Abstract
Objective:
To contrast the effects and complications in unilateral and bilateral percutaneous vertebroplasty (PVP) for osteoporotic vertebral compression fractures in elderly patients.
Methods:
Multiple databases were adopted to search relevant studies, and the articles eventually satisfied the criteria were included. All the meta-analyses were conducted with the Review Manager 5.2. To estimate the quality of each article, risk of bias table was performed.
Results:
Finally, 627 patients were enrolled in 9 studies and ultimately met the eligibility criteria. The unilateral and bilateral surgical samples were 314 and 313, respectively. The meta-analysis showed no significant difference in Visual Analog Scale/Score (VAS) (MD = −0.05, 95% confidence interval [CI] [−0.24, 0.13], P = .57), Oswestry Disability Index (ODI) score (MD = 0.03, 95% CI [−0.57, 0.62], P = .93) and cement leakage (OR = 1.00, 95% CI [0.67, 1.50], P = 1.00) between unilateral group and bilateral group. The surgery time of unilateral PVP is much less than that of bilateral PVP (MD = −8.42, 95% CI [−13.17, −3.66], P = .0005). Patients with bilateral PVP surgery have been injected more cement than patients with a unilateral surgery (MD = −2.56, 95% CI [−2.79, −2.33], P <.00001).
Conclusion
This study demonstrated unipedicular approach is the preferred surgical technique for treatment of osteoporotic vertebral fracture (OVF) compared with bilateral PVP since unipedicular approach injects less cement and cost less surgery time.
Keywords: elderly, osteoporotic vertebral compression fractures, percutaneous vertebroplasty
1. Introduction
Osteoporosis is a skeletal system disease resulting in increased bone brittleness and easy to be fractured. Fractures usually occur in the chest and lumbar segments of the hip and spine.[1–3] Osteoporotic vertebral fracture (OVF) is a common fracture in the elderly. OVF suffers from severe back pain, pulmonary dysfunction, spinal deformity, abdominal limitation, impaired mobility, chest contents, and clinical depression, which have an impact on the quality of life of patients.[4,5] Several studies suggested that population distribution of OVF patients is 8% in women and 27% in men.
The pain caused by osteoporotic vertebral compression fractures in the elderly significantly reduced the quality of life in old patients. OVF has traditionally been treated with enough rest, physical therapy and antiresorptive medications.[6,7] Patients are often with multiple system complications, and conservative treatment requires stay in bed for a long time. It might further aggravate osteoporosis, and induce complications such as respiratory and urinary infection. Since Galibert reported percutaneous vertebroplasty (PVP) for the treatment of vertebral hemangiomas in 1987, PVP has been widely used in the clinical treatment of osteoporotic vertebral compression fractures.[8,9] The procedure involves inserting a needle into a fractured vertebra and injecting polymethylmethacrylate (PMMA) or other bone cement into the fractured vertebra under radiation control. After injection of cement, the pain pathway in the surrounding tissues seems to be altered by various stimuli.
In the past decades, PVP is a safe and effective treatment. Both unilateral and bipedal operations had satisfactory results, consistent with those before surgery. However, studies have shown that compared with bilateral PVP, unilateral PVP surgery has a better therapeutic effect.[10]
The aim of this meta-analysis is to contrast the safety and effectiveness of unilateral and bilateral PVP for treatment in osteoporotic vertebral compression fractures. Because of the inconsistent results of the 2 treatments, a meta-analysis is necessary to verify the differences in the efficacy and complication rates of unilateral and bilateral PVP surgery.
2. Materials and methods
Ethical approval was not necessary because this is a meta-analysis. All data were available on the internet.
2.1. Search strategy
To search out all of the relevant published citations, multiple electronic databases including Pubmed, Springer, EMBASE, EMBASE, OVID, and China Journal Full-text Database were applied, without language restrictions. To maximize the search accuracy, the following MeSH terms were assembled with the Boolean operator “AND”:
-
(1)
osteoporotic vertebral compression fractures or OVF;
-
(2)
percutaneous vertebroplasty or vertebroplasty or PVP or VP;
-
(3)
unilateral or bilateral or unipedicular or bipedicular related articles with all publication statuses (published, unpublished, in press, and in progress) published from January 2000 to January 2018 were systematically searched and reviewed.
