Figure 3:
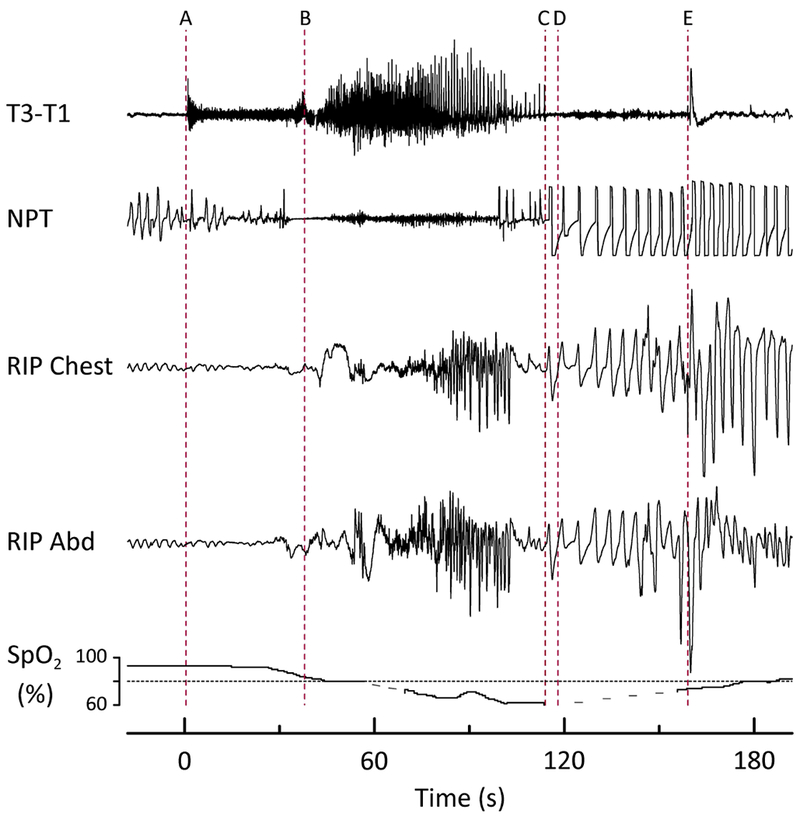
Peri-ictal respiratory depression complicating a focal to bilateral tonic-clonic seizure in a patient who later died of SUDEP Plus. Prior to (A) the patient was drowsy, lying supine in bed. (A) Clinical seizure onset (time 0) characterized by arousal, increased muscle tone, and apnea/hypopnea. (B) Vocalization and beginning of tonic phase. (C) Breathing resumed, initially with an irregular pattern, followed by increasing rate, depth, and regularity. Inspiratory flow limitation was evident on the NPT tracing, and both inspiratory and expiratory upper airway sounds were audible. (D) EEG seizure termination. (E) Patient was turned on to his left side by EMU staff. The duration of peri-ictal hypoventilation totaled 80 seconds, with oxygen saturation falling to a nadir of 61%. Heart rate (beats/min) increased throughout the event: (A) 96, (B) 108, (C) 114, (D) 120, (E) 144. Dashed lines in the pulse oximetry tracing represent data dropout from movement. T3, T1 = left mid- and anterior-temporal leads, respectively, NPT = nasal pressure transducer (airflow), RIP Chest = thoracic (chest) respiratory inductance plethysmography, RIP Abd = abdominal respiratory inductance plethysmography, SpO2 = oxygen saturation.
