Supplemental Digital Content is available in the text
Keywords: annulus, comparative studies, conservative care, disc herniation, discectomy, indirect comparison, lumbar, meta-analysis, microdiscectomy, network, nonsurgical, reherniation, systematic review
Abstract
Study design:
Systematic review with network meta-analysis.
Objective:
To compare patient outcomes of lumbar discectomy with bone-anchored annular closure (LD + AC), lumbar discectomy (LD), and continuing conservative care (CC) for treatment of lumbar disc herniation refractory to initial conservative management.
Summary of background data:
Several treatment options are available to patients with refractory symptoms of lumbar disc herniation, but their comparative efficacy is unclear.
Methods:
A systematic review was performed to compare efficacy of LD + AC, LD, and CC for treatment of lumbar disc herniation. Outcomes included leg pain, back pain, disability (each reported on a 0–100 scale), reherniation, and reoperation. Data were analyzed using random effects network meta-analysis.
Results:
This review included 14 comparative studies (8 randomized) involving 3947 patients—11 studies of LD versus CC (3232 patients), 3 studies of LD + AC versus LD (715 patients), and no studies of LD + AC versus CC. LD was more effective than CC in reducing leg pain (mean difference [MD] −10, P < .001) and back pain (MD −7, P < .001). LD + AC was more effective than LD in reducing risk of reherniation (odds ratio 0.38, P < .001) and reoperation (odds ratio 0.33, P < .001). There was indirect evidence that LD + AC was more effective than CC in reducing leg pain (MD −25, P = .003), back pain (MD −20, P = .02), and disability (MD −13, P = .02) although the treatment effect was smaller in randomized trials.
Conclusions:
Results of a network meta-analysis show LD is more effective than CC in alleviating symptoms of lumbar disc herniation refractory to initial conservative management. Further, LD + AC lowers risk of reherniation and reoperation versus LD and may improve patient symptoms more than CC.
1. Introduction
Lumbar disc herniation is a localized displacement of disc material beyond the normal margins of the intervertebral disc space[1] and is the most common cause of sciatica, affecting 1% to 5% of the population annually.[2] First-line treatments for sciatica are nonsurgical and may consist of physical therapy, pharmacologic therapy, and/or epidural steroid injection. Acute sciatica symptoms subside in most patients independent of treatment.[3,4] For symptoms that are resistant to initial conservative treatments, continued conservative care or lumbar discectomy to remove the offending herniated disc material may be considered although the question of which treatment is superior has sparked lively debate.[5] Surgery results in faster symptom relief than continued conservative care.[6] However, over longer follow-up, group differences tend to converge but continue to favor surgery.[1]
Results of randomized controlled trials (RCTs) show that over 40% of patients assigned to conservative care undergo surgery within 2 years.[7,8] Among patients undergoing surgery, recurrent disc herniation occurs in 7% to 18% of patients within 2 years,[9–12] which requires a reoperation in nearly 80% of cases.[13] Further, the risk of recurrence and reoperation is more than twofold higher in patients with large versus small annular defects after surgery.[14] Herein lies one of the therapeutic dilemmas of lumbar disc herniation with chronic radicular symptoms—continuation of conservative treatments with incomplete symptom resolution in many cases or undergoing surgery that may be followed by symptomatic reherniation.
A bone-anchored device intended to block the annular defect after lumbar discectomy, which received Conformité Européene (CE) Mark in 2009, has shown promise in reducing the risk of reherniation relative to lumbar discectomy alone.[15–17] However, whether bone-anchored annular closure improves patient outcomes relative to lumbar discectomy alone or conservative care remains unclear. The purpose of this systematic review with network meta-analysis was to compare outcomes of lumbar discectomy with bone-anchored annular closure, lumbar discectomy alone, and continuing conservative care in the treatment of lumbar disc herniation.