Two authors in our team searched the literature independently and examined the reference lists to obtain the additional relevant studies that not identified.
2.2. Citation selection
The other 2 authors independently and carefully chose the citations in the process. They sifted through the titles and abstracts of the articles identified by the proposed electronic search criteria, and then obtained the full text of the studies that might meet the criteria and reviewed them to see if the studies might be relevant.
The relevant research in this study must meet the following criteria:
-
(1)
A randomized control trial or controlled clinical trial study;
-
(2)
Sample size more than 10;
-
(3)
Adult patients with OVFs;
-
(4)
Comparison between unilateral and bilateral PVP;
-
(5)
Available Exclusion Criteria
Exclusion criteria:
-
(1)
Non-randomized studies;
-
(2)
Studies lacking outcome measures or comparable results;
-
(3)
Studies on other diseases other than OVF.
After reading the full text of the articles, the characteristics from each study using a standard data extraction were extracted: the first author's name, year of publication, nation, age range of patients, sex distribution (male/female), sample size (asthmatics/cough), follow-up period, and other parameters.
2.3. Data extraction
The 2 reviewers read the full text independently and extracted features from each study using the Excel 2010 standard data extraction table. Data extracted from these studies included the first author's name, year of publication, year of onset, average age of patients, sample size (unilateral/bilateral), gender distribution (male/female), outcome measurements, and follow-up time. Results Measurements, including Visual Analog Scale/Score (VAS), Oswestry Disability Index (ODI), operative time, cement injection volume, and cement leakage results, were collected to estimate differences between unilateral and bilateral PVP.
2.4. Statistical analysis
The meta-analyses were conducted with the software Review Manager 5.2 (The Cochrane Collaboration, 2011) to compare the clinical effects between unilateral and bilateral PVP in elderly patients among selected articles. As continuous outcomes, standard mean difference (SMD) with 95% confidence intervals (CIs) was performed. In discontinuous outcomes, odds ratio (OR) with 95% CIs were conducted. A P value <.05 was considered to be statistically significant. The heterogeneities in this study were assessed using the I2 index. We chose the random-effect model when the heterogeneity I2 statistic >50%, otherwise the fixed-effect model was applied.
In addition, the quality of the studies was assessed with sensitivity analysis and bias analysis. Risk of bias table of the included studies was independently assessed according to the Cochrane Handbook for Systematic Reviews of Interventions by 2 members of our team. Also if any occurrence of poor agreement and no consensus could be achieved, a third investigator was the adjudicator.
3. Results
3.1. Search results
After preliminary screening, a total of 1030 titles and abstracts were preliminarily reviewed in these electronic databases, 9 of which eventually met the eligibility criteria. Other 1021 articles excluded duplicate, unrelated studies, inappropriate data, inappropriate comparisons, reviews, no controls, other diseases, other operations or incomplete articles. The flow chart reflecting the search process can be seen in Figure 1, including the reasons for exclusion.
Figure 1.
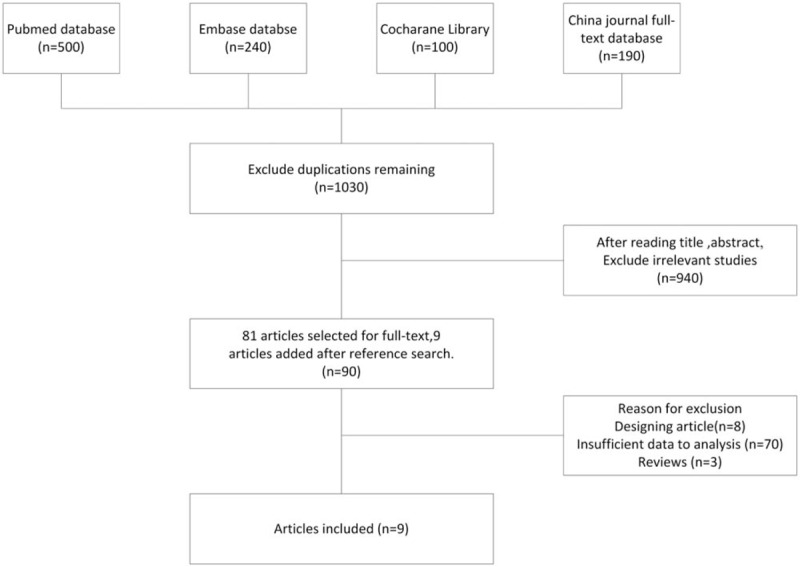
Flow diagram of the study selection.
