iron deficiency induces ventricular dilation, mitochondrial ultrastructural aberrations and cytochrome c release: involvement of nitric oxide synthase and protein tyrosine nitration. Clin Sci. 2005;109:277–286. doi: 10.1042/CS20040278. [DOI] [PubMed] [Google Scholar]
- 24.Tsutsui H, Kinugawa S, Matsushima S. Mitochondrial oxidative stress and dysfunction in myocardial remodelling. Cardiovasc Res. 2008;81:449–456. doi: 10.1093/cvr/cvn280. [DOI] [PubMed] [Google Scholar]
- 25.Nur-E-Kamal A, Gross SR, Pan Z, Balklava Z, Ma J, Liu LF. Nuclear translocation of cytochrome c during apoptosis. J Biol Chem. 2004;279:24911–24914. doi: 10.1074/jbc.C400051200. [DOI] [PubMed] [Google Scholar]
- 26.Gargalovic P, Dory L. Cellular apoptosis is associated with increased caveolin-1 expression in macrophages. J Lipid Res. 2003;44:1622–1632. doi: 10.1194/jlr.M300140-JLR200. [DOI] [PubMed] [Google Scholar]
- 27.Blayney L, Bailey-Wood R, Jacobs A, Henderson A, Muir J. The effects of iron deficiency on the respiratory function and cytochrome content of rat heart mitochondria. Circ Res. 1976;39(5):744–748. doi: 10.1161/01.RES.39.5.744. [DOI] [PubMed] [Google Scholar]
- 28.Ponka P, Lok CN. The transferrin receptor: role in health and disease. Int J Biochem Cell Biol. 1999;31:1111–1137. doi: 10.1016/S1357-2725(99)00070-9. [DOI] [PubMed] [Google Scholar]
- 29.Hentze MW, Muckenthaler MU, Andrews NC. Balancing acts: molecular control of mammalian iron metabolism. Cell. 2004;117:285–297. doi: 10.1016/S0092-8674(04)00343-5. [DOI] [PubMed] [Google Scholar]
- 30.Andrews N, Levy JE, Jin O, Fujiwara Y, Kuo F. Transferrin receptor is necessary for development of erythrocytes and the nervous system. Nat Genet. 1999;21:396–399. doi: 10.1038/7727. [DOI] [PubMed] [Google Scholar]
- 31.Xu W, Barrientos T, Mao L, Rockman HA, Sauve AA, Andrews NC. Lethal cardiomyopathy in mice lacking transferrin receptor in the heart. Cell Rep. 2015;13:533–545. doi: 10.1016/j.celrep.2015.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stehling O, Mascarenhas J, Vashisht AA, Sheftel AD, Niggemeyer B, Rösser R, Pierik AJ, Wohlschlegel JA, Lill R. Human CIA2A-FAM96A and CIA2B-FAM96B integrate Iron homeostasis and maturation of different subsets of cytosolic-nuclear Iron-sulfur proteins. Cell Metab. 2013;18:187–198. doi: 10.1016/j.cmet.2013.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xu W, Barrientos T, Andrews NC. Iron and copper in mitochondrial diseases. Cell Metab. 2013;17:319–328. doi: 10.1016/j.cmet.2013.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ganz T. Cellular iron: Ferroportin is the only way out. Cell Metab. 2005;1:155–157. doi: 10.1016/j.cmet.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 35.Roetto A, Papanikolaou G, Politou M, Alberti F, Girelli D, Christakis J, Loukopoulos D, Camaschella C. Mutant antimicrobial peptide hepcidin is associated with severe juvenile hemochromatosis. Nat Genet. 2002;33:21–22. doi: 10.1038/ng1053. [DOI] [PubMed] [Google Scholar]
- 36.Nemeth E, Tuttle MS, Powelson J et al (2004) Hepcidin regulates cellular Iron efflux by binding to Ferroportin and inducing its internalization. Science (80- ) 306:2090–2093. 10.1126/science.1104742 [DOI] [PubMed]
- 37.Merle U, Fein E, Gehrke SG, Stremmel W, Kulaksiz H. The Iron regulatory peptide Hepcidin is expressed in the heart and regulated by hypoxia and inflammation. Endocrinology. 2007;148:2663–2668. doi: 10.1210/en.2006-1331. [DOI] [PubMed] [Google Scholar]
- 38.Kulaksiz H, Theilig F, Bachmann S, Gehrke SG, Rost D, Janetzko A, Cetin Y, Stremmel W. The iron-regulatory peptide hormone hepcidin: expression and cellular localization in the mammalian kidney. J Endocrinol. 2005;184:361–370. doi: 10.1677/joe.1.05729. [DOI] [PubMed] [Google Scholar]
