Abstract
Combined anterior cruciate ligament (ACL) and medial collateral ligament (MCL) injuries are the most common type of combined ligamentous injury of the knee. The optimal treatment for these combined injuries is controversial. Combined ACL and MCL–posterior oblique ligament (POL) reconstruction avoids late anteromedial rotatory instability and chronic valgus instability of the knee and decreases the increased stress on the ACL graft. Graft choice (hamstring tendon autograft, quadriceps bone–patellar tendon–bone autograft, or Achilles tendon allograft) and anatomic restoration of the medial and posteromedial corner of the knee are challenges of this combined reconstruction. This article describes a technique that allows combined ACL and MCL-POL reconstruction. The hamstring tendons from the contralateral limb are tripled and used as the ACL graft. The gracilis tendon from the ipsilateral limb is doubled and used as the MCL-POL graft. The semitendinosus tendon of the ipsilateral limb is preserved. After ACL reconstruction, the MCL-POL graft is suspended on the ACL graft at the distal end of the tibial tunnel and the graft limbs are used for open reconstruction of the MCL and POL. Three interference screws (Arthrex, Naples, FL) and 1 metal staple are used for graft fixation of this combined reconstruction.
In the literature, 78% of combined knee injuries were anterior cruciate ligament (ACL) tears with medial collateral ligament (MCL) injuries,1, 2 and in 1 series, 99% of MCL injuries were associated with injury of the posterior oblique ligament (POL).3 Many surgeons agree that nonsurgical treatment of most isolated medial collateral ligament complex (MCLC) injuries leads to good results whereas operative intervention is required for combined multiligamentous injuries and for isolated injuries with chronic instability.4
Combined ACL and MCL-POL reconstruction avoids late anteromedial rotatory instability (AMRI) and chronic valgus instability of the knee and decreases the increased stress on the ACL graft.5, 6, 7, 8, 9 Gallo et al.10 (2017) described a technique for combined ACL and MCL reconstruction using a single Achilles tendon allograft. However, the potential shortcoming of this technique is its inability to reconstruct the POL, which plays a key role in limiting internal rotation with the knee in full extension.10, 11
Another technique was described by Hetsroni and Mann12 (2016) for combined reconstruction of the MCL and ACL using ipsilateral quadriceps tendon–bone and bone–patellar tendon–bone autografts. However, the disadvantages of this technique were the extended rehabilitation time for full recovery of the extensor mechanism, the increased risk of patellar fracture, and the inability to reconstruct the POL.12
Combined reconstruction of the MCL and ACL using ipsilateral semitendinosus and gracilis tendon autografts can be performed.12 However, this eliminates an important medial-sided stabilizer and weakens the anterior restraining action of the hamstring. Moreover, it results in a nonanatomic reconstruction of the MCL if the semitendinosus insertion is left intact during reconstruction.12
This article describes a technique that allows combined anatomic ACL and MCL-POL reconstruction (Video 1). The hamstring tendons from the contralateral limb are used as the ACL graft. The gracilis tendon from the ipsilateral limb is used as the MCL-POL graft. The semitendinosus tendon of the ipsilateral limb is preserved. The distal end of the ACL tibial tunnel is made at the anatomic distal attachment of the superficial MCL. At the end of ACL reconstruction, the ACL graft is fixed by 1 interference screw (Arthrex, Naples, FL) at its femoral tunnel. Then, the MCL-POL graft is suspended on the ACL graft at the distal end of the ACL tibial tunnel, and both grafts are fixed by another interference screw (Arthrex). The MCL-POL graft limbs are subsequently used for open, nearly anatomic reconstruction of the MCL and POL. One interference screw (Arthrex) and 1 staple are used for MCL-POL graft fixation.
Surgical Technique
Examination Under Anesthesia
The patient is positioned supine on the operating table. An examination under anesthesia is performed. Patients with a grade III torn ACL and grade III torn MCL are selected. Exposure of the medial side of the knee is performed first. Arthroscopic work is delayed until after medial exposure to avoid anatomic distortion from fluid extravasation.
Graft Preparation
A tourniquet is applied on the normal limb, and the semitendinosus and gracilis tendons are harvested, prepared, and tripled to be used as the ACL graft. Then, a tourniquet is applied on the affected limb. Surgical exposure of the medial side of the knee is achieved, and the gracilis tendon is harvested and prepared for use as the MCL-POL graft. The semitendinosus tendon of the affected limb is preserved.
Medial Surgical Exposure
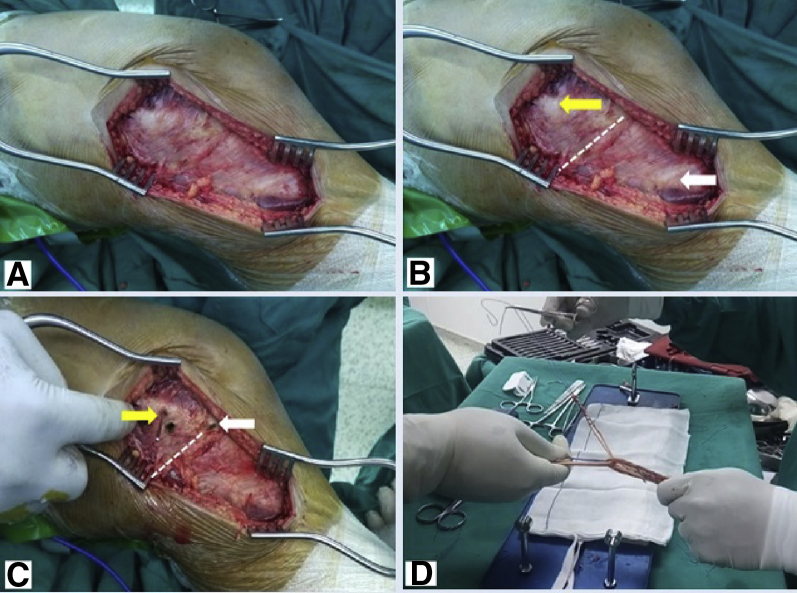
The surgeon makes a medial skin incision directed from 1 cm above the adductor tubercle down to 6 cm beyond the joint line (Fig 1A). The medial femoral epicondyle, joint line, and semitendinosus insertion are identified (Fig 1B). The surgeon inserts 1 Kirschner wire at the center of the medial femoral epicondyle and another in the joint (Fig 1C). The gracilis tendon is harvested, prepared, and suspended on the ACL graft to be used as the MCL-POL graft (Fig 1D).
Fig 1.