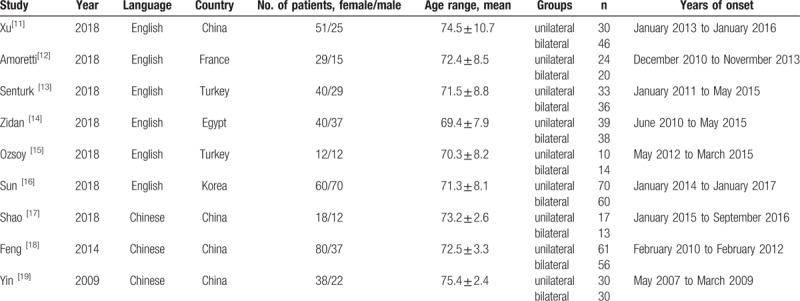
3.2. Characteristics of included studies
Table 1 provides detailed characteristics of the study. The table lists the name of the first author, the year of publication, the year of onset, the average age of the patient, sample size (unilateral/bilateral), gender distribution (male/female), outcome measurements, and follow-up time. All these articles were published from 2000 to 2018. A total of 627 patients were included in 9 studies, of which 314 were unilateral surgical specimens and 313 were bilateral surgical samples. The sample size is between 30 and 130. All patients were elderly patients.
Table 1.
Characteristics of studies included in the meta-analysis.
3.3. Quality assessment
The bias table in the Review Manager 5.2 Tutorial was used to evaluate the risk of each study by applying the criteria of evaluating design-related bias. The quality of included studies was evaluated by the risk of bias table, and the evaluation in this study was shown in Figure 2. In the 9 articles, 1 trial showed problem in patient selection and 1 showed problem in allocation bias. Overall, all the trails were out of risk.
Figure 2.
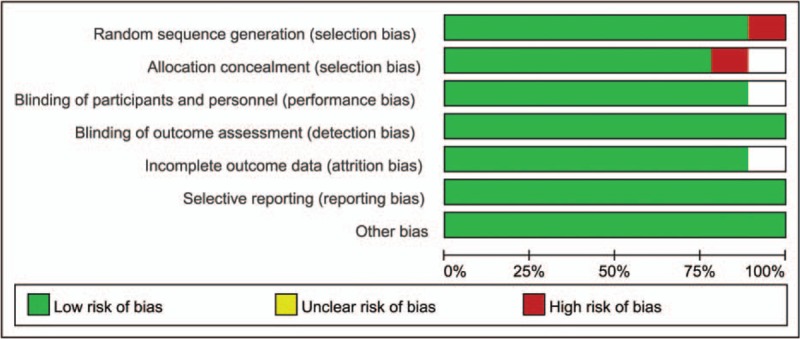
Assessment of the quality of the included studies: low risk of bias (green hexagons), unclear risk of bias (blank hexagons), and high risk of bias (red hexagons).
3.4. Meta-analysis about operating time
Nine included studies involve in operating time for unilateral and bilateral PVP. The forest plot for the operating time in unilateral and bilateral PVP groups was shown in Figure 3. The meta-analysis suggested that there was significant difference of the operating time in unilateral group and bilateral group (MD = −8.42, 95% CI [−13.17, −3.66], P = .0005; P for heterogeneity <.00001, I2 = 98%). The operating time in bilateral group was more than that in unilateral group.
Figure 3.
