Abstract
Background:
The majority of postmastectomy breast reconstruction performed in the United States is device-based. Typically, a tissue expander or implant is placed in the dual-plane (ie, subpectoral). Prepectoral breast reconstruction with acellular dermal matrices following mastectomy is a relatively new technique that has favorable outcomes with minimal complications and satisfactory aesthetic results. Few studies have compared opioid use between the 2 approaches. This study compares duration of postoperative opioid use among patients undergoing prepectoral device-based breast reconstruction with those in whom dual-plane devices were placed.
Methods:
We reviewed the records of adult female patients aged 18 years or older who underwent prepectoral or dual-plane device-based breast reconstructions following mastectomy by one of the 2 plastic surgeons (A.M. or M.V.) from 2015 to 2017 at a large tertiary care hospital. Patients with a history of substance abuse, chronic pain, or who were already receiving opioid medication were excluded. Electronic medical records were reviewed and patient surveys were conducted during postoperative visits to determine postoperative opioid requirements.
Results:
During the study period, 58 patients underwent dual-plane breast reconstruction and 94 underwent prepectoral reconstruction. Demographics and comorbidities of the groups were similar. By multivariate regression analysis, the prepectoral reconstruction group required 33% fewer days on opioid analgesic medication (P = 0.016) and were 66% less likely to require opioid prescription refills (P = 0.027). There were no statistically significant differences in other outcomes or complications.
Conclusion:
Patients undergoing prepectoral tissue expander or implant-based reconstruction required fewer days of opioid pain medication than those managed with the dual-plane technique.
BACKGROUND
Breast cancer is one of the most common malignancies and an increasing number of patients undergo mastectomy with or without immediate reconstruction.1,2 Conventional acellular dermal matrix–assisted breast reconstruction following mastectomy involves the 2-stage dual-plane tissue expander and subsequent implant placement or direct-to-implant single-stage dual plane reconstruction. Rates of infection, seroma formation, reconstructive failure, and pain associated with dual-plane breast reconstruction have been described.3 Prepectoral breast reconstruction following mastectomy has shown favorable outcomes with minimal complications and satisfactory aesthetic results.4,5 Considering the worsening opioid epidemic in the United States, surgeons are called upon to re-evaluate techniques to reduce postoperative pain and the need for opioid analgesic medications. The prepectoral approach does not require dissection of the pectoralis major muscle and previous studies have suggested it may lessen postoperative pain compared with dual-plane techniques. The objective of this study was to compare postoperative opioid requirements among patients undergoing prepectoral breast reconstruction compared with patients who were reconstructed using the dual-plane technique.
PATIENTS AND METHODS
We reviewed the records of adult female patients aged 18 years or older who underwent prepectoral or dual-plane device-based breast reconstructions following mastectomy by one of the 2 surgeons (A.M. or M.V.) from 2015 to 2017 at a large tertiary care hospital in Northern Virginia. Patients with a history of substance abuse, chronic pain, or who were already receiving opioid medication were excluded. Preoperative radiation therapy was not an exclusion criteria. The electronic medical records of these patients were reviewed and patient surveys were conducted during standard of care postoperative visits to determine the postoperative opioid pain medication requirements. The study was approved by the institutional review board governing research involving human subjects. One hundred fifty-two patients underwent unilateral or bilateral mastectomy by 7 breast surgeons during the study period. Ninety-four patients underwent immediate prepectoral reconstruction (37 direct-to-implant with 56 tissue expander, and 1 patient who underwent implant placement on one side and tissue expander on the other), and 58 patients underwent dual-plane reconstruction (6 direct-to-implant, 52 tissue expander) by 2 board-certified plastic surgeons (A.M. and M.V.) using acellular dermal matrix (Alloderm LifeCell Corporation or DermaCell Stryker Corporation, according to surgeon preference).
Mastectomy flaps were evaluated intraoperatively with SPY fluorescent Indocyanine Green imaging (SPY Elite Stryker Corporation, Kalamazoo, Mich.). All patients received standard pre- and postoperative antibiotics. The standard oral postoperative pain regimen was 30 tablets of acetaminophen/oxycodone, 5/325 mg (1–2 tablets every 4–6 hours as needed), acetaminophen/hydrocodone, 5/300 mg (1–2 tablets every 4–6 hours as needed), or oxycodone, 5 mg (1–2 tablets every 4–6 hours as needed), in addition to diazepam, 5 mg every 8 hours as needed for muscle spasm or tightness. Refills were not standardized and were based on patient need and clinical assessment on follow-up. Over-the-counter pain medications (ie, acetaminophen, ibuprofen, or other nonsteroidal anti-inflammatory drugs) were allowed at the patient’s discretion. Patients were cautioned about the maximum safe dose of acetaminophen and advised to keep track of this when taking both acetaminophen and either acetaminophen/oxycodone, 5/325 mg or acetaminophen/hydrocodone, 5/300 mg. As standard of care, patients were assessed at 1 week, 1 month, 6 months, and 1 year postoperatively, with the following questions asked during the postoperative visits:
1) How many days did you use opioid pain medications postoperatively?