Medial surgical exposure of left knee (with patient supine and knee flexed 30°). (A) The skin incision is made 1 cm above the adductor tubercle and 6 cm below the joint line. (B) The surgeon identifies the medial femoral epicondyle (yellow arrow), joint line (white dashed line), and semitendinosus insertion (white arrow). (C) The surgeon inserts 1 Kirschner wire at the center of the medial femoral epicondyle (yellow arrow) and another in the joint (white arrow). (D) The gracilis tendon is harvested, prepared, and suspended on the anterior cruciate ligament graft to be used as the medial collateral ligament–posterior oblique ligament graft.
Marking Points of MCL-POL Attachments
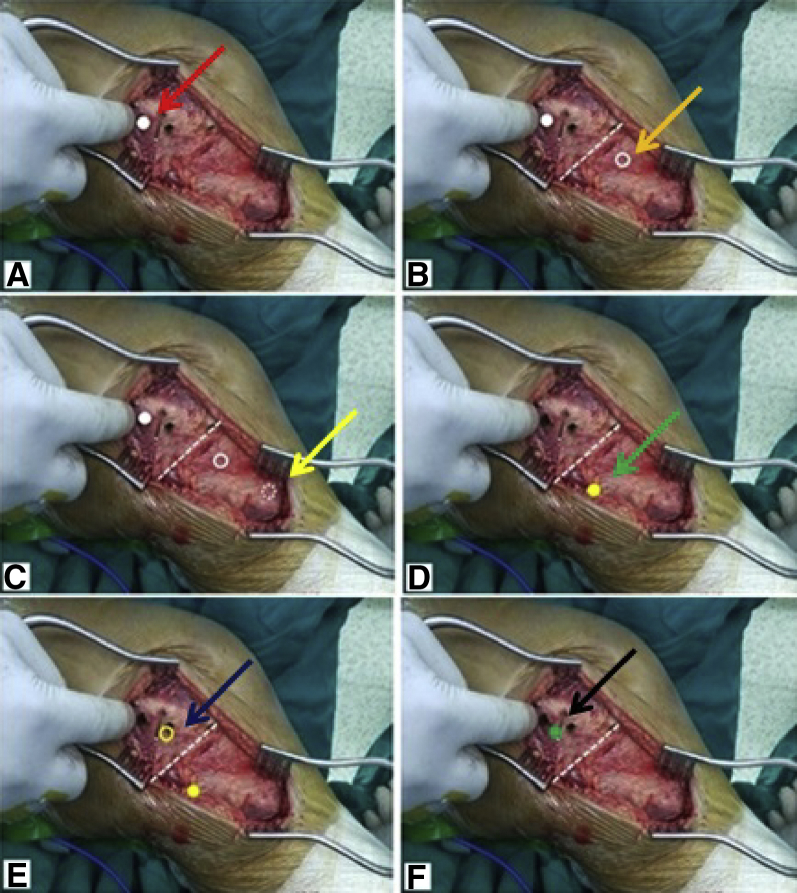
The surgeon marks the following points: point A, 3.2 mm proximal and 4.8 mm posterior to the medial femoral epicondyle (Fig 2A); point B, 1.2 cm distal to the joint line over the anterior aspect of the semimembranosus tendon (Fig 2B); and point C, 6.1 cm distal to the joint line just posterior to the semitendinosus insertion (Fig 2C). Although the proximal tibial attachment of the superficial MCL has a much lower load to failure than the distal tibial attachment, both attachments provide substantial functional contributions, including resisting valgus gapping, and therefore should be restored during MCL reconstruction.13 Then, the surgeon marks the following points: point D, 2 mm lateral to the medial tibia and 2 cm distal to the tibial plateau (Fig 2D); point E, 8 mm distal and 6 mm anterior to the posterior edge of the medial femoral epicondyle (Fig 2E); and point F, the intersection of the axes of the MCL and POL (Fig 2F).
Fig 2.
Marking points of medial collateral ligament–posterior oblique ligament attachments in left knee (with patient supine and knee flexed 30°). (A) Point A (white solid circle and red arrow), 3.2 mm proximal and 4.8 mm posterior to medial femoral epicondyle. (B) Point B (white empty circle and orange arrow), 1.2 cm distal to joint line (white dashed line) just anterior to semimembranosus tendon. (C) Point C (white dotted empty circle and yellow arrow), 6.1 cm distal to joint line (white dashed line) just posterior to semitendinosus insertion. (D) Point D (yellow solid circle and green arrow), 2 mm lateral to medial tibia and 2 cm distal to tibial plateau. (E) Point E (yellow empty circle and blue arrow), 8 mm distal and 6 mm anterior to posterior edge of medial femoral epicondyle. (F) Point F (green solid circle and black arrow), point of intersection of axes of medial collateral ligament and posterior oblique ligament at femur (isometric point).
Medial Subfascial Tunnel Creation
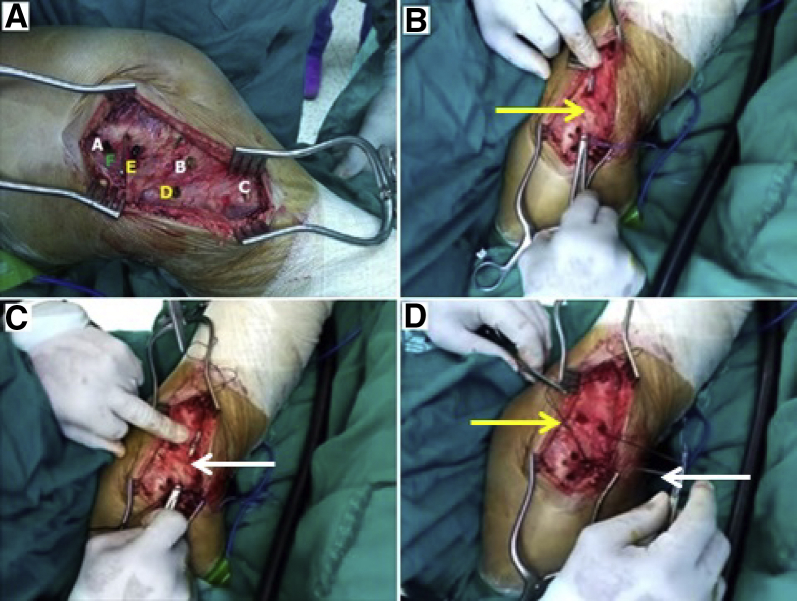
After the points of the MCL-POL attachments are marked (Fig 3A), 2 subfascial tunnels are created using a curved artery clamp. An anterior subfascial tunnel is created from point F to point B (Fig 3B) and then to point C. A posterior subfascial tunnel is created from point F to point D (Fig 3C) and then to point C. Passing sutures are passed through the subfascial tunnels (Fig 3D) for graft limb passage during MCL-POL reconstruction.
