Figure 2.
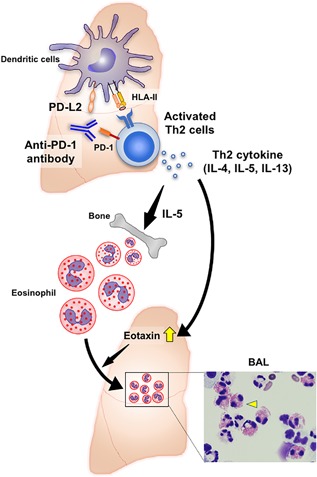
A hypothetical mechanism of the onset of AEP as an irAE in an advanced non‐small cell lung cancer patient based on the current case report and references. Antibodies against PD‐1 inhibit binding of not only PD‐L1 but also PD‐L2 to PD‐1. PD‐L2 is highly expressed on pulmonary DCs and inhibits responses of Th2 cells, which express PD‐1. The blocking the PD‐1–PD‐L2 interaction facilitates a pulmonary Th2‐type inflammation. Th2 cells predominantly produce IL‐4, IL‐5, and IL‐13, which have essential roles in the development of Th2‐associated lung diseases, enhancing the growth, differentiation, and recruitment of eosinophils. One of the Th2 cytokines, IL‐5, supports the development of eosinophils in the bone marrow. Eosinophilia in lung tissue is driven by the recruitment of eosinophils to the lung mucosa and interstitium via production of eotaxin induced by Th2 cytokines in the lung, which results in the onset of AEP as an irAE in lung cancer patients treated with an anti‐PD‐1 antibody therapy. Right lower imaging indicates a photomicrograph of representative bronchoalveolar lavage cytospin preparation, which shows eosinophilia observed in the current case. Yellow arrowhead indicates an eosinophil
