Abstract
Background
As a member of peroxiredoxin (PRX) family, PRX3 is predominantly located in mitochondria and plays an important role of free radical scavenging. Since a body of evidence demonstrated the involvement of PRX3 in insulin secretion, insulin sensitivity, and glucose metabolism, the present study was conducted to investigate the role of PRX3 in the pathogenesis of polycystic ovarian syndrome (PCOS) featured in insulin resistance.
Methods
Enzyme-linked immunosorbent assay was performed to detect plasma PRX3 in PCOS patients and control subjects. Levels of reactive oxygen species (ROS) and oxidized PRXs were detected in mouse islet cells treated with gradient glucose.
Results
We did not find significant difference of fasting plasma PRX3 between PCOS patients and controls. No association was noticed between fasting plasma PRX3 and fasting plasma glucose or insulin. After oral glucose tolerance test (OGTT), PCOS patients showed higher levels of both glucose and insulin as compared to controls. The plasma level of PRX3 was significantly increased at 2 h and began to fall back at 3 h of OGTT. There was a one-hour time lag of peak values between plasma PRX3 and insulin, and the plasma PRX3 at 2 h was positively correlated with the insulin level at 1 h of OGTT of PCOS patients. In addition, the level of ROS was significantly elevated at 1 h and oxidized PRX3 was increased dramatically at 2 h of 16.7mM glucose stimulation in mouse islet cells.
Conclusion
It seems that PRX3 does not show its antioxidant function under baseline conditions. Instead, PRX3 responds to oxidative stress induced by rapid increase of insulin and glucose in patients with PCOS.
Keywords: Peroxiredoxin, Reactive oxygen species, Oxidative stress, Polycystic ovarian syndrome, Insulin resistance
Background
Polycystic ovarian syndrome (PCOS) is one of the most common female endocrine disorders affecting about 5–10% women of reproductive age [1]. The clinical and biochemical features include oligo/anovulation, clinical/biochemical hyperandrogenism, and polycystic ovaries. In addition, insulin resistance (IR), hyperinsulinaemia, hyperglycaemia, glucose intolerance, dyslipidaemia, and obesity are frequently found in PCOS patients [2, 3]. Although the exact etiology of PCOS remains to be unclear, oxidative stress has been associated with the pathophysiology of the disorder [4, 5], which even passes to the next generation [6]. Peroxiredoxin (PRX) is a kind of antioxidant enzyme that reduces hydrogen peroxide (H2O2) into water using its conserved cysteines. PRX3 is mainly located in mitochondria and scavenges about 90% of mitochondrial H2O2 [7], playing a critical role for mitochondrial homeostasis [8]. We previously employed PRX3-knockout mice to investigate the functional role of PRX3. Our study indicated that PRX3 was an indispensible responder to oxidative stress in inflammation, pregnancy, and malignancy [9–11]. In 2011, Huh et al. reported the occurrence of obesity of PRX3-knockout mice and mitochondrial impairment of adipocytes such as increased oxidative stress, decreased mitochondrial biogenesis, and dysregulation of enzymes involved in glucose/lipid metabolism [12].
The involvement of PRX3 in glucose metabolism could be traced back to 2008 when Chen et al. reported the improvement of glucose tolerance by PRX3 through reduction of mitochondrial H2O2 [13]. Afterwards, considerable investigations demonstrated the role of PRX3 in glucose tolerance, insulin secretion, and IR. PRX3 protected pancreatic β cells from apoptosis to maintain insulin secretion [14]. More importantly, PRX3 plays a key role in maintaining mitochondrial homeostasis and increasing insulin sensitivity. PRX3-deficiency in mice exhibited metabolic disorders including impaired glucose tolerance, increased IR, and obesity. Further study showed elevated oxidative stress and down-regulation of fatty acid metabolism-ralated proteins in adipocyte, resulting in fat accumulation of PRX3-knockout mice [12]. Moreover, genetic variations or decreased expression of PRX3 were recognized in humans with obesity [12, 15]. Since a large proportion of patients with PCOS present obesity and IR, the present study is conducted to link plasma PRX3 with IR of PCOS patients.