2. Materials and methods
2.1. Literature search and study selection
This study was performed according to the PRISMA Extension Statement for Reporting of Systematic Reviews Incorporating Network Meta-analyses of Health Care Interventions[18] and followed methods prospectively defined in a nonregistered protocol. We conducted searches of MEDLINE, EMBASE, and the Cochrane Central Register of Controlled Trials for studies comparing lumbar discectomy with bone-anchored annular closure (LD + AC), lumbar discectomy (LD), or conservative care (CC) for treatment of lumbar disc herniation. Eligible papers were published in English-language journals and reported comparative data for at least one main outcome between 1 and 5 years of follow-up. No date limits were applied to the searches; the final search was completed on May 31, 2018. The details of the MEDLINE search strategy are listed in Supplementary Table 1. The search syntax for other databases was similar but adapted as necessary. We also performed focused searches of the Directory of Open Access Journals, Google Scholar, and reviewed the reference lists of included papers and relevant meta-analyses. Study selection was performed by 2 independent reviewers (LM, DF). Study selection discrepancies between the reviewers were resolved by consensus. Titles and abstracts were initially screened to exclude non-English manuscripts, review articles, commentaries, letters, single-arm case series, case reports, and obvious irrelevant studies. Full-texts of the remaining articles were retrieved and reviewed.
2.2. Outcome measures
Main outcomes of this review were leg pain, back pain, and disability. Leg and back pain data were preferentially extracted from visual analogue scale or numeric rating scale questionnaires. Disability data were preferentially extracted from the Oswestry Disability Index or the Roland-Morris Disability Questionnaire. If data were available at multiple time points within the reporting window, we extracted data at the longest follow-up period. We reported the incidence of symptomatic reherniation and reoperation in studies of LD + AC versus LD, but not in comparisons with CC due to lack of outcome reporting. The rate of crossover from CC to surgery in each study was noted.
2.3. Risk of bias
Risk of bias of the individual studies was assessed using the criteria list advised by the Cochrane Neck and Back Group.[19] This list consists of 13 questions that evaluate selection bias (3 questions), performance bias (4 questions), attrition bias (2 questions), detection bias (2 questions), reporting bias (1 question), and other possible bias sources (1 question). Each item was scored as Yes, No, or Unsure; Yes responses in each study were summed to provide an overall measure of bias risk with higher values representing lower bias risk. We included nonrandomized comparative studies in this review due to the small number of RCTs comparing these treatments.
2.4. Data collection
A database was pilot-tested to ensure consistency with outcomes reported in the literature. Data were independently extracted from eligible articles by the same 2 reviewers using a standardized form. Data extraction discrepancies between the reviewers were resolved by consensus.
2.5. Data analysis
Leg pain, back pain, and disability data were reported as the mean difference (MD) and 95% confidence interval (CI) between treatment groups. All values were transformed to a 0 to 100 scale where higher values represented worse outcomes. The risks of symptomatic reherniation and reoperation with LD + AC versus LD were reported as the odds ratio (OR) and 95% CI. We utilized a random effects model for all analyses with forest plots to illustrate individual study and pooled meta-analysis results. We used the I2 statistic to estimate heterogeneity of outcomes among studies.[20] Significant heterogeneity was defined as a Cochran Q test P < .1 or I2 > 50%. The potential for publication bias was visually examined with funnel plots and, for outcomes reported in at least 10 studies, formally evaluated with Egger regression test.[21] Subgroup analysis investigated the influence of study-level and patient-level covariates on outcomes reported in at least 10 studies.[22] The robustness of study conclusions was evaluated in a sensitivity analysis that assessed outcomes of RCTs only. All tests were 2-sided; an alpha level of .05 was chosen for significance. Statistical analyses were performed using Comprehensive Meta-analysis version 3.3 (Biostat, Englewood, NJ). Indirect comparisons of LD + AC versus CC were performed where LD was used as a common comparator within the network.[23] The treatment effect of the indirect comparison was calculated as the treatment effect of LD + AC versus LD minus the treatment effect of CC versus LD. The variance of the indirect comparison was the sum of variances of the 2 direct comparisons and was used to calculate 95% CIs and P values.