- 39.McCarthy RC, Kosman DJ. Glial cell Ceruloplasmin and Hepcidin differentially regulate Iron efflux from brain microvascular endothelial cells. PLoS One. 2014;9:e89003. doi: 10.1371/journal.pone.0089003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Evans P, Cindrova-Davies T, Muttukrishna S, Burton GJ, Porter J, Jauniaux E. Hepcidin and iron species distribution inside the first-trimester human gestational sac. Mol Hum Reprod. 2011;17:227–232. doi: 10.1093/molehr/gaq101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vela D. Balance of cardiac and systemic hepcidin and its role in heart physiology and pathology. Lab Investig. 2017;98:315–326. doi: 10.1038/labinvest.2017.111. [DOI] [PubMed] [Google Scholar]
- 42.Lakhal-Littleton S, Wolna M, Carr CA, Miller JJJ, Christian HC, Ball V, Santos A, Diaz R, Biggs D, Stillion R, Holdship P, Larner F, Tyler DJ, Clarke K, Davies B, Robbins PA. Cardiac ferroportin regulates cellular iron homeostasis and is important for cardiac function. Proc Natl Acad Sci. 2015;112:3164–3169. doi: 10.1073/pnas.1422373112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lakhal-Littleton S, Wolna M, Chung YJ, Christian HC, Heather LC, Brescia M, Ball V, Diaz R, Santos A, Biggs D, Clarke K, Davies B, Robbins PA (2016) An essential cell-autonomous role for hepcidin in cardiac iron homeostasis. Elife 5. 10.7554/eLife.19804 [DOI] [PMC free article] [PubMed]
- 44.Drakesmith H, Schimanski LM, Ormerod E, Merryweather-Clarke AT, Viprakasit V, Edwards JP, Sweetland E, Bastin JM, Cowley D, Chinthammitr Y, Robson KJ, Townsend AR. Resistance to hepcidin is conferred by hemochromatosis-associated mutations of ferroportin. Blood. 2005;106:1092–1097. doi: 10.1182/blood-2005-02-0561. [DOI] [PubMed] [Google Scholar]
- 45.Schimanski LM, Drakesmith H, Merryweather-Clarke AT, Viprakasit V, Edwards JP, Sweetland E, Bastin JM, Cowley D, Chinthammitr Y, Robson KJ, Townsend AR. In vitro functional analysis of human ferroportin (FPN) and hemochromatosis-associated FPN mutations. Blood. 2005;105:4096–4102. doi: 10.1182/blood-2004-11-4502. [DOI] [PubMed] [Google Scholar]
- 46.Anderson CP, Shen M, Eisenstein RS, Leiboldac EA (2012) Mammalian iron metabolism and its control by iron regulatory proteins. Biochim Biophys Acta - Mol Cell Res 1823:1468–1483. 10.1016/J.BBAMCR.2012.05.010 [DOI] [PMC free article] [PubMed]
- 47.Hentze MW, Muckenthaler MU, Galy B, Camaschella C. Two to tango: regulation of mammalian Iron metabolism. Cell. 2010;142:24–38. doi: 10.1016/j.cell.2010.06.028. [DOI] [PubMed] [Google Scholar]
- 48.Styś A, Galy B, Starzyński RR, Smuda E, Drapier JC, Lipiński P, Bouton C. Iron regulatory protein 1 outcompetes iron regulatory protein 2 in regulating cellular iron homeostasis in response to nitric oxide. J Biol Chem. 2011;286:22846–22854. doi: 10.1074/jbc.M111.231902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Volz K (2008) The functional duality of iron regulatory protein 1. Curr Opin Struct Biol 18:106–111. 10.1016/j.sbi.2007.12.010 [DOI] [PMC free article] [PubMed]
- 50.Haddad S, Wang Y, Galy B, et al. Iron-regulatory proteins secure iron availability in cardiomyocytes to prevent heart failure. Eur heart J. 2016;38:ehw333. doi: 10.1093/eurheartj/ehw333. [DOI] [PubMed] [Google Scholar]
- 51.Jankowska EA, Rozentryt P, Witkowska A, Nowak J, Hartmann O, Ponikowska B, Borodulin-Nadzieja L, Banasiak W, Polonski L, Filippatos G, McMurray JJV, Anker SD, Ponikowski P. Iron deficiency: an ominous sign in patients with systolic chronic heart failure. Eur Heart J. 2010;31:1872–1880. doi: 10.1093/eurheartj/ehq158. [DOI] [PubMed] [Google Scholar]
- 52.Cohen-Solal A, Damy T, Terbah M, Kerebel S, Baguet JP, Hanon O, Zannad F, Laperche T, Leclercq C, Concas V, Duvillié L, Darné B, Anker S, Mebazaa A. High prevalence of iron deficiency in patients with acute decompensated heart failure. Eur J Heart Fail. 2014;16:984–991. doi: 10.1002/ejhf.139. [DOI] [PubMed] [Google Scholar]