Fig 3.
Medial subfascial tunnel creation in left knee (with patient supine and knee flexed 30°). (A) Points of medial collateral ligament–posterior oblique ligament attachments (points A-F). (B) The anterior subfascial tunnel (yellow arrow) is created from point F through point B to point C. (C) The posterior subfascial tunnel (white arrow) is created from point F to point D. (D) Passing sutures (yellow and white arrows) are passed through subfascial tunnels.
The subfascial tunnels are passed more deeply near the joint line to include the meniscocapsular attachment. The deep MCL represents a thickening in the middle third of the medial capsular ligament. It is divided into a proximal meniscofemoral division and a distal meniscotibial division, with a firm meniscal attachment in the middle portion.14
The POL consists of 3 arms: superficial, central, and capsular arms.15, 16 The central arm is the largest, thickest, and most functionally important.15, 17 The proximal POL attachment is closer to the adductor tubercle and other nearby structures.16, 18, 19 The distal POL attachment is adjacent to the semimembranosus tendon and has an additional attachment to the medial meniscus.
Arthroscopic Examination
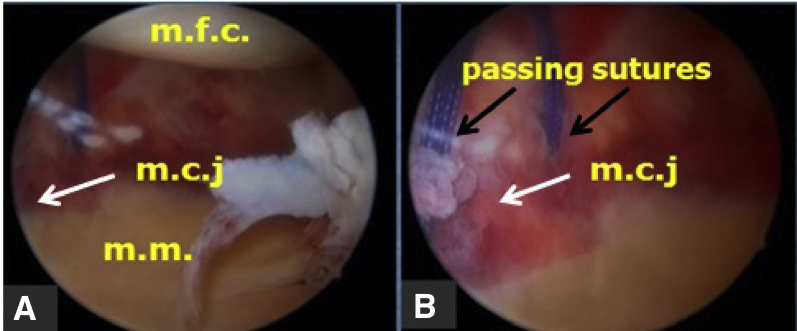
Arthroscopy is started. Arthroscopic examination of the medial compartment is performed to evaluate it for a femur-tibia gap and the meniscocapsular junction, medial meniscus (Fig 4A), and opening of the medial compartment with valgus stress applied to the knee. A portion of the passing sutures used for MCL-POL graft limb passage may be seen (Fig 4B).
Fig 4.
Arthroscopic examination. Arthroscopic view through the lateral portal in a left knee. (A) Evaluation of medial compartment, showing wide femur-tibia gap, meniscocapsular junction (mcj) (white arrow), and medial meniscus (mm). (mfc, medial femoral condyle.) (B) Passing sutures (black arrows) for medial collateral ligament–posterior oblique ligament graft limbs and meniscocapsular junction (mcj) (white arrow).
ACL Reconstruction
Single-bundle anatomic ACL reconstruction is performed using tripled hamstring tendon autografts from the contralateral limb.
ACL Tibial Tunnel Creation
The surgeon determines the location of the tibial footprint of the ACL, which is located 3 mm anterior to the inner border of the anterior horn of the lateral meniscus, just lateral to the medial eminence, and 7 to 10 mm anterior to the PCL. The surgeon also determines the location of point C, which represents the most distal attachment site of the superficial MCL on the tibial cortex. It is located 6.1 cm distal to the joint line, just posterior to the semitendinosus insertion.
The ACL aiming device (Arthrex) is fitted between point C (Fig 2C) and the ACL tibial footprint. An ACL guidewire is drilled (Fig 5A). Reaming the tibial tunnel by an appropriately sized reamer is performed over the guidewire using a curette over the pin during reaming for protection (Fig 5B). The reamed tibial tunnel is closed by a plastic stopper to maintain joint distension for better visualization.
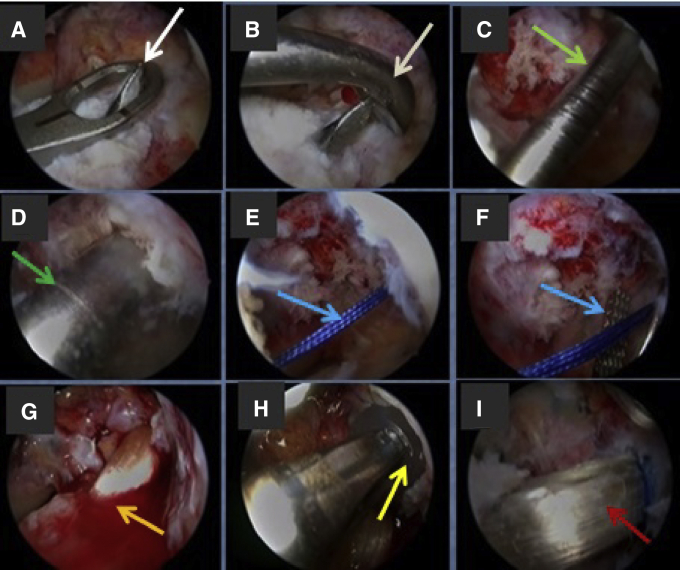
Fig 5.
Anterior cruciate ligament (ACL) reconstruction. Arthroscopic view through lateral portal in a left knee. (A) The ACL guidewire (white arrow) is drilled. (B) A curette over the pin (white arrow) is used during reaming for protection. (C) The ACL guide pin (green arrow) is drilled in the femoral footprint. (D) The femoral tunnel is reamed by an appropriately sized reamer (green arrow). (E) Passing sutures (blue arrow) are passed through the femoral tunnel using the guidewire. (F) The passing sutures in the femoral tunnel are kept there and retrieved (blue arrow) through the ACL tibial tunnel. (G) The ACL graft (orange arrow) is passed through the tibial tunnel to the joint and then to the femoral tunnel. (H) The ACL graft is fixed at the femoral tunnel by an interference screw (yellow arrow). (I) ACL graft (red arrow) after complete fixation.
ACL Femoral Tunnel Creation
The surgeon determines the location of the femoral footprint of the ACL. An ACL guide pin passed through the medial portal is drilled in the femoral footprint with the knee flexed 120° (Fig 5C). The femoral tunnel is reamed by an appropriately sized reamer (Fig 5D).
Passing sutures are passed through the femoral tunnel using the guidewire (Fig 5E). The passing sutures in the femoral tunnel are kept there and retrieved (Fig 5F) through the ACL tibial tunnel to the exterior.
