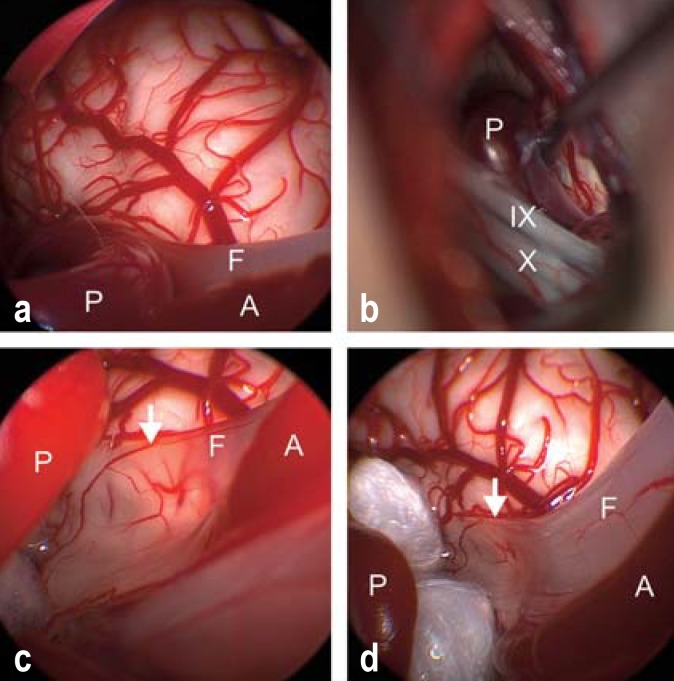
Figure 3.
Endoscopically assisted microvascular decompression for hemifacial spasm.
a) Inspection through the endoscope reveals vascular compression of the facial nerve (F) by a loop of the posterior inferior cerebellar artery (P), while the anterior inferior cerebellar artery (A) courses parallel to the nerve.
b) Inspection through the operating microscope reveals the posterior inferior cerebellar artery (P) but does not directly reveal the site of compression, which is hidden behind the lower cranial nerve group (cranial nerve IX, the glossopharyngeal nerve, and cranial nerve X, the vagus nerve).
c) After mobilization of the artery (P), inspection through the endoscope reveals that the facial nerve (F) is paper-thin after years of compression (14 years of symptoms) (arrow). The brainstem vessels are visible through the flattened, translucent nerve.
d) Two Teflon pledgets have been interposed between the posterior inferior cerebellar artery (P) and the facial nerve (F) to hold these two structures apart without touching the nerve at the site of its previous compression. The hemifacial spasm finally regressed 13 months after surgery; the long delay may be due to the severe structural change of the facial nerve as a result of its longstanding compression. The anterior inferior cerebellar artery (A) is marked as well.