2) How often did you take opioid pain medication postoperatively?
3) How many days did you take diazepam postoperatively?
Consistent with standard postoperative evaluation, patients were examined for complications such as seroma or hematoma formation, erythema, red breast syndrome, and mastectomy flap necrosis. The electronic medical records from both the practice’s office and hospital was also reviewed for refills of opioid prescriptions, use of other pain medications, need for additional procedures, 30-day all-cause readmissions, other clinical characteristics, failed reconstruction, and other complications related to initial procedure.
Descriptive statistics were provided for all covariates and outcomes: medians and interquartile ranges (IQRs) for continuous variables, and frequencies and percentages for categorical variables. Wilcoxon rank-sum test and Fisher’s exact test were used to compare the patient characteristics between the 2 groups for continuous variables and categorical variables, respectively. Univariate and multivariate negative binomial regression models were used to examine the impact of each covariate on postoperative duration of opioid usage. Incidence rate ratios (IRRs) were calculated with 95% confidence intervals (CIs). To assess the need for refills, logistic regression models were employed where odds ratios (ORs) and 95% CIs were reported. P values less than 0.05 were considered statistically significant. All statistical analysis was performed in R 3.3.2 (R Core Team, Vienna, Austria).
RESULTS
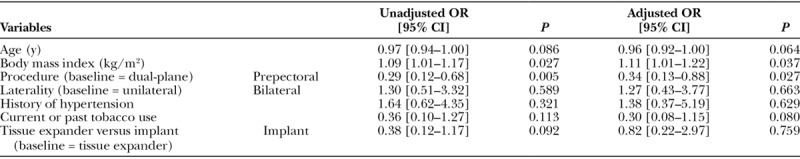
Patient demographics, comorbidities, and need for opioid prescriptions are summarized in Table 1. Of the 152 women undergoing 258 mastectomies (46 unilateral, 106 bilateral), 94 underwent prepectoral and 58 dual plane reconstructions. No statistically significant differences between the 2 groups in terms of age, body mass index, hypertension, diabetes, or tobacco use were observed. Table 2 compares the complications between the 2 cohorts. The prepectoral cohort required significantly fewer overall days of postoperative opioid pain medication (median 4 [IQR, 2–7] versus 7 [IQR, 3–13] days, P = 0.009) and a significantly smaller percentage of prepectoral patients required opioid prescription refills (10 [10.6%] versus 17 [29.3%], P = 0.005). Among the patients who did require refills, none required multiple opioid prescription refills in the prepectoral group and 3 (out of 17, 17.7%) did in the dual plane group, though not reaching statistical significance (P = 0.274). Tables 3, 4 present the results of negative binomial regression and logistic regression for duration of postoperative opioid usage and refills, respectively. After controlling for relevant covariates, the prepectoral group required 33% fewer days on opioids (adjusted IRR, 0.68; 95% CI, 0.48–0.93, P = 0.016) and were 66% less likely to require opioid prescription refills (adjusted OR, 0.34; 0.13–0.88, P = 0.027) opioids compared with the dual-plane group.
Table 1.
Summary of Patient Characteristics
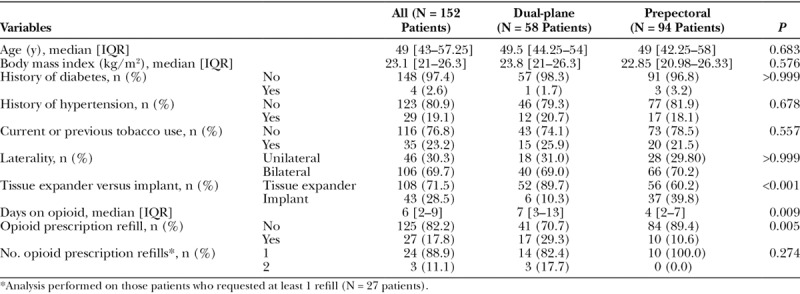
Table 2.