Graft Passage and Fixation
By use of the passing sutures, the ACL graft is passed through the tibial tunnel to the joint and then to the femoral tunnel (Fig 5G). The MCL-POL graft is suspended on the ACL graft at the distal end of the ACL tibial tunnel. The ACL graft is fixed at the femoral tunnel by an interference screw (Fig 5H). MCL-POL graft suspension is performed before ACL graft fixation at the femoral tunnel.
At the end of ACL reconstruction (Fig 5I), the ACL and MCL-POL grafts at the distal end of the ACL tibial tunnel are fixed by an interference screw (Fig 6A). The fixed suspended gracilis tendon graft limbs are used for open reconstruction of the MCL and POL (Fig 6B-D).
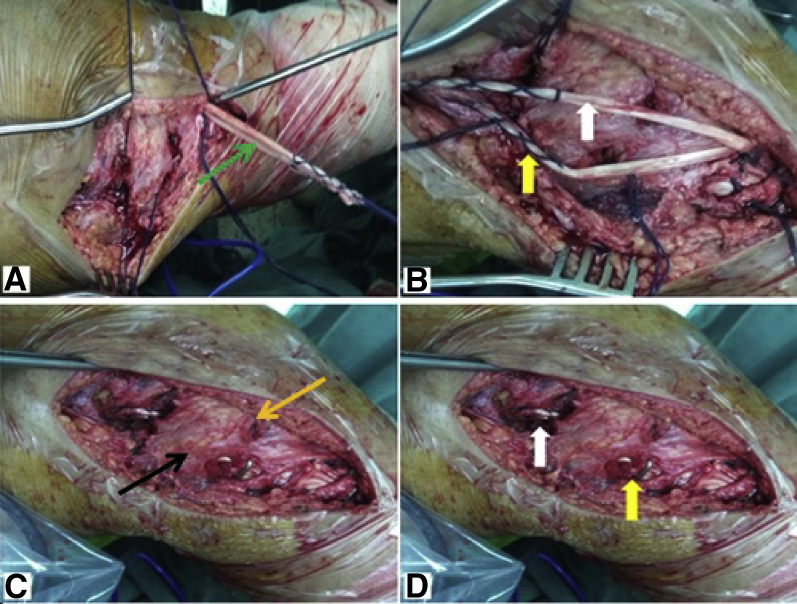
Fig 6.
Open medial collateral ligament–posterior oblique ligament reconstruction of left knee (with patient supine and knee flexed 30° during graft fixation). (A) The 2 limbs of the gracilis (green arrow) are suspended on the anterior cruciate ligament graft at the distal end of the tibial tunnel and fixed. (B) The anterior limb of the gracilis (white arrow) is used for medial collateral ligament reconstruction, and the posterior limb (yellow arrow) is used for posterior oblique ligament reconstruction. (C) The anterior limb of the gracilis is passed through the anterior subfascial tunnel (orange arrow), and the posterior limb of the gracilis is passed through the posterior subfascial tunnel (black arrow). (D) The posterior limb of the gracilis is fixed by a metal staple (yellow arrow) at point D, and both limbs are fixed by an interference screw (white arrow) at point F.
Open MCL-POL Reconstruction
The surgeon determines the point of the intersection of the axes of the MCL and POL on the femur (point F), which represents the isometric point of the MCL-POL (Fig 2F) and at which a femoral tunnel is created. A guide pin at point F is drilled, being directed anteriorly and upward, and then reamed by an appropriate reamer; suture loop is subsequently passed from medial to lateral through the tunnel, with the loop being left medially to be used for graft passage. The anterior limb of the suspended gracilis is passed through the anterior subfascial tunnel using the passing sutures, and the posterior limb is passed through the posterior subfascial tunnel (Fig 6C).
Both graft limbs are passed through a femoral tunnel at point F. With the knee flexed at 30° and slight varus, both graft limbs are fixed at the femoral tunnel (at point F) using an interference screw and the posterior limb of the graft is fixed (at point D) using a metal staple (Fig 6D) after the creation of a row bed at the tibial cortex. The superficial MCL is the primary restraint against valgus stress, external rotation at 30° of flexion, and internal rotation (along with the POL) at all flexion angles.14, 17, 20
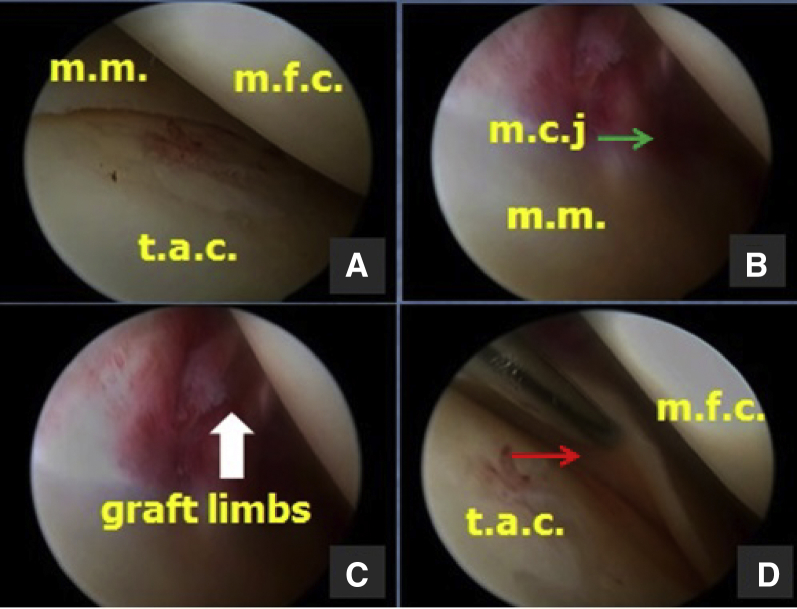
Arthroscopic Evaluation
After MCL-POL reconstruction, arthroscopic re-examination is performed to evaluate the ACL reconstruction (Fig 5I) and to evaluate the medial compartment for a femur-tibia gap (Fig 7A), as well as the meniscocapsular junction (Fig 7B), the MCL-POL graft limbs (Fig 7C), and the tibial meniscocapsular attachment (Fig 7D). Table 1 shows the advantages of the described technique, and Table 2 presents the surgical steps with pearls and pitfalls.
Fig 7.
Arthroscopic evaluation. Arthroscopic view through lateral portal in a left knee. (A) Evaluation of medial compartment for femur-tibia gap. (mfc, medial femoral condyle; mm, medial meniscus; tac, tibial articular cartilage.) (B) Evaluation of meniscocapsular junction (mcj, green arrow). (mm, medial meniscus.) (C) Evaluation of medial collateral ligament–posterior oblique ligament graft limbs (white arrow). (D) Evaluation of tibial meniscocapsular attachment (red arrow). (mfc, medial femoral condyle; tac, tibial articular cartilage.)
