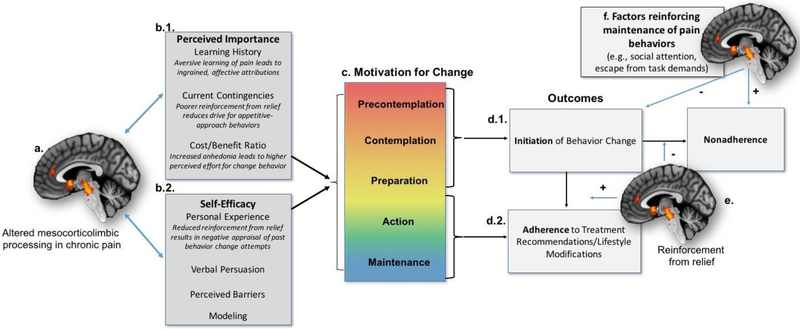
Figure 2.
A Neurobehavioral Model of Pain, Mesocorticolimbic Circuitry, and Treatment Adherence: The present model demonstrates how neurobiological factors might contribute to the Motivational Model for Pain Self-Management. First, previous evidence has demonstrated altered functioning among brain circuitry related to hedonic processing and motivation (i.e., mesocorticolimbic system), reflecting changes in reward and motivational processes in a chronic pain state (a.). As a result, pain self-management strategies might seem less important (b.1.) or the individual might have poorer self-efficacy to implement such strategies (b.2.). Motivation for behavior change/treatment adherence occurs across a gradient based on these factors (c.), and movement through these stages ultimately leads to initiation of self-management strategies (d.1.). If enough reinforcement from pain relief is processed via mesocorticolimbic circuitry (e.), initiation and subsequent adherence are increased. However, if reinforcement from relief is not sufficient, or if competing reinforcers maintain pain behaviors (f), then nonadherence is the primary outcome.