Abstract
Extremes in sleep duration are associated with higher cardiovascular risk in the general population, but their impact in patients with documented coronary artery disease (CAD) remains unknown and potentially of clinical significance. We hypothesized that both short and long sleep duration are associated with higher mortality in CAD. We inquired about sleep durations in 2,846 patients enrolled in the Emory Cardiovascular Biobank (mean age 64 years, 38% female, 23% Black, and 82% with obstructive CAD, defined by positive coronary angiography), who were then followed for all-cause and cardiovascular mortality. Multivariate Cox proportional hazard models were calculated to examine the association of sleep duration and mortality. Sleep durations of <6.5 hours (short), ≥6.5 to <7.5 hours (normal), and ≥ 7.5 hours (long), were reported by 39%, 26% and 35% of the cohort, respectively. On follow-up (median 2.8 years), mortality rates were 15%, 11%, and 17%, respectively. After adjusting for demographics and risk factors, both short and long sleep duration were associated with higher all-cause mortality (HR 1.44, 95% CI [1.10–1.89] and 1.41 [1.08–1.85], respectively). A similar pattern was demonstrated for cardiovascular mortality only for short (HR 1.48 [1.05–2.09]), but not long sleep duration. In conclusion, in patients with frank CAD, both short and long sleep duration were independently associated with higher all-cause mortality, and short sleep was independently associated with higher cardiovascular mortality. In conclusion, our study is the first to extend the observations of sleep duration and mortality from population-based studies to patients with documented cardiac disease.
Keywords: Sleep duration, cardiovascular disease, coronary artery disease, mortality
INTRODUCTION
Many population-based epidemiologic studies have shown that both short and long reported sleep durations are associated with cardiovascular mortality and morbidity,1,2 but whether the length of sleep that a patient reports has implications in a clinical setting is far from certain. Self-reports about sleep are subject to many sources of error, including but not limited to: inherent lack of correlation with objective markers,3 imprecision based on poor recall or inadequate reporting,4 or psychiatric disorder.5 In the context of a patient in a lab immediately prior to cardiac catheterization, one could envision additional stressors that would further erode the value of this estimate. In this study, we report on our experience of routinely inquiring about sleep duration in a cardiac population in a catheterization laboratory. Specifically, we examined prospectively cardiac events and morbidities subsequent to this procedure.
METHODS
A total of 2,846 patients with completed sleep questionnaires were recruited between 2004 and 2016 as part of the Emory Cardiovascular Biobank,6 a prospective registry of consecutive patients undergoing cardiac catheterization for suspected or known CAD across Emory Healthcare sites. Patients with congenital heart disease, severe valvular heart disease, severe anemia, recent blood transfusion, myocarditis, active inflammatory diseases, cancer and cardiac transplant were excluded. Recruited patients were interviewed at the time of enrollment to collect demographic characteristics and medical history. Risk factors were determined by physician diagnoses or self-reported treatment for conditions such as hypertension, hyperlipidemia, diabetes mellitus, history of smoking, and history of previous MI. Hours of daily sleep were reported as part of a self-administered enrollment questionnaire. Coronary angiograms from the index cardiac catheterization at the time of enrollment were available in 89% of participants and reviewed to calculate Gensini score,7 a quantitative scoring system of coronary luminal narrowing. The presence of obstructive CAD, defined as ≥50% luminal narrowing in a major epicardial vessel, was also assessed in 89% of the patients. Presentation with acute MI at enrollment and coronary revascularization as a result of the index cardiac catheterization were determined. The study was approved by the Institutional Review Board of Emory University and all patients provided written informed consent.
Subjects were asked to provide a free-text response to the question: “How many hours of sleep do you usually get each night (or when you usually sleep)?” While the majority of the subjects reported in whole numbers of hours, 9 subjects reported to the first decimal place, e.g. 8.5 hours. The reported sleep duration was categorized into short (< 6.5 hours per day), normal (≥ 6.5 to < 7.5 hours per day), or long (≥ 7.5 hours per day) sleep duration, for the data analysis. Because categories of normal, short and long sleep duration often vary across studies (see Discussion), we also analyzed our data using 1-hour interval bins to examine the extent to which associations might occur in a more graded manner.
Follow-up was conducted by independent personnel blinded to the angiographic, sleep and clinical data. All-cause and cardiovascular-specific mortality was determined through verbal communications with family, Georgia vital records, and the Social Security Death Index. Medical records and death certificates were obtained and reviewed by an adjudication committee of three physicians also blinded to the data. Cardiovascular death was defined as death attributable to an ischemic cardiovascular cause (fatal MI, ischemic stroke, peripheral arterial disease), vascular cause, or sudden death attributable to an unknown but presumed cardiovascular cause in high-risk patients.