2.6. Ethics and data sharing
Ethical approval and patient consent were not required because this is a systematic review and meta-analysis of previously published studies. The authors agree to make the raw data from this analysis available upon reasonable request.
3. Results
3.1. Study flow
The initial database search retrieved 338 titles and abstracts; hand searching relevant bibliographies identified 4 additional records. After screening records for inclusion criteria, 36 full-text articles were reviewed for eligibility. A listing of the reviewed papers and the reasons for exclusion are provided in Supplementary Table 2. Ultimately, we included 14 comparative studies (8 RCTs) involving 3947 patients undergoing treatment with LD + AC, LD, or CC for symptomatic lumbar disc herniation. The meta-analysis included 11 studies of LD versus CC (7 RCTs) involving 3232 patients and 3 studies of LD + AC versus LD (1 RCT) involving 715 patients. No study directly compared LD + AC to CC. A flow diagram of study identification and selection is shown in Supplementary Flow Diagram. A network graph illustrating the treatment network (i.e., 2 direct comparisons and one indirect comparison) is provided in Supplementary Figure 1.
3.2. Study and patient characteristics
Study and patient characteristics are reported in Table 1. The CC groups included multimodal nonsurgical treatments (7 studies), physical therapy (2 studies), spinal manipulation (1 study), and epidural steroid injections (1 study). Age (typically early 40s) and gender (slight male predominance) of study patients were consistent between groups and among studies. Most comparisons in this review utilized 2-year follow-up data (range 1–5 years). A listing of main outcomes reported in individual studies and the intervals during which they were assessed are listed in Supplementary Table 3. Factors that may have contributed to risk of bias are detailed in Table 2. The main sources of bias were inclusion of nonrandomized studies and lack of blinding.
Table 1.
Comparative studies of lumbar discectomy with bone-anchored annular closure, lumbar discectomy, and conservative care for lumbar disc herniation.

Table 2.
Sources of risk of bias in individual studies∗.

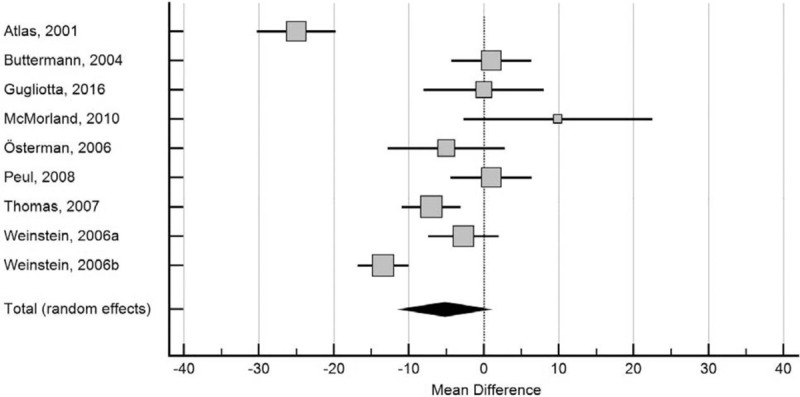
3.3. Leg pain
In studies of LD + AC versus LD, there were greater reductions in leg pain with LD + AC (MD −14; P = .06) but the differences did not achieve statistical significance (Fig. 1). LD was more effective than CC in reducing leg pain (MD −10; P < .001) (Fig. 2). In indirect comparison, leg pain improvement was greater with LD + AC compared with CC (MD −25; 95% CI −41 to −9; P = .003). When evaluating RCTs only, the treatment benefit of LD + AC over CC diminished but remained statistically significant (MD −9; 95% CI −16 to −3; P = .003).
Figure 1.
