Fig. 1. Role of rCSC-EVs in RCC. Renal carcinoma contains tumoral cells (TC) that are CD105-negative and cancer stem cells (rCSCs) that are CD105-positive. Renal cancer stem cells that are CD105-positive release EVs (rCSC-EVs) that are able to promote tumor growth.
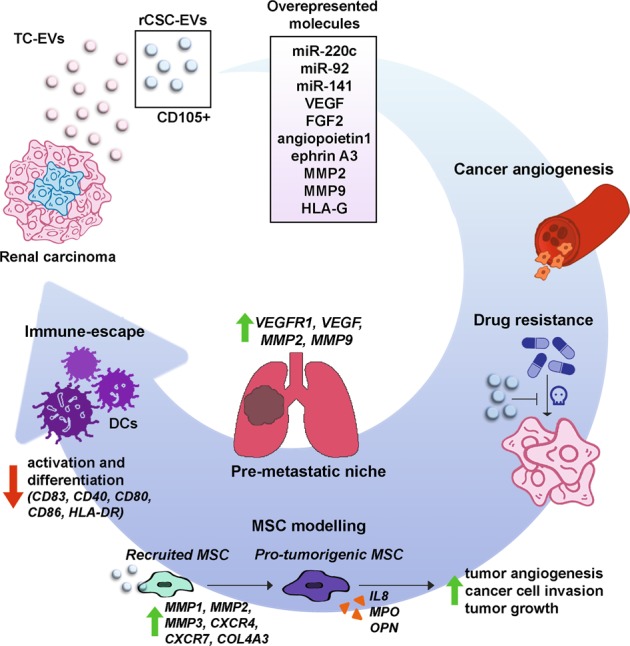
There are more than 24 upregulated miRNAs, including miR-200c miR-92 and miR-141, in CSC-EVs compared to tumoral cell-derived EVs (TC-EVs). Unlike TC-EVs, CSC-EVs carry several mRNAs of proangiogenic genes, such as VEGF, fibroblast growth factor 2 (FGF2), angiopoietin 1, ephrin A3, MMP2 and MMP9. Additionally, HLA-G protein was enriched in rCSC-EVs compared to that in TC-EVs. Moreover, rCSC-EVs support cancer development by several mechanisms. These vesicles were shown to promote tumor angiogenesis in vitro and in vivo and to promote apoptosis resistance following treatment with anticancer drug doxorubicin. Moreover, rCSC-EVs were proven to favor lung premetastatic niche formation through the upregulation of VEGFR1, VEGF, MMP2 and MMP9 in target tissue. In addition, rCSC-EVs can promote MSC migration inducing the upregulation of genes, such as MMP1, MMP3, CXCR4, MMP2, COL4A3 and CXCR7. MSCs stimulated with rCSC-EVs released IL-8, myeloperoxidase (MPO) and osteopontin (OPN) at higher concentrations, promoted cancer angiogenesis and tumor cell migration and increased tumor development in vivo. Finally, rCSC-EVs were shown to mediate cancer immunosuppression by reducing dendritic cell (DC) differentiation and activation. In particular, rCSC-EVs contained higher levels of HLA-G compared to TC-EVs and decreased the expression of activation markers CD83 and CD40, costimulatory molecules CD80 and CD86, and the antigen-presenting molecule HLA-DR in DCs