Continuous variables were presented as means (standard deviation) or as median (interquartile range) and categorical variables were reported as frequency counts and proportions (%). Chi-square test was used to compare proportions, while one-way analysis of variance with Tukey post-hoc analysis was conducted to determine whether differences in continuous variables existed between groups stratified by sleep duration. Multivariable analysis to identify variables independently associated with sleep duration was performed using multinomial logistic regression. The covariates included age, sex, race (black vs. non-black), body mass index (BMI), hypertension, diabetes, hyperlipidemia, smoking history, prior MI, heart failure, acute myocardial infarction at enrollment (Y or N), revascularization (Y or N) at enrollment, and obstructive CAD (Y or N; defined by the presence of ≥50% obstructive lesion in any of the major epicardial vessels on coronary angiography at enrollment).
Survival analysis comparing patients stratified according to sleep duration was performed using Kaplan-Meier survival curves, log-rank tests as well as Cox proportional hazards modeling with the aforementioned covariates for all-cause death and cardiovascular death. Sensitivity analysis was performed to determine whether the association with outcomes differed with respect to the presence of the individual covariates by including the interaction term of sleep duration × the covariate of interest. Proportional hazards assumption was examined by plotting Schoenfeld residuals for each covariate against time as well as including an interaction term of each covariate by time in the Cox models, and no significant violations were observed. Two-tailed P-values<0.05 were considered statistically significant, and all analyses were performed with SPSS 24 (IBM, Armonk, NY).
RESULTS
Overall, the cohort comprised of 2,846 subjects with a mean age of 64 years, 38% women and 23% Black (Table 1). The mean duration of daily sleep was 6.8 ± 1.5 hours. Overall, 39% of subjects reported short (< 6.5 hours per day), 35% reported long (≥ 7.5 hours per day) and 26% reported normal duration of sleep (≥ 6.5 to < 7.5 hours per day; Table 1).
Table 1.
Baseline characteristics and incident clinical outcomes according to the duration of daily sleep*
| Variable | All (N=2846) | Short (< 6.5 H) (N=1119) | Normal (≥ 6.5 to < 7.5 H) (N=741) | Long (≥ 7.5 H) (N=986) | Overall P-value | P-value for pairwise comparison |
||
|---|---|---|---|---|---|---|---|---|
| Normal vs short | Normal vs long | Short vs long | ||||||
| Age (years) | 64 ± 13 | 62 ± 12 | 64 ± 12 | 66 ± 13 | <0.001 | 0.006 | <0.001 | <0.001 |
| Women | 1071 (38%) | 472 (42%) | 254 (34%) | 345 (35%) | <0.001 | 0.001 | 0.76 | 0.001 |
| Black | 642 (23%) | 372 (33%) | 124 (17%) | 146 (15%) | <0.001 | <0.001 | 0.28 | <0.001 |
| Body mass index (kg/m2) | 30 ± 6 | 31 ± 7 | 30 ± 6 | 29 ± 6 | <0.001 | <0.001 | 0.61 | <0.001 |
| Hypertension | 2427 (85%) | 968 (87%) | 624 (84%) | 836 (85%) | 0.37 | 0.20 | 0.80 | 0.27 |
| Diabetes mellitus | 1064 (38%) | 441 (40%) | 258 (35%) | 365 (37%) | 0.13 | 0.05 | 0.34 | 0.27 |
| Hyperlipidemia† | 2139 (75%) | 838 (75%) | 535 (72%) | 766 (78%) | 0.04 | 0.17 | 0.01 | 0.17 |
| Smoker | 2067 (73%) | 800 (72%) | 522 (70%) | 745 (76%) | 0.03 | 0.63 | 0.02 | 0.04 |
| Prior MI | 642 (23%) | 241 (22%) | 149 (21 %) | 252 (26%) | 0.02 | 0.46 | 0.01 | 0.04 |
| Heart failure | 987 (35%) | 412 (37%) | 230 (31%) | 345 (35%) | 0.04 | 0.01 | 0.09 | 0.38 |
| Ejection fraction (%) | 53 ± 12 | 53 ± 13 | 54 ± 11 | 52 ± 13 | 0.01 | 0.04 | 0.02 | 0.88 |
| Gensini score, points | 86 [2,240] | 80 [0,234] | 85 [2,244] | 112 [4,256] | 0.07 | 0.91 | 0.83 | 0.06 |
| Obstructive CAD‡ | 2082 (82%) | 792 (81%) | 542 (81%) | 748 (84%) | 0.20 | 0.68 | 0.24 | 0.08 |
| Acute MI at enrollment | 228 (8%) | 90 (8%) | 60 (8%) | 78 (8%) | 0.99 | 0.97 | 0.89 | 0.97 |
| Revascularization at enrollment | 941 (33%) | 373 (33%) | 253 (34%) | 315 (32%) | 0.61 | 0.72 | 0.34 | 0.50 |
| All-cause death | 412 (15%) | 166 (15%) | 81 (11%) | 165 (17%) | 0.003 | 0.02 | 0.001 | 0.05 |
| Cardiovascular death | 251 (9%) | 111 (10%) | 50 (7%) | 90 (9%) | 0.06 | 0.02 | 0.07 | 0.77 |
| Myocardial infarction | 107 (4%) | 42 (4%) | 22 (3%) | 43 (4%) | 0.32 | 0.36 | 0.13 | 0.99 |
| Coronary revascularization | 587 (21%) | 236 (21%) | 150 (20%) | 201 (20%) | 0.88 | 0.66 | 0.94 | 0.73 |
| Stroke | 68 (2%) | 25 (2%) | 18 (2%) | 25 (3%) | 0.90 | 0.78 | 0.89 | 0.65 |
Values are mean (SD), median [25th and 75th interquartile range], or n (%).