Table 1.
Advantages of Technique
| Combined reconstruction |
| No need for second operation as in staged reconstruction |
| Saves time of patient |
| Lower risk of ACL graft failure |
| No negligence of MCL reconstruction |
| POL reconstruction |
| Reconstruction of both MCL and POL |
| Nearly anatomic reconstruction of MCL |
| POL plays key role in limiting internal rotation with knee in full extension10https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5796970/11 |
| Graft choice |
| Avoids allograft comorbidities, less cost, more incorporation |
| Avoids risk of fracture of patella, early rehabilitation |
| Preserves ipsilateral semitendinosus, no more weakening of medial side of knee |
| Anatomic graft position and graft shape |
| Graft suspension |
| Adequate graft length for MCL and POL reconstruction |
| More graft fixation by graft anchorage at distal end of ACL tibial tunnel |
| Single tibial tunnel |
| One interference screw is used for fixation of both ACL and MCL grafts at tibial tunnel |
| Little morbidity to patient and with less cost |
| Minimizes number of tibial tunnels |
| Avoids tunnel collision and transection in medial tibial cortex |
| Avoids graft rupture and weakening or fracture of medial tibial cortex |
| Preserves bone stock at medial tibial cortex |
ACL, anterior cruciate ligament; MCL, medial collateral ligament; POL, posterior oblique ligament.
Table 2.
Surgical Steps, Pearls, and Pitfalls
| Surgical Step | Pearls | Pitfalls |
|---|---|---|
| Tourniquet | A tourniquet is applied to both sides, but the surgeon should elevate the tourniquet on the normal limb first for graft harvest. Then, after draping and complete instrumentation, the surgeon should elevate the tourniquet on the affected limb. | If the tourniquet is elevated on the affected limb first, this will lead to increased tourniquet time and the need for its release and then elevation, increasing surgery time. |
| ACL graft | A closed or open tendon stripper can be used to free the graft. A closed stripper is preferred. | The use of an open tendon stripper may be associated with premature cutting of the graft and a short graft. |
| Tripled hamstrings allow suspension at either end; suspension is achieved by sutures at the proximal end and by gracilis graft at the distal end. | Doubled hamstrings allow suspension at only 1 end and do not allow gracilis graft or passing-suture suspension. | |
| Tripled hamstrings allow adequate graft length. The ACL tibial tunnel is longer than usual because the distal end is made at least 6 cm below the joint line. | A quadrupled hamstring leads to a shorter ACL graft. A more proximal entry of the ACL tibial tunnel is associated with a nonanatomic MCL-POL graft position. | |
| MCL-POL graft | After medial surgical exposure, the gracilis tendon is harvested and the semitendinosus tendon is preserved. | If performed before medial surgical exposure, the semitendinosus tendon may be harvested accidentally. |
| Subfascial tunnels | The surgeon should start from proximal to distal. | The reverse is difficult. |
| Tunnels are created with the knee flexed 30°. | This is in line with the knee position during graft fixation. | |
| The anterior subfascial tunnel is passed under and posterior to the preserved semitendinosus. | A subfascial tunnel that is anterior or proximal to the preserved semitendinosus is nonanatomic. | |
| The anterior subfascial tunnel is created in 2 steps to give 2 tibial attachments. | If created in 1 step, this ignores the proximal tibial attachments. | |
| The posterior subfascial tunnel is created in 2 steps to give 2 tibial attachments. The proximal one is fixed by a metal staple after creation of a row bed at the tibial cortex. | If a row bed at the tibial cortex at the proximal tibial attachment is not created, graft-to-bone healing is delayed. | |
| Subfascial tunnels are passed deeply near the knee joint line. | This gives a more stable and anatomic reconstruction. | |
| The anterior subfascial tunnel forms, with the posterior tunnel, a triangle. Its apex is at the isometric point on the medial femoral condyle. | This gives a more stable and nearly anatomic MCL reconstruction. | |
| Passing sutures are made to mark the subfascial tunnels. | This allows easy graft passage at the MCL-POL reconstruction. | |
| ACL tibial tunnel | The entry point of the tibial tunnel should be 6 cm from the joint line posterior to the semitendinosus. | An entry point <6 cm below the joint line or anterior to the semitendinosus is nonanatomic. |
| The surgeon should use a curette through the anteromedial portal for protection during reaming. | If not used, PCL and/or articular cartilage injury may occur. | |
| The tibial guide pin is inserted while the knee is in 90° of flexion for proper visualization. | Knee flexion >90° will draw the infrapatellar fat pad into the field, making visualization difficult. | |
| Intermittent use of a plastic stopper in the tibial tunnel prevents loss of fluid and allows washout of bone debris through the tunnel. | Fluid loss will lead to loss of joint distension and accumulation of bone debris with poor visualization. | |
| Graft passage and fixation | The ACL graft is passed; then, the MCL-POL graft is suspended on the ACL graft at the medial cortex of the tibia. | If the ACL graft is passed after MCL-POL graft suspension, the graft may be impacted at the tibial tunnel. |
| The ACL graft is fixed at the femoral tunnel after MCL-POL graft suspension. | If the reverse is performed, MCL-POL graft suspension may be difficult. | |
| The ACL graft is fixed first at the femoral tunnel and then at the tibial tunnel. | If the reverse is performed, this may lead to loss graft tension. | |
| The entry point of the tibial tunnel is enlarged by a reamer to allow settling of the graft at the point of suspension. | If the entry point of the tibial tunnel is not enlarged, a painful prominent graft on the medial tibia and delayed suspended graft incorporation may occur. | |
| An interference screw of the same graft thickness with a length of 25-30 mm is used. The surgeon should ensure settling of the screw in the tunnel. | If the interference screw is not settled well, it may protrude under the medial fascia, causing its irritation. | |
| The interference screw is inserted in the anterior or distal half of the tibial tunnel. This is performed according to the orientation of the suspended graft; if the 2 graft limbs are oriented vertically after their suspension, the screw is inserted in the anterior half of the tibial tunnel, whereas if the 2 graft limbs are oriented horizontally after their suspension, the screw is inserted in the distal half of the tibial tunnel. | Insertion of the interference screw into the posterior or proximal half of the tibial tunnel will lead to graft impingement on the screw and will shorten the graft and cause its prominence. | |
| MCL graft | Passage is performed in a femoral tunnel at the isometric point and is directed anteriorly and upward. | This is done to avoid injury to the trochlear surface or intercondylar notch. |
| Arthroscopic evaluation | Arthroscopy at the end is performed to check the ACL reconstruction, ACL graft tension, and medial-compartment joint space and to show the intra-articular MCL graft limbs. |
ACL, anterior cruciate ligament; MCL, medial collateral ligament; POL, posterior oblique ligament.