Methods
Patients
After approval by the Ethics Committee of Binzhou Medical University (Yantai, China), we obtained written consent from all participants. The diagnostic criteria of PCOS were based on the revised Rotterdam consensus [16] including any two of the following three clinical features: (1) oligo/anovulation, (2) clinical and/or biochemical hyperandrogenism, and (3) polycystic ovaries on ultrasound. Women with other related disorders such as adrenal congenital hyperplasia, thyroid disease, Cushing’s syndrome, or androgen-secreting tumors were excluded.
Definitions of obesity and calculation of IR
The body mass index (BMI) ≥28 was identified as obesity according to the diagnostic criteria for obesity in the Asia-Pacific region issued by World Health Organization (WHO) [17]. Homeostasis model assessment of IR (HOMA-IR) was calculated by fasting plasma glucose (FPG) × fasting insulin (FINS)/22.5.
Oral glucose tolerance test (OGTT)
Fasting blood samples were collected from the antecubital vein of the subjects on the second or third day of the menstrual cycle. In addition to routine examination of reproductive hormones including follicle stimulating hormone (FSH), luteinizing hormone (LH), estradiol (E2), prolactin (PRL), and testosterone (T), a 75-g OGTT was performed to detect the changes of plasma glucose, insulin, and PRX3 at the time points 1 h, 2 h, and 3 h respectively. The plasma level of PRX3 was detected by enzyme-linked immunosorbent assay (ELISA). The kit for ELISA was purchased from NeoScientific (MA, USA) and the experiment was performed according to the manufacturer’s instruction. We assayed duplicates of each sample and measured the absorbance at 450 nm on a spectrophotometer.
Glucose stimulation of mouse islet cells
The Beta-TC-6 mouse islet cell line was purchased from the Cell Bank of Chinese Academy of Sciences (Shanghai, China) and maintained in Dulbecco’s modified Eagle’s medium containing 15% fetal bovine serum, 100 U/L streptomycin, and 100 U/L penicillin. After obtaining enough cells, we re-cultured the cells in six-well plates. Two days later when the cell confluence reached more than 80%, we changed the medium as Krebs-Ringer Bicarbonate Buffer (KRBB: 129 mM NaCL, 4 .8mM KCL, 1 .2mM MgSO4, 1 .2mM KH2PO4, 2 .5mM CaCL2, 5 mM NaHCO3, 0.1% BSA, and 10 mM HEPES. pH: 7.4) containing 2 .8mM glucose and 2 μM 2′,7′-dichlorofluorescin diacetate (DCFH-DA, Molecular Probes). After incubation at 37 °C for 30 min, we applied KRBB containing glucose at 2 .8mM, 5 .6mM, and 16.7mM respectively. The level of reactive oxygen species (ROS) in cultured supernatants was estimated at the indicated time points through the oxidation of DCFH-DA using a fluorescent measurement system (Cytofluor 2350, Millipore, MA, USA) at 504 nm excitation and 524 nm emission. In addition, the level of oxidized two-cysteine PRXs in the mouse islet cells was detected by Western Blotting using rabbit polyclonal Anti-Peroxiredoxin-SO3 antibody (ab16830, Abcam, MA, USA).
Statistical analysis
Software SPSS 20.0 was used for statistical analysis. The blood levels of glucose, insulin and PRX3 were compared between the two groups by t test. The rate of obesity between the two groups was compared by Chi-square analysis. The ROS level in cultured mediums of mouse islet cells was compared by analysis of variance. The association between plasma PRX3 and glucose or insulin was performed by Spearman correlation analysis. P < 0.05 was considered to be statistically significant.