Defined by physician diagnosis in medical charts
Obstructive coronary artery disease (CAD) is defined by the presence of ≥50% obstructive lesion in any of the major epicardial vessels on coronary angiography at enrollment.
Abbreviations: MI = myocardial infraction; CAD = coronary artery disease
Subjects reporting short duration of sleep were likely to be younger, female and Black with higher BMI, diabetes, and heart failure than those with normal sleep duration on univariate analysis (Table 1). Patients with long duration of sleep were older and more likely to have a history of hyperlipidemia, smoking, and prior MI than those with normal sleep duration (Table 1). In multinomial logistic regression analyses, independent predictors of short sleep duration were female sex, Black race, and higher BMI, whereas older age and history of smoking were independently associated with long sleep duration (Table 2). There was no significant difference in the prevalence of obstructive CAD at enrollment among the 3 groups of sleep duration while there was statistically insignificant increase in Gensini score among those with long sleep compared to those with short sleep duration (P=0.06; Table 1). However, neither obstructive CAD nor Gensini score was predictive of either short or long sleep duration (Table 2).
Table 2.
Multinomial logistic regression of daily sleep duration and baseline demographic and clinical characteristics
| Variable | Short (< 6.5 H) vs. Normal (≥ 6.5to < 7.5 H) |
Long (≥ 8.5 H) vs. Normal (≥ 6.5 to <7 .5 H) |
||
|---|---|---|---|---|
| OR, 95% C.I. | P-value | OR, 95% C.I. | P-value | |
| Age, per increase of 10 years | 0.94 (0.85 – 1.03) | 0.17 | 1.13 (1.03 – 1.25) | 0.014 |
| Body mass index, per 5kg/m2 | 1.11 (1.01 – 1.21) | 0.027 | 0.99 (0.90 – 1.08) | 0.75 |
| Women | 1.34 (1.07 – 1.68) | 0.011 | 1.01 (0.80 – 1.27) | 0.96 |
| Black | 1.95 (1.49 – 2.57) | <0.001 | 0.82 (0.60 – 1.11) | 0.20 |
| Hypertension | 1.00 (0.73 – 1.38) | 0.99 | 0.88 (0.64 – 1.20) | 0.88 |
| Diabetes mellitus | 1.00 (0.80 – 1.27) | 0.98 | 1.08 (0.85 – 1.36) | 0.54 |
| Hyperlipidemia | 1.28 (0.99 – 1.66) | 0.06 | 1.27 (0.98 – 1.65) | 0.07 |
| Smoker | 1.11 (0.88 – 1.40) | 0.40 | 1.36 (1.07 – 1.73) | 0.013 |
| Prior MI | 1.03 (0.79 – 1.35) | 0.83 | 1.26 (0.97 – 1.65) | 0.09 |
| Heart failure | 1.10 (0.87 – 1.39) | 0.42 | 1.12 (0.88 – 1.42) | 0.35 |
| Acute MI at enrollment | 1.08 (0.72 – 1.62) | 0.71 | 1.03 (0.69 – 1.55) | 0.88 |
| Revascularization at enrollment | 1.07 (0.84 – 1.36) | 0.57 | 0.85 (0.67 – 1.08) | 0.19 |
| Gensini score, per 10 points | 1.00 (1.00 – 1.01) | 0.58 | 1.00 (0.99 – 1.01) | 0.99 |
| Obstructive CAD* | 1.04 (0.79 – 1.38) | 0.77 | 0.98 (0.73 – 1.31) | 0.88 |
Obstructive coronary artery disease (CAD) is defined by the presence of ≥50% obstructive lesion in any of the major epicardial vessels on coronary angiography at enrollment.
Abbreviations: OR = odds ratio; C.I. = confidence interval; MI = myocardial infraction; CAD = coronary artery disease
During a median 2.8 year follow-up period, there were 412 (15%) all-cause deaths, and 251(9%) cardiovascular deaths (Table 1). Kaplan-Meier survival analysis revealed that all-cause mortality was significantly different among the groups reporting short (15%), normal (11%) and long (17%) sleep duration (Log-rank P=0.003, Figure 1A). Unadjusted Cox proportional hazard model showed that compared to normal sleep duration, both short and long sleep duration were associated with higher all-cause mortality rate (Table 3, Model 1), which remained significant after adjusting for age, sex, race, BMI, hypertension, diabetes, hyperlipidemia, history of smoking, history of prior MI, and heart failure (HR 1.44, 95% CI [1.10–1.89] and 1.41 [1.08–1.85], respectively; Table 3, Model 2) and after adjustment for CAD severity (Table 3, Model 3). We also calculated the risk of all-cause mortality sequentially with a 1-hour incremental change from the reference duration of sleep (≥ 6.5 to < 7.5 hours per day) in the fully adjusted model (Model 3). The adjusted risk of all-cause mortality increased with increasing and decreasing duration of sleep compared to those reporting the reference duration of daily sleep. Specifically, those with extremely short sleep duration (<4.5 hours per day) had an adjusted HR of 1.96 and those with extremely long ≥8.5 hours of sleep per day had a HR 1.84 for all-cause mortality compared to those with a normal sleep duration (Figure 2A).