- 53.Núñez J, Comín-Colet J, Miñana G, Núñez E, Santas E, Mollar A, Valero E, García-Blas S, Cardells I, Bodí V, Chorro FJ, Sanchis J. Iron deficiency and risk of early readmission following a hospitalization for acute heart failure. Eur J Heart Fail. 2016;18:798–802. doi: 10.1002/ejhf.513. [DOI] [PubMed] [Google Scholar]
- 54.Melenovsky V, Petrak J, Mracek T, Benes J, Borlaug BA, Nuskova H, Pluhacek T, Spatenka J, Kovalcikova J, Drahota Z, Kautzner J, Pirk J, Houstek J. Myocardial iron content and mitochondrial function in human heart failure: a direct tissue analysis. Eur J Heart Fail. 2017;19(4):522–530. doi: 10.1002/ejhf.640. [DOI] [PubMed] [Google Scholar]
- 55.Leszek P, Sochanowicz B, Szperl M, Kolsut P, Brzóska K, Piotrowski W, Rywik TM, Danko B, Polkowska-Motrenko H, Różański JM, Kruszewski M. Myocardial iron homeostasis in advanced chronic heart failure patients. Int J Cardiol. 2012;159:47–52. doi: 10.1016/j.ijcard.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 56.Hoes MF, Grote Beverborg N, Kijlstra JD, Kuipers J, Swinkels DW, Giepmans BNG, Rodenburg RJ, van Veldhuisen DJ, de Boer RA, van der Meer P. Iron deficiency impairs contractility of human cardiomyocytes through decreased mitochondrial function. Eur J Heart Fail. 2018;20:910–919. doi: 10.1002/ejhf.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kasztura M, Dzięgała M, Kobak K, Bania J, Mazur G, Banasiak W, Ponikowski P, Jankowska EA. Both iron excess and iron depletion impair viability of rat H9C2 cardiomyocytes and L6G8C5 myocytes. Kardiol Pol. 2017;75:267–275. doi: 10.5603/KP.a2016.0155. [DOI] [PubMed] [Google Scholar]
- 58.Dziegala M, Kasztura M, Kobak K, Bania J, Banasiak W, Ponikowski P, Jankowska EA. Influence of the availability of iron during hypoxia on the genes associated with apoptotic activity and local iron metabolism in rat H9C2 cardiomyocytes and L6G8C5 skeletal myocytes. Mol Med Rep. 2016;14:3969–3977. doi: 10.3892/mmr.2016.5705. [DOI] [PubMed] [Google Scholar]
- 59.Nagao M, Matsuo Y, Kamitani T, Yonezawa M, Yamasaki Y, Kawanami S, Abe K, Mukai Y, Higo T, Yabuuchi H, Takemura A, Yoshiura T, Sunagawa K, Honda H. Quantification of myocardial Iron deficiency in nonischemic heart failure by cardiac T2* magnetic resonance imaging. Am J Cardiol. 2014;113:1024–1030. doi: 10.1016/j.amjcard.2013.11.061. [DOI] [PubMed] [Google Scholar]
- 60.Nagao M, Baba S, Yonezawa M, Yamasaki Y, Kamitani T, Isoda T, Kawanami S, Maruoka Y, Kitamura Y, Abe K, Higo T, Sunagawa K, Honda H. Prediction of adverse cardiac events in dilated cardiomyopathy using cardiac T2* MRI and MIBG scintigraphy. Int J Cardiovasc Imaging. 2015;31:399–407. doi: 10.1007/s10554-014-0562-1. [DOI] [PubMed] [Google Scholar]
- 61.Núñez J, Monmeneu JV, Mollar A, Núñez E, Bodí V, Miñana G, García-Blas S, Santas E, Agüero J, Chorro FJ, Sanchis J, López-Lereu MP. Left ventricular ejection fraction recovery in patients with heart failure treated with intravenous iron: a pilot study. ESC Hear Fail. 2016;3:293–298. doi: 10.1002/ehf2.12101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Terrovitis JV, Kaldara E, Ntalianis A, Sventzouri S, Kapelios C, Barbarousi D, Matsouka C, Nanas JN. Intravenous Iron alone is equally effective with the combination of Iron and erythropoietin for the treatment of Iron-deficiency Anemia in advanced heart failure. J Am Coll Cardiol. 2012;60:2255–2256. doi: 10.1016/j.jacc.2012.05.065. [DOI] [PubMed] [Google Scholar]