Discussion
The MCLC is formed by many parts with different functions at different angles of knee flexion.21 This complex is formed by the superficial and deep MCL and the posteromedial corner (PMC) structures.22 The PMC structures include the POL, semimembranosus expansions, posterior horn of the medial meniscus, and oblique popliteal ligament.22
The MCLC acts as a primary stabilizer against valgus stress and a secondary significant restraint to rotatory motion and anterior-posterior translation.22 The complex injuries are not always isolated to the superficial MCL but can also involve the deep MCL and PMC structures.23 Injury to the POL is common, but other sites of disruption at the PMC have been reported.3
The MCL has the capacity to heal with conservative measures.24 However, injury to the PMC may not heal without surgical repair or reconstruction, particularly when it is part of a multiple-ligament injury.22, 25 Thus, specific surgical indications do exist for certain isolated and many combined MCLC injuries.
Injuries to the medial side of the knee are not always single injuries and may be combined with other knee ligament injuries. Combined ACL and MCLC injuries are the most common type of combined ligamentous injury of the knee. They represent 78% of combined knee ligament injuries.1, 2
The optimal management for combined ACL and MCLC injuries is still controversial.26 Combined ACL and MCL-POL reconstruction avoids late AMRI and chronic valgus instability of the knee and decreases the increased stress on the ACL graft.5, 6, 7, 8, 9
AMRI is defined as excessive valgus motion of the knee coupled with external rotation. The anteromedial tibial plateau subluxates anterior to the medial femoral condyle.27 Valgus instability places additional strain on a reconstructed anterior or posterior cruciate ligament, which can contribute to late graft failure.4, 9
Successful management of combined ACL and MCL-POL injuries requires reconstruction and elimination of all the elements of instability,21 and to restore function of the medial side of the knee, reconstruction must address all parts of the medial ligament: superficial and deep medial ligament and POL.28, 29 Xu et al.30 (2017) described an anatomic-like triangular-vector ligament reconstruction for the MCL and POL injury with a single femoral tunnel. They concluded that anatomic-like triangular ligament reconstruction can restore valgus stability and rotational stability and that the use of implantation can be reduced, decreasing the incidence rate of allergy and saving costs.
Gallo et al.10 (2017) performed combined ACL and MCL reconstruction using a single Achilles tendon allograft. However, the disadvantages of this technique include allograft complications and the inability of the technique to reconstruct the POL.10 The POL has a key role in the medial stability of the knee, and it has been reported that treatment of medial-compartment ligaments without repair of the POL often fails to achieve static stability.3, 11, 16, 23, 31, 32
The use of allograft to simultaneously reconstruct the ACL and MCL is associated with increased financial costs33 and carries the risk of disease transmission.34 Allograft has a slower remodeling response and slower biological incorporation than autograft.35, 36 It is one of the predictors of increased odds of graft failure, increased failure rates, and inferior functional outcomes in young active adults.37, 38
Hetsroni and Mann12 (2016) performed combined reconstruction of the ACL and MCL using ipsilateral quadriceps tendon–bone and bone–patellar tendon–bone autografts. However, the disadvantages of this technique are the increased risk of patellar fracture, the long rehabilitation time needed for full recovery of the extensor mechanism,12 and the inability of the technique to reconstruct the POL.
Yoshiya et al.39 (2005) argued that the use of semitendinosus and gracilis autografts in MCL reconstruction results in loss of their function as secondary medial stabilizers and weakens the anterior restraining action of the hamstrings. Moreover, a nonanatomic reconstruction of the MCL is produced when the semitendinosus insertion is left intact during reconstruction.12
This article describes a technique that allows combined ACL and MCL-POL reconstruction. The hamstring tendons from the contralateral limb are used as the ACL graft. The gracilis tendon from the ipsilateral limb is used as the MCL-POL graft. The semitendinosus tendon of the ipsilateral limb is preserved.
At the end of ACL reconstruction, the MCL-POL graft is suspended on the ACL graft at the distal end of the tibial tunnel and fixed and is then used for open triangular reconstruction of the MCL and POL through a single femoral tunnel. Three interference screws (Arthrex) and 1 metal staple are used for graft fixation of this combined reconstruction.
This reconstruction addresses the main elements of instability; avoids the complications of allografts; spares the ipsilateral semitendinosus tendon; uses a single femoral tunnel in MCL-POL reconstruction and a single tibial tunnel in combined ACL and MCL-POL reconstruction, thus preserving the medial tibial bone stock; avoids the possible tunnel merging on the tibial side; and decreases the number of implants used. It is of limited use for patients with a grade III torn MCL and ACL and for patients with healthy sites for graft harvest.
This technique has potential risks of a prolonged surgical time and possible tourniquet complications. Arranged surgical steps shorten the surgical time and avoid tourniquet complications.
The technique has a potential risk of possible injury to the physis in skeletally immature patients. Medial femoral physeal injury may occur during proximal MCL-POL graft tunneling and fixation. Medial tibial physeal injury may occur during distal POL graft fixation.
The overall functional results of ACL reconstruction in skeletally immature patients in many series were good40, 41, 42; there was only a single case of a growth abnormality, which consisted of a valgus deformity.43 Skeletal immaturity is a limitation to this technique owing to possible injury to the physis. Contralateral knee ligament injury and bilateral knee multiligament injuries are limitations to this technique because of the scarce source of the graft.
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Technique of combined anterior cruciate ligament (ACL) and medial collateral ligament (MCL)–posterior oblique ligament (POL) reconstruction of a left knee through a single tibial tunnel using hamstring tendon autografts (the patient is positioned supine). The steps of the technique are shown: (1) examination under anesthesia; (2) medial surgical exposure of the knee; (3) marking of the points of the MCL-POL attachments; (4) medial subfascial tunnel creation; (5) arthroscopic examination; (6) ACL reconstruction (ACL tibial tunnel creation, ACL femoral tunnel creation, and ACL graft passage and fixation); (7) open MCL-POL reconstruction; and (8) arthroscopic evaluation at end of procedure.