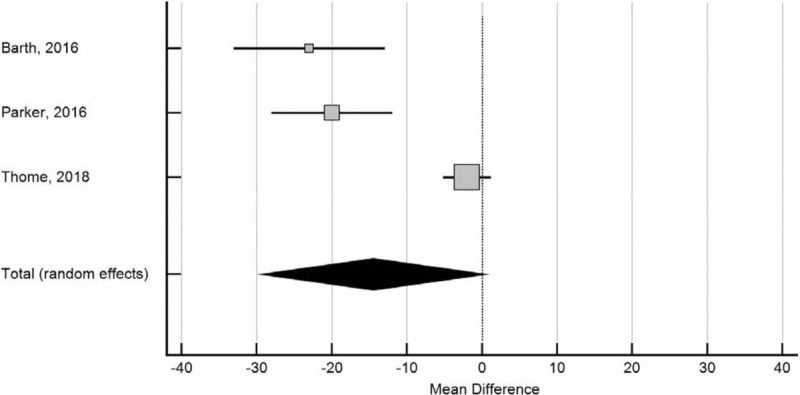
Forest plot of leg pain severity after lumbar discectomy with bone-anchored annular closure versus lumbar discectomy. The mean difference and 95% confidence interval is plotted for each study. The pooled mean difference (diamond apex) and 95% confidence interval (diamond width) is calculated using a random effects model. Positive pooled mean difference suggests greater leg pain with bone-anchored annular closure. Negative pooled mean difference suggests less leg pain with bone-anchored annular closure. Mean difference −14, P = .06. Heterogeneity: I2 = 90%; P < .001.
Figure 2.

Forest plot of leg pain severity after lumbar discectomy or conservative care. The mean difference and 95% confidence interval is plotted for each study. The pooled mean difference (diamond apex) and 95% confidence interval (diamond width) is calculated using a random effects model. Positive pooled mean difference suggests greater leg pain with lumbar discectomy. Negative pooled mean difference suggests less leg pain with lumbar discectomy. Mean difference −10, P < .001. Heterogeneity: I2 = 90%; P < .001.
3.4. Back pain
Back pain reductions with LD + AC versus LD were not statistically significant (MD −13; P = .11) (Fig. 3). LD resulted in greater reductions in back pain relative to CC (MD −7; P = .02) (Fig. 4). In indirect comparison, back pain reduction was 20 points greater with LD + AC versus CC (95% CI −38 to −3; P = .03); in RCTs, the benefit of LD + AC over CC was 7 points (95% CI −13 to −1; P = .04).
Figure 3.
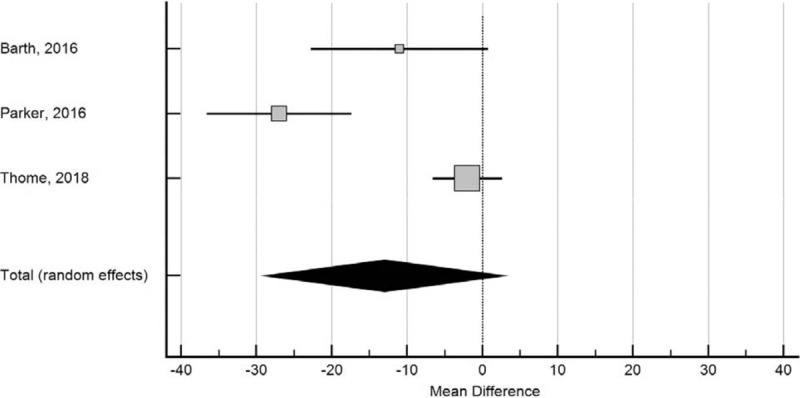
Forest plot of back pain severity after lumbar discectomy with bone-anchored annular closure versus lumbar discectomy. The mean difference and 95% confidence interval is plotted for each study. The pooled mean difference (diamond apex) and 95% confidence interval (diamond width) is calculated using a random effects model. Positive pooled mean difference suggests greater back pain with bone-anchored annular closure. Negative pooled mean difference suggests less back pain with bone-anchored annular closure. Mean difference −13, P = .11. Heterogeneity: I2 = 91%; P < .001.
Figure 4.

Forest plot of back pain severity after lumbar discectomy or conservative care. The mean difference and 95% confidence interval is plotted for each study. The pooled mean difference (diamond apex) and 95% confidence interval (diamond width) is calculated using a random effects model. Positive pooled mean difference suggests greater back pain with lumbar discectomy. Negative pooled mean difference suggests less back pain with lumbar discectomy. Mean difference −7, P = .02. Heterogeneity: I2 = 74%; P < .001.