Figure 1.
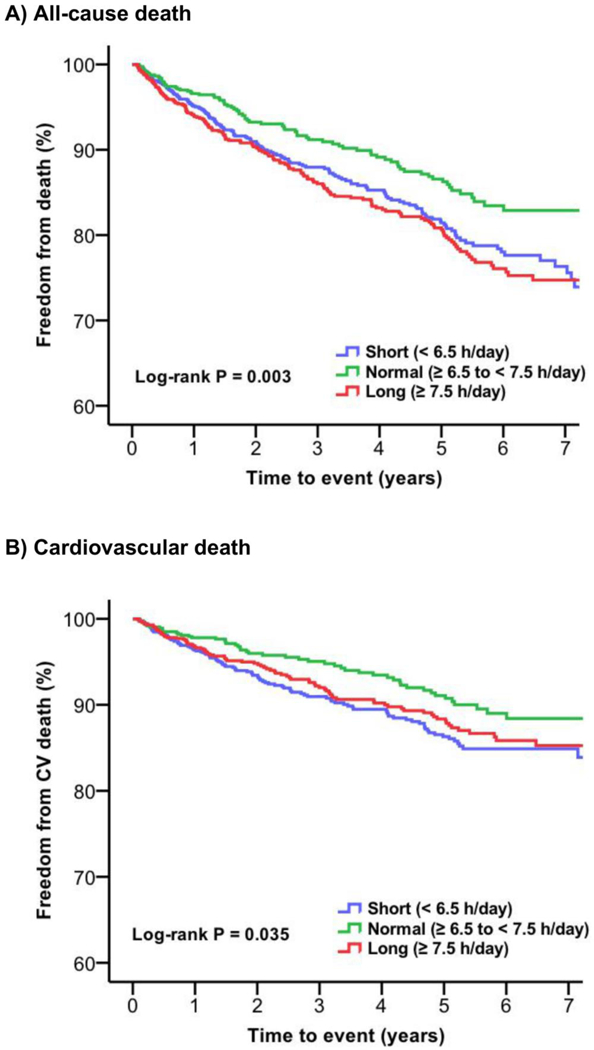
Kaplan-Meier curves for all-cause and cardiovascular death stratified by the duration of daily sleep.
Table 3.
Association between the duration of daily sleep and all-cause / cardiovascular mortality
| Outcome | Model | Short vs normal |
Long vs normal |
||
|---|---|---|---|---|---|
| HR, 95% C.I. | P-value | HR, 95% C.I. | P-value | ||
| All death | Model 1 (Unadjusted) | 1.43 (1.09–1.86) | 0.009 | 1.58 (1.21–2.06) | 0.001 |
| Model 2 (Model 1 + CV risk factors*) | 1.44 (1.10–1.89) | 0.009 | 1.41 (1.08–1.85) | 0.013 | |
| Model 3 (Model 2 + CAD severity†) | 1.56 (1.16–2.10) | 0.003 | 1.47 (1.10–1.96) | 0.010 | |
| Cardiovascular death | Model 1 (Unadjusted) | 1.55 (1.11–2.16) | 0.011 | 1.40 (0.99–1.98) | 0.056 |
| Model 2 (Model 1 + CV risk factors*) | 1.48 (1.05–2.09) | 0.026 | 1.24 (0.87–1.77) | 0.229 | |
| Model 3 (Model 2 + CAD severity†) | 1.49 (1.03–2.15) | 0.035 | 1.19 (0.82–1.73) | 0.371 | |
Includes age (continuous), sex (male vs female), race (Black vs non-Black), body mass index (continuous), hypertension (Y or N), diabetes mellitus (Y or N), hyperlipidemia (Y or N), history of smoking (Y or N), prior MI (Y or N), and heart failure (Y or N)
Includes acute myocardial infarction at enrollment (Y or N), revascularization (Y or N) at enrollment, and obstructive CAD (Y or N; defined by the presence of ≥50% obstructive lesion in any of the major epicardial vessels on coronary angiography at enrollment).
Abbreviations: HR = hazard ratio; C.I. = confidence interval; CV=cardiovascular; CAD = coronary artery disease
Figure 2. Adjusted hazard ratio of all-cause (A) and cardiovascular (B) mortality stratified by the hours of daily sleep duration.