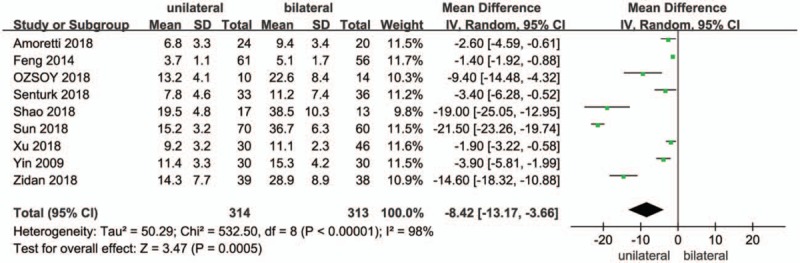
A forest plot for the operating time in unilateral and bilateral PVP groups. PVP = percutaneous vertebroplasty.
3.5. Meta-analysis about VAS score
All studies involved in the VAS score between unilateral and bilateral PVP groups. As shown in the forest plot (Fig. 4). The result of meta-analysis showed that the difference of VAS score between unilateral and bilateral PVP was not significant (MD = −0.05, 95% CI [−0.24, 0.13], P = .57; P for heterogeneity = .007, I2 = 44%).
Figure 4.
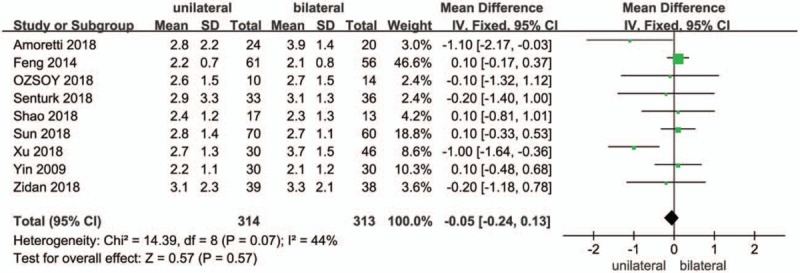
A forest plot for the VAS score in unilateral and bilateral PVP groups. PVP = percutaneous vertebroplasty, VAS = Visual Analog Scale/Score.
3.6. Meta-analysis about the ODI score
There are 9 studies about the comparison of ODI score. The forest plot for the ODI score was shown in Figure 5. All these 9 studies showed no significant differences of ODI score between unilateral and bilateral PVP (MD = 0.03, 95% CI [−0.57, 0.62], P = .93; P for heterogeneity = .73, I2 = 0%).
Figure 5.
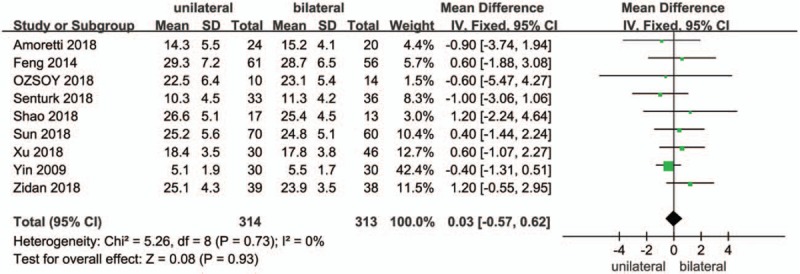
A forest plot for the ODI score in unilateral and bilateral PVP groups. ODI = Oswestry Disability Index, PVP = percutaneous vertebroplasty.
3.7. Meta-analysis about the injected cement volume
All the 9 studies on the cement volume injected in PVP have shown the statistically significant difference between unilateral and bilateral PVP. The result of meta-analysis indicated that in bilateral PVP surgery, patients with OVF have been injected more cement than patients in a unilateral surgery (MD = −2.56, 95% CI [−2.79, −2.33], P <.00001; P for heterogeneity = 0.65, I2 = 0%). The forest plot for the injected cement volume was shown in Figure 6.
Figure 6.