Comparison of Complications between Dual-plane and Prepectoral Cohorts
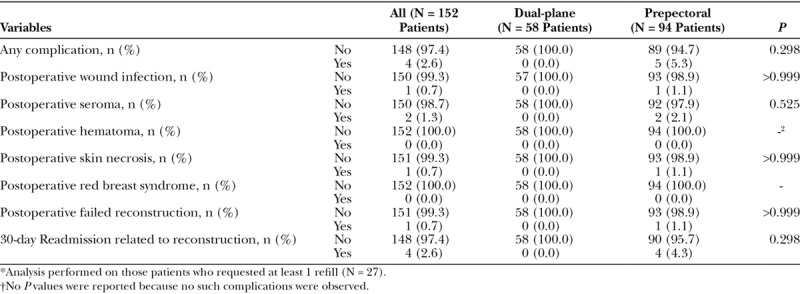
Table 3.
Results of Negative Binomial Regression Model for Number of Days on Postoperative Opioid Medications
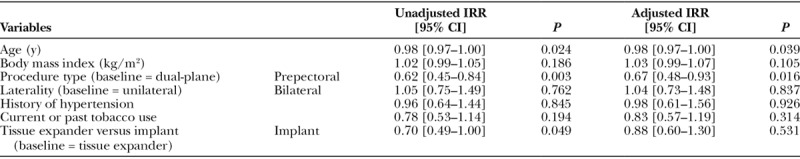
Table 4.
Results of Logistic Regression Model for Need for Opioid Prescription Refill
Four patients (4.3%) in the prepectoral group required readmission within 30 days due to 2 seromas, 1 wound infection with subsequent failure of reconstruction, and 1 mastectomy flap necrosis, though no statistically significant difference in complications were observed across the 2 groups (P = 0.298). Two patients developed seromas requiring surgical evacuation without need for expander removal, and underwent eventual successful implant placement. One patient developed a wound infection requiring readmission for intravenous antibiotics and expander removal. The patient who developed peri-incisional mastectomy flap necrosis was an active smoker throughout the pre- and postoperative period. She underwent intraoperative debridement and eventual successful implant placement.
DISCUSSION
Age-adjusted mortality rates of opioid overdose have tripled in the last decade and nonfatal opioid overdoses occur at least 7 times more often than fatal overdoses, with the majority occurring in nonchronic (less than 90 days) opioid users.6 Major contributors to opioid misuse are physician over-prescription and that surgical patients are discharged from the hospital 4 times more often than nonsurgical patients. Opioid-naive patients are at risk for chronic opioid use in the postoperative period. Evidence shows that each refill and additional week of opioid prescription use is associated with increased misuse.7–10 It is incumbent upon surgeons to re-evaluate surgical techniques to reduce the need for postoperative opioid analgesic medications.
Breast reconstruction following mastectomy is increasingly performed in the United States.11 The incidence of postoperative pain has increased in mastectomy patients undergoing classical reconstruction, via the subpectoral approach, with 49% experiencing acute and chronic pain.12–15 Previously described methods to reduce postoperative pain include a pain-catheter, which can be cumbersome for patients and is associated with hypotension, pneumothorax, and infection.16 Prepectoral breast reconstruction is associated with reconstructive outcomes comparable to those with dual-plane procedures.3,4 A Medline database review of English-language articles published in the last 20 years using the search terms, “mammoplasty or prepectoral or subpectoral” and “exp pain or exp narcotics”, found few studies that directly compared postoperative pain or narcotic use in patients undergoing dual plane versus prepectoral reconstruction. In our study, patients undergoing prepectoral reconstruction had less postoperative opioid use than the dual plane group, both in terms of overall days of opioid requirement and need for opioid prescription refills.