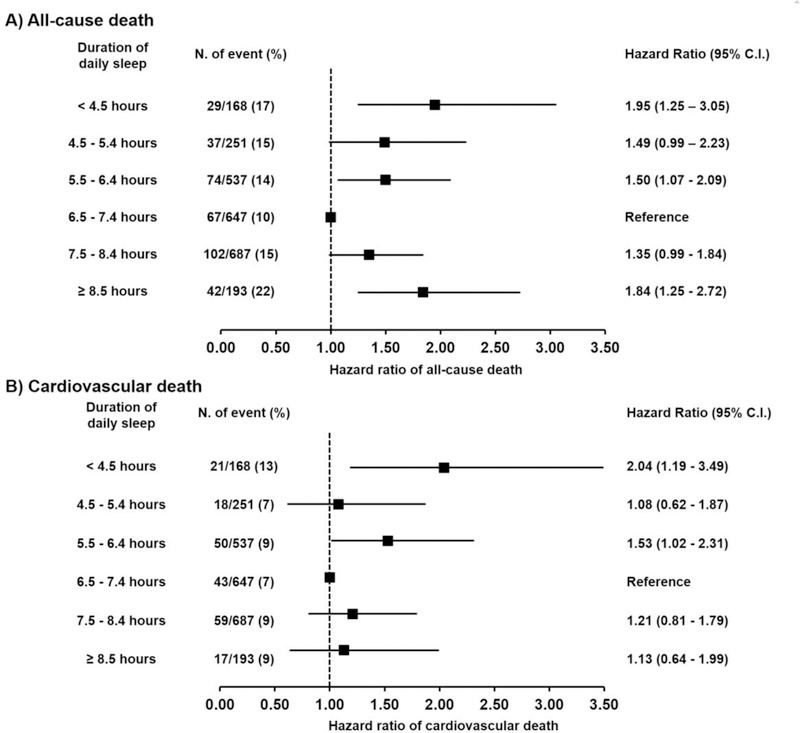
The model is adjusted for age, sex, race, body mass index, hypertension, diabetes, hyperlipidemia, smoking history, prior myocardial infarction, heart failure, acute myocardial infarction at enrollment, revascularization at enrollment, and obstructive coronary artery disease. N = number. C.I. = confidence interval.
Cardiovascular mortality rates were also significantly different among the 3 groups of short (10%), normal (7%), and long (9%) sleep duration in the Kaplan-Meier survival analysis (Log-rank P = 0.035, Figure 1B). Univariate Cox regression model demonstrated that compared to normal sleep, short sleep duration was associated with higher risk of cardiovascular mortality (Table 3, Model 1), which remained significant after multivariate adjustment for the aforementioned covariates (HR 1.48 [1.05–2.09]; Table 3, Model 2) and for CAD severity (Table 3, Model 3). We also calculated cardiovascular mortality rates sequentially with a 1-hour incremental change from the reference (≥ 6.5 hours to < 7.5 hours per day) in the fully adjusted model (Model 3). Cardiovascular mortality rates increased with decreasing duration of sleep compared to those reporting the reference duration of sleep. Specifically, those with extremely short sleep duration (<4.5 hours per day) had an adjusted HR of 2.04, but there was no significant increase in risk with increasing sleep duration (Figure 2B). Treating non-cardiovascular death as a competing risk did not affect the results of cardiovascular mortality and sleep duration.
There was no significant difference in the incident MI rates during follow-up (Table 1). However, those with normal sleep duration had fewer number of total MIs (pre-enrollment, at enrollment, and incident MIs combined) (26 %) than those with long sleep duration (30%) (P= 0.035) while the difference with those with short sleep duration (28%) was statistically insignificant (P=0.28). In addition, there were no significant differences in incident coronary revascularization or stroke events among the 3 groups of sleep duration (Table 1).
In sensitivity analysis, the effect of long sleep duration for all-cause mortality differed significantly by BMI (P-value for interaction = 0.02) and the presence of acute MI at enrollment (P-value for interaction = 0.03) with higher mortality only in those with BMI ≤ 30kg/m2 and without a history of MI (Figure 3; Table 1S). There were no significant interactions with the other examined demographic or clinical variables for the association between short sleep duration and all-cause mortality. Similarly, the association between long sleep duration and cardiovascular mortality differed by BMI (P-value for interaction = 0.02) where long duration of sleep was associated with higher cardiovascular mortality among those with BMI ≤ 30kg/m2, not in those with BMI > 30kg/m2 (Figure 4; Table 2S). Otherwise, there was no other significant interaction with the examined demographic or clinical variables for the relationship between sleep duration and cardiovascular mortality.
Figure 3. Sensitivity analysis of the association between all-cause mortality and daily sleep duration.