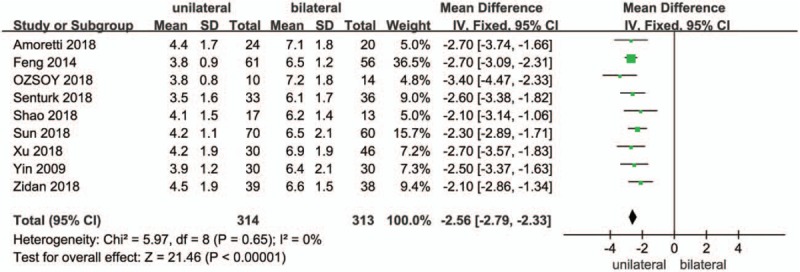
A forest plot for the injected cement volume in unilateral and bilateral PVP groups. PVP = percutaneous vertebroplasty.
3.8. Meta-analysis about the cement leakage
There are 9 studies are about the cement leakage in unilateral and bilateral PVP groups. The result of meta-analysis showed that no difference of cement leakage between unilateral and bilateral PVP was not significant (OR = 1.00, 95% CI [0.67, 1.50], P = 1.00; P for heterogeneity = .98, I2 = 0%) (Fig. 7).
Figure 7.
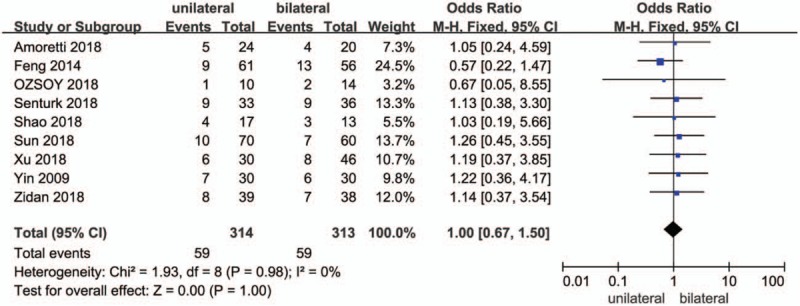
A forest plot for the cement leakage in unilateral and bilateral PVP groups. PVP = percutaneous vertebroplasty.
3.9. Sensitivity analysis
According to the results of meta-analyses, the heterogeneities of operating time was very high (I2 > = 95%). As shown in Figure 8, the high heterogeneity of operating time was probably attributed to the different results in each study. When the article of Sun in 2018 was excluded, I2 changed from 98% to 92%.
Figure 8.
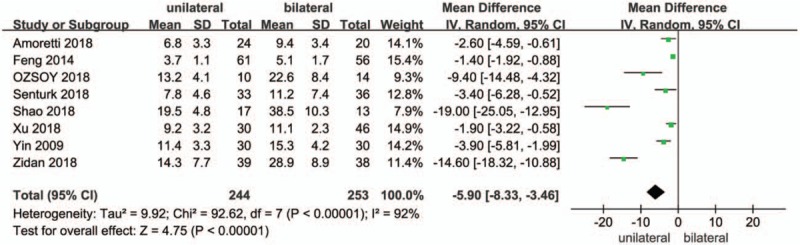
A forest plot for the sensitivity analysis in operating time.
3.10. Bias analysis
A funnel plot for the studies about operating time in unilateral and bilateral PVP groups was performed (Fig. 9). All the studies were included in the plot. The result showed that there existed some publication bias since the symmetrical characteristic of the funnel plot was not good.
Figure 9.
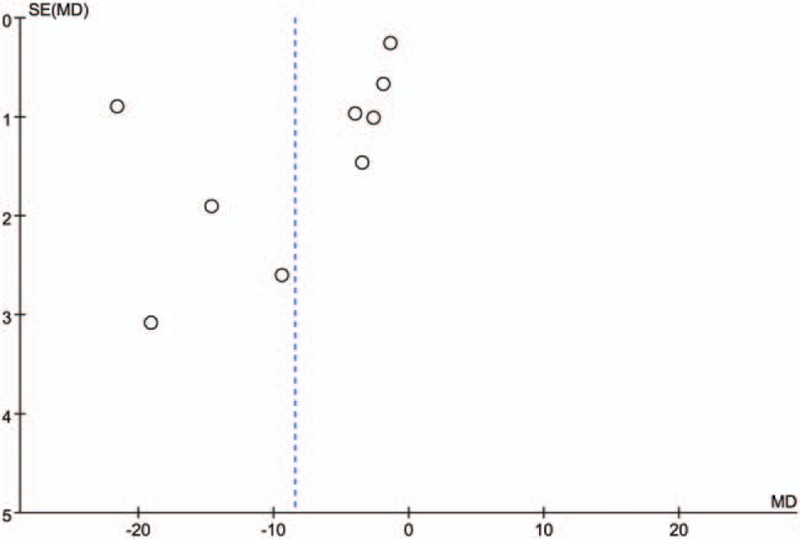
A funnel plot for the studies about operating time in unilateral and bilateral PVP groups. PVP = percutaneous vertebroplasty.