References
- 1.Elliott M., Johnson D.L. Management of medial-sided knee injuries. Orthopedics. 2015;38:180–184. doi: 10.3928/01477447-20150305-06. [DOI] [PubMed] [Google Scholar]
- 2.Miyakasa K.C., Daniel D.M., Stone M.L., Hirshman P. The incidence of knee ligament injuries in the general population. Am J Knee Surg. 1991;4:3–8. [Google Scholar]
- 3.Sims W.F., Jacobson K.E. The posteromedial corner of the knee: Medial-sided injury patterns revisited. Am J Sports Med. 2004;32:337–345. doi: 10.1177/0363546503261738. [DOI] [PubMed] [Google Scholar]
- 4.Marchant M.H., Tibor L.M., Sekiya J.K., Hardaker W.T., Garrett W.E., Taylor D.C. Management of medial-sided knee injuries, Part 1: Medial collateral ligament. Am J Sports Med. 2011;39:1102–1113. doi: 10.1177/0363546510385999. [DOI] [PubMed] [Google Scholar]
- 5.Grant J.A., Tannenbaum E., Miller B.S., Bedi A. Treatment of combined complete tears of the anterior cruciate and medial collateral ligaments. Arthroscopy. 2012;28:110–122. doi: 10.1016/j.arthro.2011.08.293. [DOI] [PubMed] [Google Scholar]
- 6.Mancini E.J., Kohen R., Esquivel A.O., Cracchiolo A.M., Lemos S.E. Comparison of ACL strain in the MCL-deficient and MCL-reconstructed knee during simulated landing in a cadaveric model. Am J Sports Med. 2017;45:1090–1094. doi: 10.1177/0363546516685312. [DOI] [PubMed] [Google Scholar]
- 7.Ahn J.H., Lee S.H. Risk factors for knee instability after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24:2936–2942. doi: 10.1007/s00167-015-3568-x. [DOI] [PubMed] [Google Scholar]
- 8.Zaffagnini S., Bignozzi S., Martelli S., Lopomo N., Marcacci M. Does ACL reconstruction restore knee stability in combined lesions? An in vivo study. Clin Orthop Relat Res. 2007;454:95–99. doi: 10.1097/BLO.0b013e31802b4a86. [DOI] [PubMed] [Google Scholar]
- 9.Battaglia M.J., Lenhoff M.W., Ehteshami J.R. Medial collateral ligament injuries and subsequent load on the anterior cruciate ligament: A biomechanical evaluation in a cadaveric model. Am J Sports Med. 2009;37:305–311. doi: 10.1177/0363546508324969. [DOI] [PubMed] [Google Scholar]
- 10.Gallo R.A., Kozlansky G., Bonazza N., Warren R.F. Combined anterior cruciate ligament and medial collateral ligament reconstruction using a single Achilles tendon allograft. Arthrosc Tech. 2017;6:e1821–e1827. doi: 10.1016/j.eats.2017.06.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Griffith C.J., Wijdicks C.A., LaPrade R.F., Armitage B.M., Johansen S., Engebretsen L. Force measurements on the posterior oblique ligament and superficial medial collateral ligament proximal and distal divisions to applied loads. Am J Sports Med. 2009;37:140–148. doi: 10.1177/0363546508322890. [DOI] [PubMed] [Google Scholar]
- 12.Hetsroni I., Mann G. Combined reconstruction of the medial collateral ligament and anterior cruciate ligament using ipsilateral quadriceps tendon-bone and bone-patellar tendon-bone autografts. Arthrosc Tech. 2016;5:e579–e587. doi: 10.1016/j.eats.2016.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wijdicks C.A., Ewart D.T., Nuckley D.J., Johansen S., Engebretsen L., LaPrade R.F. Structural properties of the primary medial knee ligaments. Am J Sports Med. 2010;38:1638–1646. doi: 10.1177/0363546510363465. [DOI] [PubMed] [Google Scholar]
- 14.LaPrade R.F., Engebretsen L., Marx R.G. Repair and reconstruction of medial- and lateral-sided knee injuries. Instr Course Lect. 2015;64:531–542. [PubMed] [Google Scholar]
- 15.LaPrade R.F., Engebretsen A.H., Ly T.V., Johansen S., Wentorf F.A., Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89:2000–2010. doi: 10.2106/JBJS.F.01176. [DOI] [PubMed] [Google Scholar]
- 16.Hughston J.C., Eilers A.F. The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. J Bone Joint Surg Am. 1973;55:923–940. [PubMed] [Google Scholar]
- 17.Griffith C.J., LaPrade R.F., Johansen S., Armitage B., Wijdicks C., Engebretsen L. Medial knee injury: Part 1. Static function of the individual components of the main medial knee structures. Am J Sports Med. 2009;37:1762–1770. doi: 10.1177/0363546509333852. [DOI] [PubMed] [Google Scholar]
- 18.Fischer R.A., Arms S.W., Johnson R.J., Pope M.H. The functional relationship of the posterior oblique ligament to the medial collateral ligament of the human knee. Am J Sports Med. 1985;13:390–397. doi: 10.1177/036354658501300605. [DOI] [PubMed] [Google Scholar]
- 19.Loredo R., Hodler J., Pedowitz R., Yeh L.R., Trudell D., Resnick D. Posteromedial corner of the knee: MR imaging with gross anatomic correlation. Skeletal Radiol. 1999;28:305–311. doi: 10.1007/s002560050522. [DOI] [PubMed] [Google Scholar]
- 20.Wijdicks C.A., Griffith C.J., LaPrade R.F. Medial knee injury: Part 2. Load sharing between the posterior oblique ligament and superficial medial collateral ligament. Am J Sports Med. 2009;37:1771–1776. doi: 10.1177/0363546509335191. [DOI] [PubMed] [Google Scholar]
- 21.Koga H., Muneta T., Yagishita K., Ju Y.-J., Sekiya I. Surgical management of grade 3 medial knee injuries combined with cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2012;20:88–94. doi: 10.1007/s00167-011-1541-x. [DOI] [PubMed] [Google Scholar]
- 22.Tibor L.M., Marchant M.H., Taylor D.C., Hardaker W.T., Garrett W.E., Sekiya J.K. Management of medial-sided knee injuries, Part 2: Posteromedial corner. Am J Sports Med. 2011;39:1332–1340. doi: 10.1177/0363546510387765. [DOI] [PubMed] [Google Scholar]
- 23.Jacobson K.E., Chi F.S. Evaluation and treatment of medial collateral ligament and medial-sided injuries of the knee. Sports Med Arthrosc. 2006;14:58–66. doi: 10.1097/01.jsa.0000212305.47323.58. [DOI] [PubMed] [Google Scholar]
- 24.Fanelli G.C., Harris J.D. Surgical treatment of acute medial collateral ligament and posteromedial corner injuries of the knee. Sports Med Arthrosc. 2006;14:78–83. doi: 10.1097/01.jsa.0000212301.80496.dc. [DOI] [PubMed] [Google Scholar]