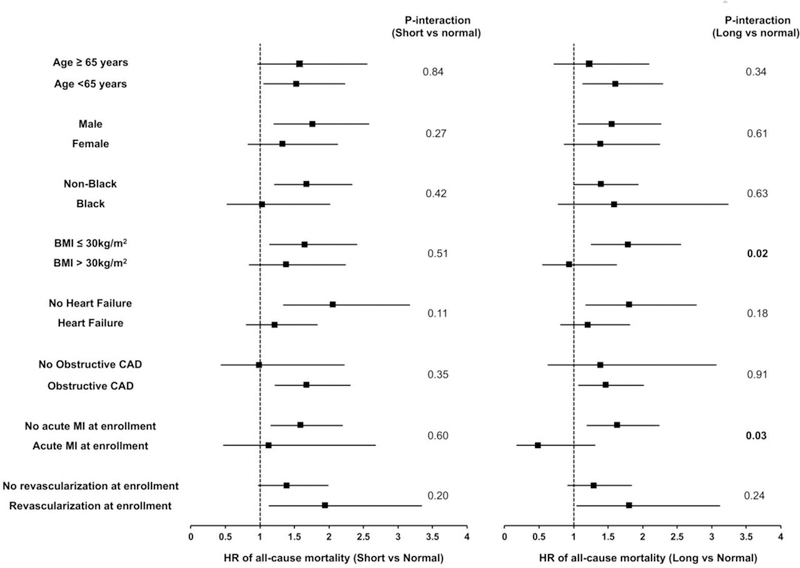
All models are adjusted for age, sex, race, body mass index, hypertension, diabetes, hyperlipidemia, smoking history, prior myocardial infarction, heart failure, acute myocardial infarction at enrollment, revascularization at enrollment, and obstructive coronary artery disease. BMI = body mass index. CAD = coronary artery disease. MI = myocardial infarction.
Figure 4. Sensitivity analysis of the association between cardiovascular mortality and daily sleep duration.
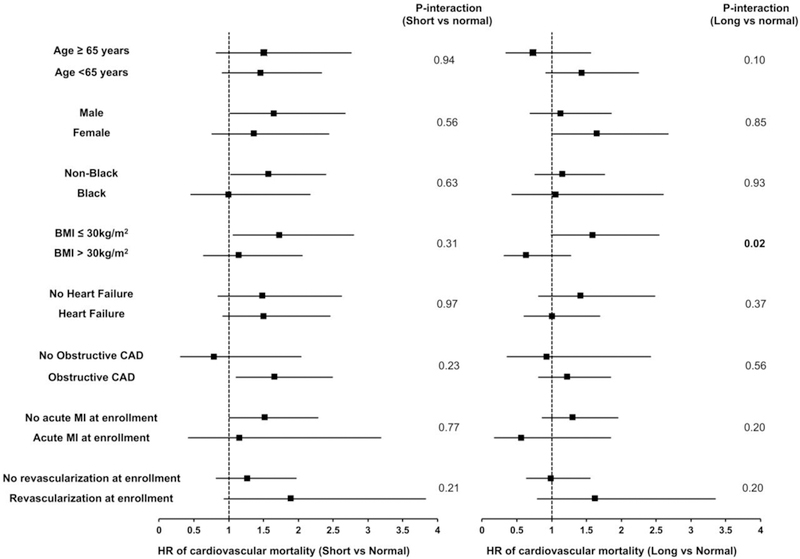
All models are adjusted for age, sex, race, body mass index, hypertension, diabetes, hyperlipidemia, smoking history, prior myocardial infarction, heart failure, acute myocardial infarction at enrollment, revascularization at enrollment, and obstructive coronary artery disease. BMI = body mass index. CAD = coronary artery disease. MI = myocardial infarction.
Finally, although we were underpowered to examine associations between sleep durations and all-cause and cardiovascular mortality in individuals without definitive evidence of CAD, we also tested for interaction between individuals with a Gensini score > 0 when compared to all other individuals and found no evidence of interaction (P-values for both short versus normal and long versus normal, as well as for both all-cause and cardiovascular mortality ranged from 0.29 to 0.67) (data not shown).
DISCUSSION
In a large population of patients with CAD, we observed that compared to those with normal sleep duration (≥ 6.5 to < 7.5 hours), patients with either short or long sleep duration (< 6.5 and ≥ 7.5 hours) had a higher all-cause mortality rate. Moreover, short sleep duration was associated with a higher cardiovascular mortality rate. To our knowledge, this is the first study to investigate the adverse impact of sleep duration in a population with CAD.
Women, Black race and higher BMI were independent predictors of short sleep duration. Racial differences in sleep duration have been reported, 8 likely mediated by genetic and socio-ecological influences.9 While not all studies found that shorter sleep duration occurred more commonly in in women,10,11 the association between higher BMI and shorter sleep duration is well-established, probably due to associated changes in leptin and ghrelin.12 We also found that older individuals and smokers had longer sleep duration. Shorter sleep duration and decreased sleep quality/efficiency has been previously reported in older individuals,13 suggesting that our findings reflect decreased sleep efficiency and longer time in bed rather than longer sleep time per se. In keeping with previous reports, we also found that smoking was associated with longer sleep duration.14,15
In comparison to normal sleep duration (≥ 6.5 to < 7.5 hours), both short (< 6.5 hours) and long (≥ 7.5 hours) sleep duration were associated with a higher all-cause mortality by 56% and 47%, respectively, even after adjustment for demographic and risk factor differences. Our finding confirm previous studies that reported a U-shaped association between sleep duration and higher mortality in population-based, non-clinic cohorts with relatively low prevalence of cardiac disease.16–19 Cardiovascular mortality was also 49% higher and independently associated with short sleep duration. The 19% adjusted increase in cardiovascular mortality rate in those with long sleep duration was not statistically significant, findings similar to some1,2 but not other population-based studies.17 Potential reasons for this discrepancy include statistical power, and probability that the higher cardiovascular mortality with long sleep is mediated by cardiovascular risk factors and demography that was not fully adjusted for in previous studies. As “normal” duration of daily sleep has not been clearly defined in the literature, sleep duration ranging from 6 to 9 hours have been used as a reference range previously.1,18,19 To clarify this further, we also examined mortality risk with 1-hour increments of sleep duration from the reference group (≥6.5 to 7.5 hours) and found a higher mortality rate in those with extremes of both increasing and decreasing sleep duration, with 96% increase in those sleeping ≤4.5 hours and 84% increase in those sleeping ≥8.5 hours.