4. Discussion
Osteoporosis is a progressive and metabolic bone disease. The main manifestations are the increase of bone brittleness, the decrease of bone mass and the decrease of bone strength.[20–22] It is one of the important factors that affect the quality of life in the elderly, and the most common complication is the osteoporotic compression fracture of the thoracolumbar spine.
PVP is one of the mainstream treatments for OVF, which can rapidly relieve pain and stability of vertebral fractures. However, the choice of surgical approach remains controversial.[23,24] Some researchers believe that bilateral PVP is more effective in relieving pain, which is related to the distribution of bone cement in the vertebral body. In recent years, unilateral PVP has been increasingly used in surgery, reduced exposure time to radiation, reduced risk of cement leakage, and complications. Bilateral PVP showed increased operation time and injected cement volume, while unilateral PVP reduced operation time, surgery-related complications and radiation exposure.
VAS is a psychometric response scale used in questionnaires, which is to measure the subjective characteristics or attitudes that cannot be directly measured. Studies adopt VAS to estimate pain relief after PVP surgery. In this research, VAS score between unilateral and bilateral PVP was not significant (MD = −0.05, 95% CI [−0.24, 0.13], P = .57; P for heterogeneity = .007, I2 = 44%). This indicated that the pain relief of unilateral group was as much as that of bilateral group. ODI is an index that used by clinicians and researchers to quantify disability for low back pain. The results showed that the ODI score of unilateral PVP was similar to that of bilateral PVP (MD = 0.03, 95% CI [−0.57, 0.62], P = .93; P for heterogeneity = .73, I2 = 0%). Cement leakage is a common complication of vertebroplasty. Symptoms of nerve irritation with compression of nerve roots may be caused by the leakage. Difference of cement leakage between unilateral and bilateral PVP was not significant (OR = 1.00, 95% CI [0.67, 1.50], P = 1.00; P for heterogeneity = .98, I2 = 0%). Yu reported that the effects of unilateral and bilateral PVP had no difference.[25] Patients with severe vertebral deformation were recommended to adopt bilateral PVP while unilateral PVP was preferred when degree of vertebral compression is not large.
There is significant difference of the operating time in unilateral group and bilateral group (MD = −8.42, 95% CI [−13.17, −3.66], P = .0005; P for heterogeneity <.00001, I2 = 98%). The operating time in unilateral group was less than bilateral group. The patients in bilateral group have been injected more cement than patients in a unilateral surgery (MD = −2.56, 95% CI [−2.79, −2.33], P <.00001; P for heterogeneity = .65, I2 = 0%). Qi suggested that unilateral PVP as the advantages of low incidence of cement injection, short exposure time and short operative time.[26]
In the comparison between PVP and conservative therapy, PVP had a better clinical effect. Mattie and Rachelle reported that the effect of PVP exceeded the effect of conservative therapy with respect to pain relief in patients with osteoporotic compression fractures.[27,28]
The results in this study supported that the unipedicular PVP is a faster treatment for comparable spinal deformity contrasted with the bipedicular approach. It also improves the cost-effectiveness of the procedure for injecting less cement and reduces the operation time, thereby reducing the risk of disease. However, there exists controversy about the effect of PVP that the clinical effect of PVP and placebo have no difference.[29] Some surgeons believe that PVP better effect in the relieving acute pain than conservative treatment, but in the long-term efficacy the difference between PVP and placebo had no significance.[30] The clinical efficacy of PVP needs to be further researched
However, some limitations still existed in this research. First, the more indicators in both unilateral and bilateral groups could be analyzed, and it could be evaluated in the future. Second, more articles could be involved, which could be conducted in the further research. Third, the comparison among unipedicular approach, bilateral PVP and conservative therapy could be conducted in the future.