There were 4 (4.3%) 30-day readmissions in the prepectoral group related to seroma formation (2 patients), skin necrosis (1 patient), or wound infection (1 patient), though there was no statistically significant difference in complications between groups. The increased rate of seromas in prepectoral reconstruction has been noted in previous studies.3 The need for fewer prescription refills is particularly important, as each refill and week of opioid use is associated with a greater risk of misuse among opioid-naive patients than the dose itself.10 The reduction in postoperative pain with use of the prepectoral technique is consistent with previous studies, though our study is unique in directly examining opioid consumption.13
Several limitations should be noted, including the retrospective nature of this study and that duration of opioid use was patient-reported and therefore subject to reporting or recall bias. Future studies could incorporate electronic data recording applications to more precisely record the amount of narcotic taken and decrease reporting and recall bias. Furthermore, patients were instructed to take nonopioid medications for pain, as well, and it is difficult to quantify the exact dose and duration of nonopioid medication use. This may have resulted in lower opioid use, though we would not expect this to differ between groups. We did not encounter patients who developed long-term opioid dependence, though this is a risk, as described above. Longer follow-up would be needed to assess for this. Aesthetic and functional outcomes of the reconstruction were not assessed, as this was not the focus of this study. Finally, limitations of prepectoral reconstruction are worth noting. This approach may be limited in patients who desire larger implant volumes or have thin subcutaneous flaps, and may be associated with increased degrees of visible rippling.13
CONCLUSIONS
In view of the worsening opioid epidemic, it is important to develop and adopt techniques to reduce postoperative pain and opioid requirements. In this study, there was a 33% reduction in days requiring postoperative opioid pain medication in patients undergoing prepectoral breast reconstruction compared with those undergoing dual-plane reconstruction. In addition, there was a 66% reduction in the likelihood of opioid prescription refills. These results support the incorporation of prepectoral-based breast reconstruction into clinical practice. The potential need for and risks of opioid medications after surgery should be discussed with all patients preoperatively. The reduced need for opioid medications after prepectoral-based breast reconstruction is an advantage of this technique and should be considered when discussing operative approaches with patients.
Footnotes
Published online 13 February 2019.
Disclosure: Dr. Venturi is a consultant for Allergan and Stryker. Dr. Mesbahi is a consultant for Allergan. None of the other authors have any financial disclosures. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Becker H, Lind JG, 2nd, Hopkins EG. Immediate implant-based prepectoral breast reconstruction using a vertical incision. Plast Reconstr Surg Glob Open. 2015;3:e412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reitsamer R, Peintinger F. Prepectoral implant placement and complete coverage with porcine acellular dermal matrix: a new technique for direct-to-implant breast reconstruction after nipple-sparing mastectomy. J Plast Reconstr Aesthet Surg. 2015;68:162–167. [DOI] [PubMed] [Google Scholar]
- 3.Nahabedian MY, Cocilovo C. Two-stage prosthetic breast reconstruction: a comparison between prepectoral and partial subpectoral techniques. Plast Reconstr Surg. 2017;140:22S–30S. [DOI] [PubMed] [Google Scholar]
- 4.Sigalove S, Maxwell GP, Sigalove NM, et al. Prepectoral implant-based breast reconstruction: rationale, indications, and preliminary results. Plast Reconstr Surg. 2017;139:287–294. [DOI] [PubMed] [Google Scholar]
- 5.Lanier ST, Wang ED, Chen JJ, et al. The effect of acellular dermal matrix use on complication rates in tissue expander/implant breast reconstruction. Ann Plast Surg. 2010;64:674–678. [DOI] [PubMed] [Google Scholar]
- 6.Elzey MJ, Barden SM, Edwards ES. Patient characteristics and outcomes in unintentional, non-fatal prescription opioid overdoses: a systematic review. Pain Physician. 2016;19:215–228. [PubMed] [Google Scholar]
- 7.Sun EC, Darnall BD, Baker LC, et al. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016;176:1286–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305:1315–1321. [DOI] [PubMed] [Google Scholar]
- 9.Mosher H, Richardson K, Lund B. The 1-year treatment course of new opioid recipients in veterans health administration. Pain Med. 2016;17:1282–91. [DOI] [PubMed] [Google Scholar]
- 10.Brat GA, Agniel D, Beam A, et al. Postsurgical prescriptions for opioid naive patients and association with overdose and misuse: retrospective cohort study. BMJ. 2018;360:j5790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131:15–23. [DOI] [PubMed] [Google Scholar]
- 12.Vadivelu N, Schreck M, Lopez J, et al. Pain after mastectomy and breast reconstruction. Am Surg. 2008;74:285–296. [PubMed] [Google Scholar]
- 13.Cattelani L, Polotto S, Arcuri M, et al. One-step prepectoral breast reconstruction with dermal matrix-covered implant compared to submuscular implantation: functional and cost evaluation. Clin Breast Cancer. 2017:pii: . [DOI] [PubMed] [Google Scholar]
- 14.Wallace MS, Wallace AM, Lee J, et al. Pain after breast surgery: a survey of 282 women. Pain. 1996;66:195–205. [DOI] [PubMed] [Google Scholar]
- 15.Chaudhry A, Hallam S, Chambers A, et al. Improving postoperative pain management in subpectoral tissue expander implant reconstruction of the breast using an elastomeric pump. Ann R Coll Surg Engl. 2015;97:364–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glissmeyer C, Johnson W, Sherman B, et al. Effect of paravertebral nerve blocks on narcotic use after mastectomy with reconstruction. Am J Surg. 2015;209:881–883. [DOI] [PubMed] [Google Scholar]