3.5. Disability
Patients treated with LD + AC had less disability than those treated with LD (MD −8; P = .09) (Fig. 5) as did those treated with LD relative to CC (MD −5; P = .09) (Fig. 6), but outcomes did not achieve statistical significance. In indirect comparison, disability levels were lower with LD + AC versus CC (MD −13; 95% CI −24 to −2; P = .02). However, there was no difference between LD + AC and CC when evaluating RCTs only (MD −2; 95% CI −6 to 2; P = .24).
Figure 5.
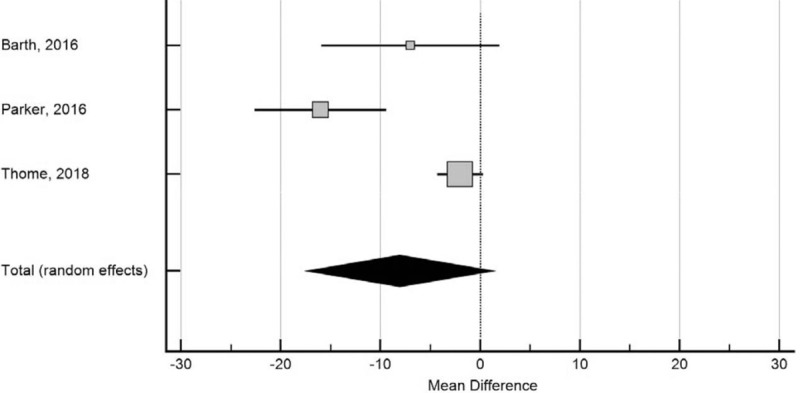
Forest plot of disability after lumbar discectomy with bone-anchored annular closure versus lumbar discectomy. The mean difference and 95% confidence interval is plotted for each study. The pooled mean difference (diamond apex) and 95% confidence interval (diamond width) is calculated using a random effects model. Positive pooled mean difference suggests greater disability with bone-anchored annular closure. Negative pooled mean difference suggests less disability with bone-anchored annular closure. Mean difference −8, P = .09. Heterogeneity: I2 = 87%; P < .001.
Figure 6.
Forest plot of disability after lumbar discectomy or conservative care. The mean difference and 95% confidence interval is plotted for each study. The pooled mean difference (diamond apex) and 95% confidence interval (diamond width) is calculated using a random effects model. Positive pooled mean difference suggests greater disability with lumbar discectomy. Negative pooled mean difference suggests less disability with lumbar discectomy. Mean difference −5, P = .09. Heterogeneity: I2 = 91%; P < .001.
3.6. Symptomatic reherniation and reoperations
Treatment with LD + AC was associated with a considerably lower risk of symptomatic reherniation (OR 0.38; 95% CI 0.24–0.61, P < .001) and associated reoperation (OR 0.33; 95% CI 0.18–0.60, P < .001) compared to LD. Among CC studies, the median rate of crossover to surgery was 39%.
3.7. Meta-analysis diagnostics and subgroup analysis
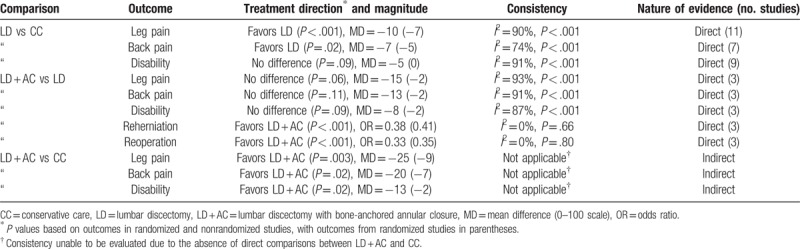
Publication bias was not evident for leg pain in comparisons of LD to CC (Egger P = .40). Publication bias was not formally evaluated among other combinations of outcomes and comparisons owing to a small number of studies, but visual assessment of the funnel plots did not indicate asymmetry. For comparisons of LD + AC to LD, significant heterogeneity was identified for leg pain (I2 = 90%; P < .001), back pain (I2 = 91%; P < .001), and disability (I2 = 87%; P < .001). For comparisons of LD to CC, significant heterogeneity was identified for leg pain (I2 = 61%; P < .01) and disability (I2 = 82%; P < .001), but not back pain (I2 = 0%; P = .52). Heterogeneity was not evident for reherniation and reoperation comparing LD + AC versus LD (both I2 = 0%). In subgroup analysis, the benefit of LD over CC in reducing leg pain was consistent among most subgroups. While some variability in the magnitude of treatment effect was observed, no covariate significantly explained this variability (Table 3). A summary of evidence, including the direction, magnitude, and nature of treatment effects, is provided in Table 4.