Author contributions
Conceptualization: Yingchun Chen.
Data curation: Lin Zhang, Er-nan Li.
Investigation: Lin Zhang, Er-nan Li, Li-xiang Ding, Gen-ai Zhang, Yu Hou, Wei Yuan.
Methodology: Lin Zhang, Er-nan Li.
Project administration: Lin Zhang.
Resources: Li-xiang Ding, Gen-ai Zhang, Yu Hou, Wei Yuan.
Supervision: Yingchun Chen.
Validation: Er-nan Li, Li-xiang Ding.
Writing – review & editing: Yingchun Chen.
Footnotes
Abbreviations: CIs = confidence intervals, ODI = Oswestry Disability Index, OVF = osteoporotic vertebral fracture, VAS = Visual Analog Scale/Score.
The authors have no conflicts of interest to disclose.
References
- [1].Muijs SPJ. Percutaneous vertebroplasty for painful long-standing osteoporotic vertebral compression fractures: indication, clinical outcome, cement leakage & classification. Dep Orthop Surg Fac Med 2012. [Google Scholar]
- [2].Shimizu R. Percutaneous vertebroplasty for osteoporotic vertebral pseudoarthrosis with intravertebral cleft. Spine J 2012;12:S158–9. [Google Scholar]
- [3].Aslam E, Muhammad T, Sharif S. Percutaneous vertebroplasty in osteoporotic vertebral compression fractures: our initial experience. JPMA J Pak Med Assoc 2008;58:498. [PubMed] [Google Scholar]
- [4].Voormolen MH. The risk of new osteoporotic vertebral compression fractures in the year after percutaneous vertebroplasty. J Vasc Interv Radiol 2006;17:71–6. [DOI] [PubMed] [Google Scholar]
- [5].Yu W. Risk factors for recollapse of the augmented vertebrae after percutaneous vertebroplasty for osteoporotic vertebral fractures with intravertebral vacuum cleft. Medicine 2017;96:e5675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Balkarli H. Treatment of osteoporotic vertebral compression fractures with percutaneous vertebroplasty under local anesthesia: clinical and radiological results. Int J Clin Exp Med 2015;8:16287–93. [PMC free article] [PubMed] [Google Scholar]
- [7].Chen LH. Percutaneous vertebroplasty for pathological vertebral compression fractures secondary to multiple myeloma. Arch Orthop Trauma Surg 2012;132:759–64. [DOI] [PubMed] [Google Scholar]
- [8].Jurczyszyn A. Percutaneous vertebroplasty for pathological vertebral compression fractures secondary to multiple myeloma—medium-term and long-term assessment of pain relief and quality of life. Adv Clin Exp Med Off Organ Wroclaw Med Univ 2015;24:651–6. [DOI] [PubMed] [Google Scholar]
- [9].Ng PP, CL., Dowd CF. Percutaneous vertebroplasty: an emerging therapy for vertebral compression fractures. Semin Neurol 2002;22:149–56. [DOI] [PubMed] [Google Scholar]
- [10].Zhao H. The importance of percutaneous vertebroplasty and radiation therapy for pathological vertebral compression fractures secondary to multiple myeloma. Arch Orthop Trauma Surg 2012;132:1669–70. [DOI] [PubMed] [Google Scholar]
- [11].Xu W. Correlation analysis between the magnetic resonance imaging characteristics of osteoporotic vertebral compression fractures and the efficacy of percutaneous vertebroplasty: a prospective cohort study. BMC Musculoskelet Disord 2018;19: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Amoretti N. Percutaneous vertebroplasty in tumoral spinal fractures with posterior vertebral wall involvement: Feasibility and safety. Eur J Radiol 2018;104:38–42. [DOI] [PubMed] [Google Scholar]
- [13].Şenturk S. Minimally invasive translaminar endoscopic approach to percutaneous vertebroplasty cement leakage: technical note. World Neurosurg 2018;117:15–9. [DOI] [PubMed] [Google Scholar]