The mechanisms underlying the association between sleep duration and mortality remain unknown.20,21 Short sleep duration has been associated with cardiometabolic syndrome 22 and sub-clinical cardiovascular disease denoted by coronary calcification,23 carotid intimal thickening,24 and endothelial dysfunction.25 Potential mechanisms for long sleep duration include sleep fragmentation, fatigue, lack of physiological challenge, depression, low socioeconomic status, obstructive sleep apnea, cancer, and respiratory disase.18,21,26,27 Finally, higher cardiovascular mortality with long sleep duration may be mediated through other cardiovascular risk factors, as adjustment for these attenuated the association between long sleep duration and cardiovascular mortality in our cohort.
The association between mortality and sleep duration were relatively similar across different subgroups stratified by demographic and clinical characteristics. However, higher mortality with longer sleep duration was found in non-obese subjects, but not in obese subjects. A strong correlation has been reported between obesity, short sleep duration, and poor sleep quality, while the evidence is not robust for long sleep duration.28 Thus, it is possible that the report of long sleep duration from an obese person may be indicative of relatively better sleep quality and structure, nullifying the true adverse impact of long sleep duration. Secondly, higher risk of all-cause mortality with long sleep duration was only seen among patients without acute MI at enrollment, but not in those with acute MI, a difference that is most likely driven by the large number of subjects without acute MI (92%) in our cohort.
Several limitations of our analysis should be noted. Single center enrollment from patients undergoing cardiac catheterization limits the generalizability. Second, as in previous epidemiologic cohorts, sleep duration was self-reported. However, studies utilizing wrist actigraphy have confirmed close correlation between self-reported and objective measures, although there are also discrepancies in some sub-groups.29 Third, self-reported sleep duration may represent a proxy for other aspects of sleep such as time in bed and sleep quality, which could be vulnerable to biases of reporting individuals. Furthermore, sleep duration was assessed once at the baseline, but there is evidence showing the change in sleep duration having prognostic implications.30 Finally, we did not assess sleep-related breathing disorders, which may impact the duration of sleep reported by this otherwise infirm population.
In conclusion, we demonstrated in a cohort of patients with CAD that both short (< 6.5 hours per day) and long (≥ 7.5 hour per day) sleep duration compared to normal sleep duration (≥ 6.5 to < 7.5 hours) were independently associated with higher all-cause mortality, and mortality from cardiovascular causes was higher in those with short sleep duration. These results extend the findings from the population-based cohorts to those with documented CAD.
Supplementary Material
ACKNOWLEDEGMENT
We would like to thank all patients who volunteered to enroll in the Emory Cardiovascular Biobank for their contributions to our research.
Sources of Funding
AAQ reports research support from NIH (5P01HL101398-02, 1P20HL113451-01, 1R56HL126558-01, 1RF1AG051633-01, R01 NS064162-01, R01 HL89650-01, HL095479-01, 1U10HL110302-01, 1DP3DK094346- 01, 2P01HL086773-06A1) and American Heart Association (Grant No. 0000031288). JHK is supported by American Heart Association (Grant No. 0000031288) and the Abraham J. and Phyllis Katz Foundation (Atlanta, GA). The sponsors of this study had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
Dr. Bliwise serves as a consultant for Merck, Jazz, Ferring, Eisai, and Respicardia, and as a speaker for Merck. None of the other authors report conflict of interest relevant to this article.