Table 3.
Post hoc subgroup analysis of leg pain severity after lumbar discectomy or conservative care for lumbar disc herniation.

Table 4.
Summary of evidence for lumbar discectomy with bone-anchored annular closure, lumbar discectomy, and conservative care for lumbar disc herniation.
4. Discussion
Among patients with refractory radicular symptoms due to lumbar disc herniation, the findings of this systematic review with network meta-analysis show that LD decreases leg and back pain more than CC. Further, LD + AC lowers the risk of symptom recurrence and reoperation compared to LD and may decrease leg pain, back pain, and disability to a greater degree than CC. This is the first known study to report the comparative efficacy of these 3 treatment options for patients with lumbar disc herniation.
Lumbar discectomy was more effective than CC in reducing leg and back pain, but not disability. These results were consistent among all studies as well as in RCTs only. Although the results of the subgroup analysis of leg pain severity were likely underpowered, the potential for factors such as crossover to surgery and different CC regimens to influence outcomes must be acknowledged. Importantly, the benefit of LD over CC in reducing leg pain was maintained among most subgroups analyzed and the observed heterogeneity influenced the magnitude of benefit with LD, but not whether a benefit was realized. While the large proportion of patients who crossed over from CC to LD among the include studies complicates interpretation of these findings, this finding suggests that the treatment benefit of LD relative to CC may be underestimated.
Supplemental implantation with a bone-anchored annular closure device reduced the risk for symptom recurrence and reoperation and provided minor improvements in leg pain, back pain, or disability relative to LD. A plausible explanation for these results may relate to the timing of pain and disability assessments in the studies. Patients who undergo a reoperation for recurrence in the interim between scheduled follow-up visits may report favorable results at subsequent visits that are mainly attributable to the reoperation. To the extent that reoperation rates are higher with LD than with LD + AC, this may bias patient-reported outcomes at follow-up visits to favor LD. In a RCT of LD + AC versus LD,[17] leg pain severity (0–100 scale) at the 2-year follow-up visit was comparable between groups (12 vs 14; P = .33). However, when patients with recurrence were treated as failures in the analysis, leg pain severity was lower with LD + AC (19 vs 29; P < .001)[24] with the treatment benefit approximating that reported in the current meta-analysis. Overall, these results are suggestive of a modest benefit in pain and disability with LD + AC versus LD that is partially mediated by the lower recurrence rates with LD + AC.
Despite the absence of head-to-head studies of LD + AC versus CC, utilization of network meta-analysis facilitated indirect comparison of these groups. In frequent situations where studies have not been performed to directly compare all possible treatments for a medical condition, patient care decisions must often rely on conclusions derived from indirect comparisons. Relative to CC, LD + AC significantly lowered leg pain by 25 points (9 points in RCTs) and back pain by 20 points (7 points in RCTs). While disability outcomes favored LD + AC by 13 points, there was no statistical difference between groups among RCTs. In the absence of comparative studies, these initial results represent the best available evidence and suggest that LD + AC may reduce pain relative to CC in the treatment of lumbar disc herniation.