- 63.McDonagh T, Macdougall IC. Iron therapy for the treatment of iron deficiency in chronic heart failure: intravenous or oral? Eur J Heart Fail. 2015;17:248–262. doi: 10.1002/ejhf.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lewis GD, Malhotra R, Hernandez AF, McNulty SE, Smith A, Felker GM, Tang WHW, LaRue SJ, Redfield MM, Semigran MJ, Givertz MM, van Buren P, Whellan D, Anstrom KJ, Shah MR, Desvigne-Nickens P, Butler J, Braunwald E, for the NHLBI Heart Failure Clinical Research Network Effect of Oral Iron repletion on exercise capacity in patients with heart failure with reduced ejection fraction and Iron deficiency. JAMA. 2017;317:1958–1966. doi: 10.1001/jama.2017.5427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Anker SD, Comin Colet J, Filippatos G, Willenheimer R, Dickstein K, Drexler H, Lüscher TF, Bart B, Banasiak W, Niegowska J, Kirwan BA, Mori C, von Eisenhart Rothe B, Pocock SJ, Poole-Wilson PA, Ponikowski P, FAIR-HF Trial Investigators Ferric Carboxymaltose in patients with heart failure and Iron deficiency. N Engl J Med. 2009;361:2436–2448. doi: 10.1056/NEJMoa0908355. [DOI] [PubMed] [Google Scholar]
- 66.Ponikowski P, van Veldhuisen DJ, Comin-Colet J, Ertl G, Komajda M, Mareev V, McDonagh T, Parkhomenko A, Tavazzi L, Levesque V, Mori C, Roubert B, Filippatos G, Ruschitzka F, Anker SD, for the CONFIRM-HF Investigators Beneficial effects of long-term intravenous iron therapy with ferric carboxymaltose in patients with symptomatic heart failure and iron deficiency. Eur Heart J. 2015;36:657–668. doi: 10.1093/eurheartj/ehu385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Filippatos G, Farmakis D, Colet JC, Dickstein K, Lüscher TF, Willenheimer R, Parissis J, Gaudesius G, Mori C, von Eisenhart Rothe B, Greenlaw N, Ford I, Ponikowski P, Anker SD. Intravenous ferric carboxymaltose in iron-deficient chronic heart failure patients with and without anaemia: a subanalysis of the FAIR-HF trial. Eur J Heart Fail. 2013;15:1267–1276. doi: 10.1093/eurjhf/hft099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bolger AP, Bartlett FR, Penston HS, O’Leary J, Pollock N, Kaprielian R, Chapman CM. Intravenous Iron alone for the treatment of Anemia in patients with chronic heart failure. J Am Coll Cardiol. 2006;48:1225–1227. doi: 10.1016/j.jacc.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 69.Toblli JE, Lombraña A, Duarte P, Di Gennaro F. Intravenous Iron reduces NT-pro-brain natriuretic peptide in anemic patients with chronic heart failure and renal insufficiency. J Am Coll Cardiol. 2007;50:1657–1665. doi: 10.1016/j.jacc.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 70.Okonko DO, Grzeslo A, Witkowski T, Mandal AKJ, Slater RM, Roughton M, Foldes G, Thum T, Majda J, Banasiak W, Missouris CG, Poole-Wilson PA, Anker SD, Ponikowski P. Effect of intravenous Iron sucrose on exercise tolerance in anemic and nonanemic patients with symptomatic chronic heart failure and Iron deficiency. J Am Coll Cardiol. 2008;51:103–112. doi: 10.1016/j.jacc.2007.09.036. [DOI] [PubMed] [Google Scholar]
- 71.Usmanov RI, Zueva EB, Silverberg DS, Shaked M Intravenous iron without erythropoietin for the treatment of iron deficiency anemia in patients with moderate to severe congestive heart failure and chronic kidney insufficiency. J Nephrol 21:236–242 [PubMed]
- 72.Gaber R, Kotb NA, Ghazy M, Nagy HM, Salama M, Elhendy A. Tissue Doppler and strain rate imaging detect improvement of myocardial function in Iron deficient patients with congestive heart failure after Iron replacement therapy. Echocardiography. 2012;29:13–18. doi: 10.1111/j.1540-8175.2011.01532.x. [DOI] [PubMed] [Google Scholar]
- 73.Ke Y, Chen YY, Chang YZ, Duan XL, Ho KP, Jiang DH, Wang K, Qian ZM. Post-transcriptional expression of DMT1 in the heart of rat. J Cell Physiol. 2003;196:124–130. doi: 10.1002/jcp.10284. [DOI] [PubMed] [Google Scholar]
- 74.Zhabyeyev P, Oudit GY. Unravelling the molecular basis for cardiac iron metabolism and deficiency in heart failure. Eur heart J. 2016;38:ehw386. doi: 10.1093/eurheartj/ehw386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, ESC Scientific Document Group 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2016;37:2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]