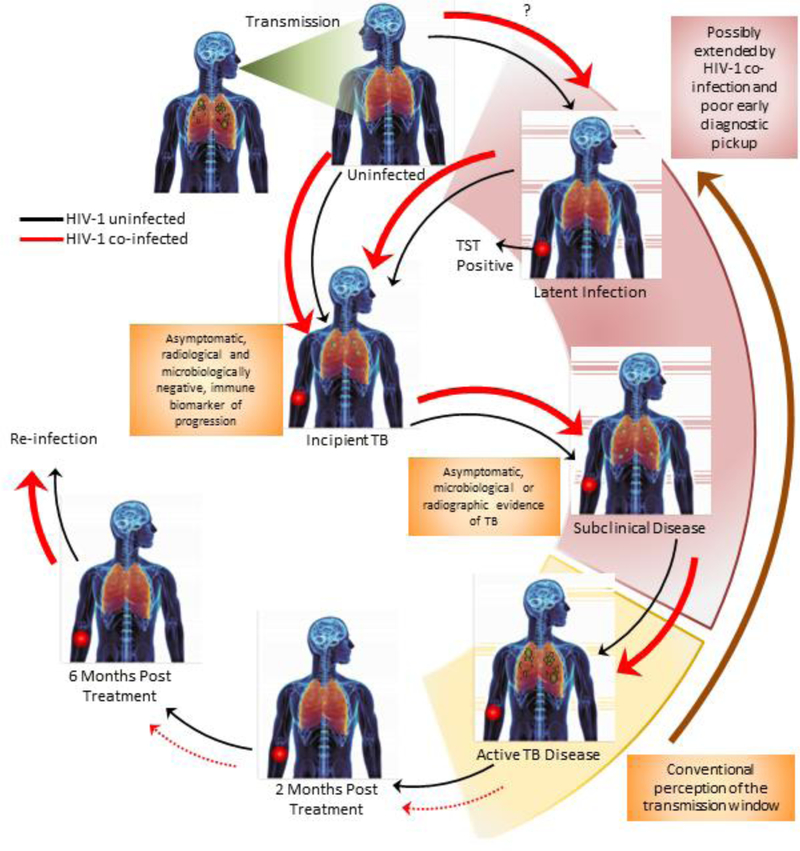
Figure 1. Effects of HIV-1 infection on the progression of tuberculosis disease and the transmission window.
Progression to active, pulmonary tuberculosis disease involves a complex sequence of events that is dependent on initial exposure intensity and the interplay between innate and acquired immunity. Thicker arrows represent an enhanced risk and broken arrows indicate poor progression/reversion to the next/preceding phase. Red arrows indicate the sequence in the case of tuberculosis-HIV infection. Most cases of exposure lead to the development of asymptomatic latent tuberculosis infection (LTBI), which is characterized by an immunological response to mycobacterial antigens (using the tuberculin skin test [TST]). This can progress to incipient tuberculosis, which is defined as asymptomatic disease with no radiological or microbiological signs of disease but can be distinguished from LTBI by an immune biomarker progression from infection to disease. Subclinical disease develops thereafter and is classified as asymptomatic disease associated with either radiological or microbiological confirmation of tuberculosis. In some cases, individuals can spontaneously convert their TST to become uninfected again. HIV co-infection alters the dynamics of immune control and can favour progression to infection, in exposed individuals, and/or progression to incipient tuberculosis. It remains unclear if HIV infection increases the risk of becoming infected with LTBI. The risk of progression to active pulmonary tuberculosis can also be substantively enhanced in the presence of HIV co-infection. Conventionally, the transmission window (shown in yellow) has been assumed to circumscribe the development of granulomatous tuberculosis disease, with a high bacterial load and cavities. HIV co-infection can potentially extend this window (shown in pink) by (I) creating a larger proportion of individuals with incipient/subclinical tuberculosis, within whom the propensity to transmit is as yet unclear (II) creating a larger pool of actively diseased individuals who can transmit and (III) presenting poor treatment outcomes due to extra-pulmonary tuberculosis and drug-drug interactions.