There are several factors pertaining to the characteristics of included studies that warrant further discussion. First, in pairwise meta-analyses, heterogeneity of outcomes among studies was frequently observed, which confounded data interpretation and was not explained in subgroup analysis. We cannot rule out the possibility that factors such as study quality, randomization, and crossover to surgery influenced results since the subgroup analysis was likely underpowered. Second, inclusion of data from randomized and nonrandomized studies may have introduced bias into the results. While the meta-analysis conclusions were largely unchanged when evaluating RCTs only, the treatment benefit of LD versus CC—and consequently that of LD + AC versus CC—was reduced among RCTs. Third, most patients included in comparative studies of LD + AC versus LD had a large postsurgical annular defect (≥6 mm width), which has an uncertain impact on comparisons of patient-reported outcomes within the network. While large postsurgical annular defects are a known risk factor for symptom recurrence and reoperation,[14] there is no evidence that the size of the postsurgical defect is associated with the magnitude of postoperative pain and disability. Evidence from this review supports the efficacy of LD + AC in patients with large annular defects who are inherently at higher risk of recurrence, but the utility of LD + AC in smaller annular defects is unknown. Fourth, the comparisons of LD + AC to CC wee inherently observational since conclusions were derived exclusively from indirect comparisons. Consequently, several key assumptions inherent in network meta-analyses (e.g., transitivity, consistency) could not be formally evaluated. Despite these limitations, the results presented here represent the best available evidence on the efficacy of LD + AC versus CC in the treatment of lumbar disc herniation.
5. Conclusion
Results of a network meta-analysis suggest LD is more effective than CC in alleviating symptoms of lumbar disc herniation refractory to initial conservative management. Further, LD + AC lowers risk of reherniation and reoperation versus LD and may improve patient symptoms more than CC.
Acknowledgments
We thank David Fay, PhD for assistance with literature review and Teresa Nelson, MS for assisting with statistical analysis and review. The authors had no writing assistance in the preparation of this manuscript.
Author contributions
Conceptualization: Mark P. Arts, Adisa Kuršumović, Larry Edwin Miller, Jasper F.C. Wolfs, Jason M. Perrin, Erik Van de Kelft, Volkmar Heidecke.
Formal analysis: Larry Edwin Miller.
Writing – original draft: Larry Edwin Miller.
Writing – review & editing: Mark P. Arts, Adisa Kuršumović, Jasper F.C. Wolfs, Jason M. Perrin, Erik Van de Kelft, Volkmar Heidecke.
Larry Edwin Miller orcid: 0000-0003-1594-1885.
Supplementary Material
Footnotes
Abbreviations: CC = conservative care, CE = Conformité Européene, CI = confidence interval, LD = lumbar discectomy, LD + AC = lumbar discectomy with bone-anchored annular closure, MD = mean difference, OR = odds ratio, RCT = randomized controlled trial.
Funding: This research was supported by Intrinsic Therapeutics (Woburn, MA, USA).
Conflicts of interest: Mart Arts reports consultancy with Intrinsic Therapeutics; other from Zimmer-Biomet, EIT, and Silony, outside the submitted work; and receipt of royalties from EIT. Adisa Kuršumović reports consultancy with Intrinsic Therapeutics. Larry Miller reports consultancy with Intrinsic Therapeutics. Jasper Wolfs reports nonfinancial support from Intrinsic Therapeutics; other from Zimmer Biomet, Safe Orthopaedics, Silony, and EIT, outside the submitted work. Jason Perrin has nothing to disclose. Erik Van de Kelft reports consultancy with Intrinsic Therapeutics. Volkmar Heidecke has nothing to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Kreiner DS, Hwang SW, Easa JE, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J 2014;14:180–91. [DOI] [PubMed] [Google Scholar]
- [2].Frymoyer JW. Back pain and sciatica. N Engl J Med 1988;318:291–300. [DOI] [PubMed] [Google Scholar]
