Figure 11.
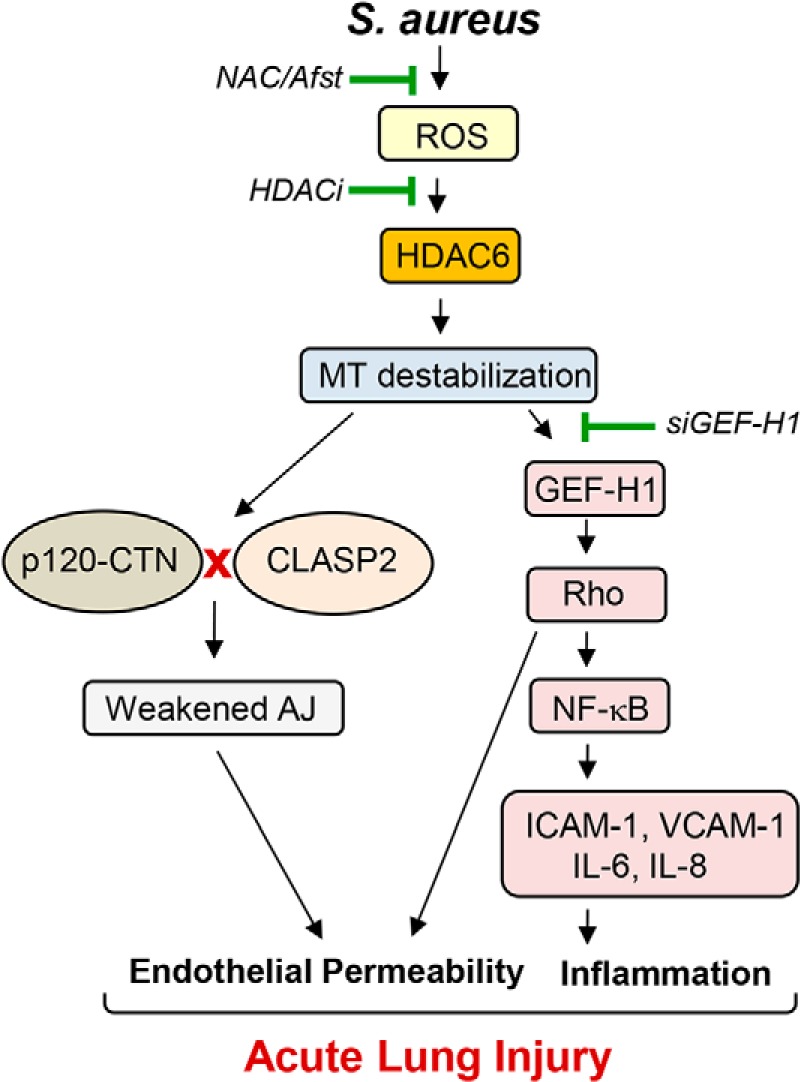
Proposed model HDAC6-dependent regulation of HKSA-induced EC permeability and inflammation. S. aureus infections generate ROS, which activates HDAC6, causing MT destabilization. Disassembly of peripheral MT structure and inhibition of MT growth to the cell periphery compromises delivery of MT-associated protein CLASP2 and its interaction with AJ proteins, leading to decreased AJ assembly and increased EC permeability. Concurrently, GEF-H1 released from destabilized MT evokes inflammation via the RhoA-dependent augmentation of NF-κB inflammatory cascade. RhoA also directly increases endothelial permeability via activation of actin cytoskeletal remodeling and actomyosin contractile mechanisms. ROS scavengers or pharmacological or genetic inhibitors of HDAC6 rescue HKSA/MRSA-induced EC permeability and inflammation by enhancing stability of MT cytoskeleton and promoting MT-dependent mechanisms of barrier protection.
