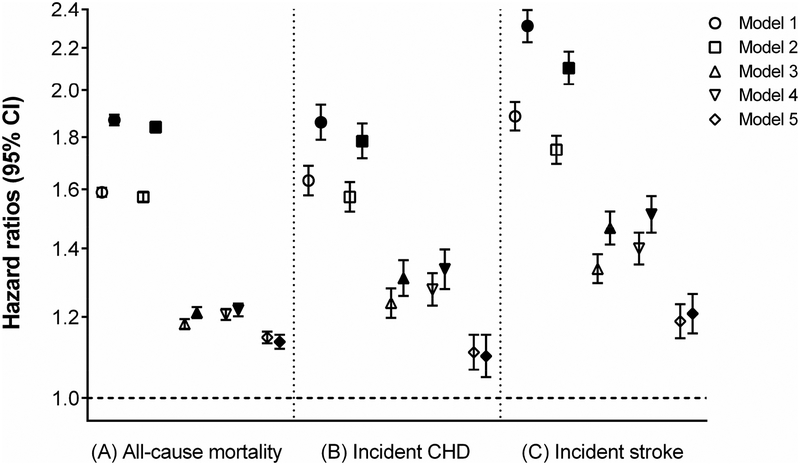
Figure 3.
Hazard ratios and 95% confidence intervals of (A) all-cause mortality, (B) incident CHD, and (C) incident stroke associated with laxative use* in the overall cohort.
*Patients with one (blank symbols) or ≥2 (filled symbols) types of laxatives compared with those with no laxatives (reference). Models represent hazard ratios after adjustment for age (model 1); age plus gender, race, and baseline eGFR (model 2); model 2 variables plus comorbidities (diabetes mellitus, hypertension, coronary heart disease, congestive heart failure, cerebrovascular disease, peripheral arterial disease, peptic ulcer disease, rheumatic disease, malignancy, dementia, Parkinson’s disease, depression, liver disease, chronic lung disease, human immunodeficiency virus/acquired immunodeficiency syndrome, and bowel disorders) and Charlson comorbidity index (model 3); model 3 plus baseline body mass index, systolic blood pressure, diastolic blood pressure, and total cholesterol (model 4); model 4 plus socioeconomic parameters (mean per capita income, marital status, service connectedness, housing stress, low education, low employment, persistent poverty), number of VA healthcare encounters, cumulative length of hospitalization, receipt of influenza vaccination(s), each patient’s VA healthcare region, and use of angiotensin-converting enzyme inhibitors/angiotensin-receptor blockers, calcium channel blockers, diuretics, statins, antidepressants, non-opioid analgesics, opioids, antihistamines, anticholinergics, antiarrhythmics, anticoagulants, antipsychotics, anti-Parkinson drugs, antacids, anticonvulsants, alkylating agents, and oral iron supplements (model 5). CHD = coronary heart disease; CI = confidence interval; eGFR = estimated glomerular filtration rate; VA = veterans affairs.