References
- 1.Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J 2011;32:1484–1492. [DOI] [PubMed] [Google Scholar]
- 2.Sabanayagam C, Shankar A. Sleep duration and cardiovascular disease: results from the National Health Interview Survey. Sleep 2010;33:1037–1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology 2008;19:838–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gehrman P, Matt GE, Turingan M, Dinh Q, Ancoli-Israel S. Towards an understanding of self-reports of sleep. Journal of Sleep Research 2002;11:229–236. [DOI] [PubMed] [Google Scholar]
- 5.Park S, Cho MJ, Chang SM, Bae JN, Jeon HJ, Cho S-J, Kim B-S, Chung I-W, Ahn JH, Lee HW, Hong JP. Relationships of sleep duration with sociodemographic and health-related factors, psychiatric disorders and sleep disturbances in a community sample of Korean adults. Journal of Sleep Research 2010;19:567–577. [DOI] [PubMed] [Google Scholar]
- 6.Ko Y-A, Hayek S, Sandesara P, Samman Tahhan A, Quyyumi A. Cohort profile: the Emory Cardiovascular Biobank (EmCAB). BMJ open 2017;7:e018753–e018753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gensini GG. Coronary arteriography New York, NY: Futura Pub. Co., 1975. [Google Scholar]
- 8.Whinnery J, Jackson N, Rattanaumpawan P, Grandner MA. Short and Long Sleep Duration Associated with Race/Ethnicity, Sociodemographics, and Socioeconomic Position. Sleep 2014;37:601–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adenekan B, Pandey A, McKenzie S, Zizi F, Casimir GJ, Jean-Louis G. Sleep in America: Role of racial/ethnic differences. Sleep Medicine Reviews 2013;17:255–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van den Berg JF, Miedema HME, Tulen JHM, Hofman A, Neven AK, Tiemeier H. Sex Differences in Subjective and Actigraphic Sleep Measures: A Population-Based Study of Elderly Persons. Sleep 2009;32:1367–1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Polo-Kantola P, Laine A, Kronholm E, Saarinen MM, Rautava P, Aromaa M, Sillanpaa M. Gender differences in actual and preferred nocturnal sleep duration among Finnish employed population. Maturitas 2016;94:77–83. [DOI] [PubMed] [Google Scholar]
- 12.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS medicine 2004;1:e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep 2004;27:1255–1273. [DOI] [PubMed] [Google Scholar]
- 14.Tsou M-T. Association Between Sleep Duration and Health Outcome in Elderly Taiwanese. International Journal of Gerontology 2011;5:200–205. [Google Scholar]
- 15.Schoenborn CA, Adams PF. Sleep duration as a correlate of smoking, alcohol use, leisure-time physical inactivity, and obesity among adults: United States, 2004–2006 National Health Statistics Reports Hyattsville, MD: National Center for Health Statistics, 2008. [Google Scholar]
- 16.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Archives of general psychiatry 2002;59:131–136. [DOI] [PubMed] [Google Scholar]
- 17.Xiao Q, Keadle SK, Hollenbeck AR, Matthews CE. Sleep duration and total and cause-specific mortality in a large US cohort: interrelationships with physical activity, sedentary behavior, and body mass index. Am J Epidemiol 2014;180:997–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res 2009;18:148–158. [DOI] [PubMed] [Google Scholar]
- 19.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep 2010;33:585–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grandner MA, Hale L, Moore M, Patel NP. Mortality associated with short sleep duration: The evidence, the possible mechanisms, and the future. Sleep Med Rev 2010;14:191–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grandner MA, Drummond SP. Who are the long sleepers? Towards an understanding of the mortality relationship. Sleep Med Rev 2007;11:341–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grandner MA, Chakravorty S, Perlis ML, Oliver L, Gurubhagavatula I. Habitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factors. Sleep Med 2014;15:42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.King CR, Knutson KL, Rathouz PJ, Sidney S, Liu K, Lauderdale DS. Short sleep duration and incident coronary artery calcification. Jama 2008;300:2859–2866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sands MR, Lauderdale DS, Liu K, Knutson KL, Matthews KA, Eaton CB, Linkletter CD, Loucks EB. Short sleep duration is associated with carotid intima-media thickness among men in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Stroke 2012;43:2858–2864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hall MH, Mulukutla S, Kline CE, Samuelsson LB, Taylor BJ, Thayer JF, Krafty RT, Frank E, Kupfer DJ. Objective Sleep Duration Is Prospectively Associated With Endothelial Health. Sleep 2017;40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bliwise DL, King AC, Harris RB. Habitual sleep durations and health in a 50–65 year old population. Journal of clinical epidemiology 1994;47:35–41. [DOI] [PubMed] [Google Scholar]
- 27.Yeo Y, Ma SH, Park SK, Chang SH, Shin HR, Kang D, Yoo KY. A prospective cohort study on the relationship of sleep duration with all-cause and disease-specific mortality in the Korean Multi-center Cancer Cohort study. J Prev Med Public Health 2013;46:271–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spiegel K, Tasali E, Leproult R, Van Cauter E. Effects of poor and short sleep on glucose metabolism and obesity risk. Nature Reviews Endocrinology 2009;5:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cespedes EM, Hu FB, Redline S, Rosner B, Alcantara C, Cai J, Hall MH, Loredo JS, Mossavar-Rahmani Y, Ramos AR, Reid KJ, Shah NA, Sotres-Alvarez D, Zee PC, Wang R, Patel SR. Comparison of Self-Reported Sleep Duration With Actigraphy: Results From the Hispanic Community Health Study/Study of Latinos Sueño Ancillary Study. American Journal of Epidemiology 2016;183:561–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferrie JE, Shipley MJ, Cappuccio FP, Brunner E, Miller MA, Kumari M, Marmot MG. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep 2007;30:1659–1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


