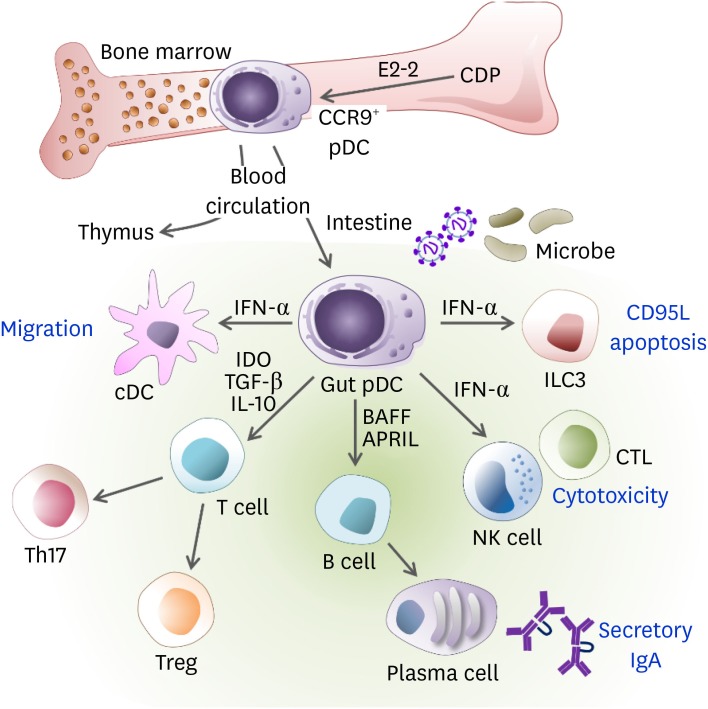
Figure 1. The role of pDCs in gut immunity. The pDCs can be differentiated from CDPs and IL-7R+ lymphoid precursor cells in an E2-2-dependent manner in the BM and distributed via the blood circulation to lymphoid organs such as the thymus, spleen, LNs, and peripheral tissues such as the intestine. The pDCs are recruited to the lamina propria of the small intestine in a CCR9-dependent manner. While pDCs do not migrate from the intestinal periphery to the draining MLNs, they can mobilize the lamina propria cDCs toward MLN via the production of type I IFN. During viral infections, type I IFN produced by gut pDCs induces CD95L expression on ILC3, which reduces IL-22 and then impairs barrier permeability. The pDCs activate NK cells and CD8+ T cells to enhance cytotoxicity via IFN-α. Activated pDCs produce BAFF and APRIL, which induce secretory IgA production from B cells. The pDCs are poor APCs to naïve T cells. However, the gut pDCs conditioned by microbial ligands such as PSA or TLR9 induce the generation of Tregs and Th17 cells via IDO, IL-10, and/or TGF-β.
APRIL, a proliferation-inducing ligand; BAFF, B cell activating factor; CCR9, C-C chemokine receptor type 9.