- [3].Vroomen PC, de Krom MC, Knottnerus JA. Predicting the outcome of sciatica at short-term follow-up. Br J Gen Pract 2002;52:119–23. [PMC free article] [PubMed] [Google Scholar]
- [4].Vroomen PC, de Krom MC, Wilmink JT, et al. Lack of effectiveness of bed rest for sciatica. N Engl J Med 1999;340:418–23. [DOI] [PubMed] [Google Scholar]
- [5].Ramaswami R, Ghogawala Z, Weinstein JN. Management of sciatica. N Engl J Med 2017;376:1175–7. [DOI] [PubMed] [Google Scholar]
- [6].Peul WC, van Houwelingen HC, van den Hout WB, et al. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med 2007;356:2245–56. [DOI] [PubMed] [Google Scholar]
- [7].Peul WC, van den Hout WB, Brand R, et al. Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation: two year results of a randomised controlled trial. BMJ 2008;336:1355–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA 2006;296:2441–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Carragee EJ, Spinnickie AO, Alamin TF, et al. A prospective controlled study of limited versus subtotal posterior discectomy: short-term outcomes in patients with herniated lumbar intervertebral discs and large posterior anular defect. Spine (Phila Pa 1976) 2006;31:653–7. [DOI] [PubMed] [Google Scholar]
- [10].Ambrossi GL, McGirt MJ, Sciubba DM, et al. Recurrent lumbar disc herniation after single-level lumbar discectomy: incidence and health care cost analysis. Neurosurgery 2009;65:574–8. discussion 578. [DOI] [PubMed] [Google Scholar]
- [11].McGirt MJ, Eustacchio S, Varga P, et al. A prospective cohort study of close interval computed tomography and magnetic resonance imaging after primary lumbar discectomy: factors associated with recurrent disc herniation and disc height loss. Spine (Phila Pa 1976) 2009;34:2044–51. [DOI] [PubMed] [Google Scholar]
- [12].Arts MP, Brand R, van den Akker ME, et al. Tubular diskectomy vs conventional microdiskectomy for the treatment of lumbar disk herniation: 2-year results of a double-blind randomized controlled trial. Neurosurgery 2011;69:135–44. discussion 144. [DOI] [PubMed] [Google Scholar]
- [13].Ran J, Hu Y, Zheng Z, et al. Comparison of discectomy versus sequestrectomy in lumbar disc herniation: a meta-analysis of comparative studies. PLoS ONE 2015;10:e0121816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Miller LE, McGirt MJ, Garfin SR, et al. Association of annular defect width after lumbar discectomy with risk of symptom recurrence and reoperation: systematic review and meta-analysis of comparative studies. Spine (Phila Pa 1976) 2018;43:E308–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Barth M, Fontana J, Thome C, et al. Occurrence of discal and non-discal changes after sequestrectomy alone versus sequestrectomy and implantation of an anulus closure device. J Clin Neurosci 2016;34:288–93. [DOI] [PubMed] [Google Scholar]
- [16].Parker SL, Grahovac G, Vukas D, et al. Effect of an annular closure device (barricaid) on same-level recurrent disk herniation and disk height loss after primary lumbar discectomy: two-year results of a multicenter prospective cohort study. Clin Spine Surg 2016;29:454–60. [DOI] [PubMed] [Google Scholar]
- [17].Thome C, Klassen PD, Bouma GJ, et al. Annular closure in lumbar microdiskectomy for prevention of reherniation: a randomized clinical trial. Spine J 2018. [DOI] [PubMed] [Google Scholar]
- [18].Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 2015;162:777–84. [DOI] [PubMed] [Google Scholar]
- [19].Furlan AD, Malmivaara A, Chou R, et al. 2015 Updated method guideline for systematic reviews in the Cochrane Back and Neck Group. Spine (Phila Pa 1976) 2015;40:1660–73. [DOI] [PubMed] [Google Scholar]
- [20].Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0. The Cochrane Collaboration 2011. [Google Scholar]
- [23].Bucher HC, Guyatt GH, Griffith LE, et al. The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. J Clin Epidemiol 1997;50:683–91. [DOI] [PubMed] [Google Scholar]
- [24].Miller LE. Challenges in the analysis of longitudinal pain data: practical lessons from a randomized trial of annular closure in lumbar disc surgery. J Pain Res 2018;In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