- [14].Zidan I, Fayed AA, Elwany A. Multilevel percutaneous vertebroplasty (more than three levels) in the management of osteoporotic fractures. J Korean Neurosurg Soc 2018;61:700–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Ozsoy KM. Percutaneous vertebroplasty for the treatment of osteoporotic thoracolumbar fractures with posterior body involved in elderly patients. Turkish Neurosurg 2018;29:90–4. [DOI] [PubMed] [Google Scholar]
- [16].Hai-Bo Sun and XJ. The Optimal Volume Fraction in Percutaneous Vertebroplasty Evaluated by Pain Relief, Cement Dispersion, and Cement Leakage: A Prospective Cohort Study of 130 Patients with Painful Osteoporotic Vertebral Compression Fracture in the Thoracolumbar Vertebra. World Neurosurg, 2018. [DOI] [PubMed] [Google Scholar]
- [17].Shao Lei, AE Comparison of curative effect between unilateral and bilateral percutaneous vertebroplasty in the treatment of senile lumbar vertebral compression fractures. Imaging Res Med Appl 2018;251–2. [Google Scholar]
- [18].Feng Yu, WH Comparison of unilateral and bilateral percutaneous vertebroplasty for treating aged osteoporotic vertebral compression fractures with local anesthesia. J Clin Exp Med 2014;13:911–4. [Google Scholar]
- [19].Yin Li-gang, TB A comparison of the short-tern efficacy in aged osteoporofic vertebral compressive fratctllres: Unilateral percutaneous vertebroplasty versus bilateral percutaneous vertebroplasty. Chin J Osteoporos 2009. [Google Scholar]
- [20].Hemama M, Fatemi NE, Gana R. Percutaneous vertebroplasty in Moroccan patients with vertebral compression fractures. Pan African Med J 2017;26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Radchenko V, Popov A. Study of percutaneous vertebroplasty in osteoporosis vertebral compression fractures using various compositive materials. Internet J Minimal Invas Spinal Technol 2010. [Google Scholar]
- [22].Kim MS. Percutaneous Vertebroplasty in Osteoporotic Vertebral Compression Fractures; The Degree of Vertebral Compression and Outcome. 2003. [Google Scholar]
- [23].Im TS. Effects of facet joint injection reducing the need for percutaneous vertebroplasty in vertebral compression fractures. Cardiovasc Intervent Radiol 2016;39:740–5. [DOI] [PubMed] [Google Scholar]
- [24].Zhao DH. Postoperative functional evaluation of percutaneous vertebroplasty compared with percutaneous kyphoplasty for vertebral compression fractures. Am J Ther 2016;23: [DOI] [PubMed] [Google Scholar]
- [25].Yu Dongfang, QX Curative effectiveness of PVP by trans-single-pedicle approach VS trans-both-pedicles approach for vertebral compression fractures. J Clin Surg 2012;20: [Google Scholar]
- [26].Qi Zhenliang, LW Comparison of unilateral and bilateral percutaneous vertebroplasty in the treatment of thoracolumbar osteoporotic compression fractures. J Cervicodynia Lumbodynia 2016;501–3. [Google Scholar]
- [27].Mattie R, Laimi K, Yu S, et al. Comparing percutaneous vertebroplasty and conservative therapy for treating osteoporotic compression fractures in the thoracic and lumbar spine: a systematic review and meta-analysis. J Bone Jt Surg Am Vol 2016;98:1041. [DOI] [PubMed] [Google Scholar]
- [28].Buchbinder R, Johnston RV, Rischin KJ, et al. Percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Cochrane Database Syst Rev 2015;4:CD006349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Wali A, Martin J, Rennert R, et al. Vertebroplasty for vertebral compression fractures: placebo or effective? Surg Neurol Int 2017;8:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Lehman VT, Gray LA, Kallmes DF. Percutaneous vertebroplasty for painful compression fractures in a small cohort of patients with a decreased expectation-related placebo effect due to dementia. AJNR Am J Neuroradiol 2008;29:1461–4. [DOI] [PMC free article] [PubMed] [Google Scholar]