- 25.Zhang H., Bai X., Sun Y., Han X. Tibial inlay reconstruction of the medial collateral ligament using Achilles tendon allograft for the treatment of medial instability of the knee. Knee Surg Sports Traumatol Arthrosc. 2014;22:279–284. doi: 10.1007/s00167-013-2382-6. [DOI] [PubMed] [Google Scholar]
- 26.Papalia R., Osti L., Del Buono A., Denaro V., Maffulli N. Management of combined ACL-MCL tears: A systematic review. Br Med Bull. 2010;93:201–215. doi: 10.1093/bmb/ldp044. [DOI] [PubMed] [Google Scholar]
- 27.Slocum D.B., Larson R.L. Rotatory instability of the knee: Its pathogenesis and a clinical test to demonstrate its presence. J Bone Joint Surg Am. 1968;50:211–225. [PubMed] [Google Scholar]
- 28.Robinson J.R., Bull A.M., Amis A.A. Structural properties of the medial collateral ligament complex of the human knee. J Biomech. 2005;38:1067–1074. doi: 10.1016/j.jbiomech.2004.05.034. [DOI] [PubMed] [Google Scholar]
- 29.Dong J.T., Chen B.C., Men X.Q. Application of triangular vector to functionally reconstruct the medial collateral ligament with double-bundle allograft technique. Arthroscopy. 2012;28:1445–1453. doi: 10.1016/j.arthro.2012.03.024. [DOI] [PubMed] [Google Scholar]
- 30.Xu H., Kang K., Zhang J. An anatomical-like triangular-vector ligament reconstruction for the medial collateral ligament and the posterior oblique ligament injury with single femoral tunnel: A retrospective study. J Orthop Surg Res. 2017;12:96. doi: 10.1186/s13018-017-0602-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hughston J.C. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without as associated rupture of the anterior cruciate ligament: Results of long-term follow-up. J Bone Joint Surg Am. 1994;76:1328–1344. doi: 10.2106/00004623-199409000-00008. [DOI] [PubMed] [Google Scholar]
- 32.Haimes J.L., Wroble R.R., Grood E.S., Noyes F.R. Role of the medial structures in the intact and anterior cruciate ligament-deficient knee: Limit of motion in the human knee. Am J Sports Med. 1994;22:402–409. doi: 10.1177/036354659402200317. [DOI] [PubMed] [Google Scholar]
- 33.Nagda S.H., Altobelli G.G., Bowdry K.A., Brewster C.E., Lombardo S.J. Cost analysis of outpatient anterior cruciate ligament reconstruction: Autograft versus allograft. Clin Orthop Relat Res. 2010;468:1418–1422. doi: 10.1007/s11999-009-1178-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mroz T.E., Joyce M.J., Steinmetz M.P., Lieberman I.H., Wang J.C. Musculoskeletal allograft risks and recalls in the United States. J Am Acad Orthop Surg. 2008;16:559–565. doi: 10.5435/00124635-200810000-00001. [DOI] [PubMed] [Google Scholar]
- 35.Tom J.A., Rodeo S.A. Soft tissue allografts for knee reconstruction in sports medicine. Clin Orthop Relat Res. 2002;402:135–156. doi: 10.1097/00003086-200209000-00012. [DOI] [PubMed] [Google Scholar]
- 36.Bhatia S., Bell R., Frank R.M. Bony incorporation of soft tissue anterior cruciate ligament grafts in an animal model: Autograft versus allograft with low-dose gamma irradiation. Am J Sports Med. 2012;40:1789–1798. doi: 10.1177/0363546511435637. [DOI] [PubMed] [Google Scholar]
- 37.Kaeding C.C., Pedroza A.D., Reinke E.K., Huston L.J., MOON Consortium. Spindler K.P. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: Prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43:1583–1590. doi: 10.1177/0363546515578836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mascarenhas R., Erickson B.J., Sayegh E.T. Is there a higher failure rate of allografts compared with autografts in anterior cruciate ligament reconstruction: A systematic review of overlapping meta-analysis. Arthroscopy. 2015;31:364–372. doi: 10.1016/j.arthro.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 39.Yoshiya S., Kuroda R., Mizuno K., Yamamoto T., Kurosaka M. Medial collateral ligament reconstruction using autogenous hamstring tendons: Technique and results in initial cases. Am J Sports Med. 2005;33:1380–1385. doi: 10.1177/0363546504273487. [DOI] [PubMed] [Google Scholar]
- 40.Cruz A.I., Jr., Fabricant P.D., McGraw M., Rozell J.C., Ganley T.J., Wells L. All-epiphyseal ACL reconstruction in children: Review of safety and early complications. J Pediatr Orthop. 2015;37:204–209. doi: 10.1097/BPO.0000000000000606. [DOI] [PubMed] [Google Scholar]
- 41.Nawabi D.H., Jones K.J., Lurie B., Potter H.G., Green D.W., Cordasco F.A. All-inside, physeal-sparing anterior cruciate ligament reconstruction does not significantly compromise the physis in skeletally immature athletes: A postoperative physeal magnetic resonance imaging analysis. Am J Sports Med. 2014;42:2933–2940. doi: 10.1177/0363546514552994. [DOI] [PubMed] [Google Scholar]
- 42.Calvo R., Figueroa D., Gili F. Transphyseal anterior cruciate ligament reconstruction in patients with open physes: 10-Year follow-up study. Am J Sports Med. 2015;43:289–294. doi: 10.1177/0363546514557939. [DOI] [PubMed] [Google Scholar]
- 43.Pennock A., Murphy M.M., Wu M. Anterior cruciate ligament reconstruction in skeletally immature patients. Curr Rev Musculoskelet Med. 2016;9:445–453. doi: 10.1007/s12178-016-9367-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technique of combined anterior cruciate ligament (ACL) and medial collateral ligament (MCL)–posterior oblique ligament (POL) reconstruction of a left knee through a single tibial tunnel using hamstring tendon autografts (the patient is positioned supine). The steps of the technique are shown: (1) examination under anesthesia; (2) medial surgical exposure of the knee; (3) marking of the points of the MCL-POL attachments; (4) medial subfascial tunnel creation; (5) arthroscopic examination; (6) ACL reconstruction (ACL tibial tunnel creation, ACL femoral tunnel creation, and ACL graft passage and fixation); (7) open MCL-POL reconstruction; and (8) arthroscopic evaluation at end of procedure.