Results
General information
We included fifty PCOS patients in the present study, and fifty-six infertile patients without PCOS were used as controls. As indicated in Table 1, there was no significant difference of age and FPG between the two groups. The levels of LH and T were significantly higher in PCOS patients than in controls. The obesity rate, the levels of BMI, FINS, and HOMA-IR were significantly higher in PCOS patients than in controls. We did not find significant difference of plasma PRX3 between PCOS patients and controls (Table 2).
Table 1.
Comparison of reproductive hormones between PCOS patients and controls
| Age | FSH (U/L) | LH (U/L) | E2 (pmol/L) | PRL (nmol/L) | T (nmol/L) | |
|---|---|---|---|---|---|---|
| PCOS | 29.0 ± 3.0 | 4.45 ± 0.2 | 5.73 ± 0.4 | 129 ± 9.5 | 808 ± 62 | 1.71 ± 0.1 |
| Control | 30.8 ± 4.4 | 5.24 ± 0.2 | 3.62 ± 0.1 | 112 ± 5.5 | 670 ± 27 | 0.98 ± 0.04 |
| t values | 1.346 | 0.156 | 2.901 | 0.901 | 1.758 | 3.480 |
| P values | 0.197 | 0.877 | 0.006a | 0.377 | 0.085 | 0.002a |
asignificant difference
Table 2.
Comparison of general information between PCOS patients and controls
| Obesity (%) | BMI | FPG (mmoL/L) | FINS (mU/L) | HOMA-IR | PRX3 (ng/ml) | |
|---|---|---|---|---|---|---|
| PCOS | 52.0 | 28.9 ± 4.4 | 6.1 ± 1.2 | 18.7 ± 1.3 | 4.7 ± 0.2 | 29.5 ± 3.8 |
| Control | 10.7 | 23.2 ± 3.3 | 5.6 ± 0.5 | 11.2 ± 0.6 | 2.7 ± 0.1 | 29.3 ± 3.4 |
| t (χ2) values | 10.68 | 5.334 | 1.559 | 2.833 | 2.575 | 0.107 |
| P values | 0.001a | < 0.001a | 0.119 | 0.005a | 0.010a | 0.915 |
asignificant difference
To further understand the difference of plasma PRX3 between PCOS patients and controls, we sub-grouped the subjects according to the IR and BMI respectively. Subjects with IR ≥2.69 were divided into high IR sub-group, while the subjects with IR < 2.69 were divided into low IR sub-group. Obese PCOS patients with high IR (PCOS-IRH-Obese) were respectively compared to lean PCOS patients with low IR (PCOS-IRL-Lean) and lean controls with low IR (Control-IRL-Lean). As indicated in Table 3, there was no significant difference of plasma PRX3 between PCOS-IRH-Obese patients and Control-IRL-Lean subjects. The plasma level of PRX3 was slightly lower in PCOS-IRL-Lean patients than in PCOS-IRH-Obese patients but did not reach statistical significance.
Table 3.
IR and BMI-based comparison of PCOS patients and controls
| n | Age | BMI | FPG (mmoL/L) | FINS (mU/L) | HOMA-IR | PRX3 (ng/ml) | |
|---|---|---|---|---|---|---|---|
| Control-IRL -Lean | 28 | 29.6 ± 4.4 | 20.9 ± 3.3 | 5.3 ± 0.5 | 7.7 ± 0.6 | 1.8 ± 0.1 | 29.8 ± 3.4 |
| t values | 0.397 | 7.534 | 2.580 | 7.961 | 4.962 | 0.156 | |
| P values | 0.695 | < 0.001a | 0.02a | < 0.001a | < 0.001a | 0.877 | |
| PCOS-IRH -Obese | 22 | 29.3 ± 3.0 | 31.4 ± 3.1 | 6.7 ± 1.5 | 29.3 ± 10.5 | 9.2 ± 5.2 | 30.4 ± 3.6 |
| t values | −1.093 | 4.315 | 2.661 | 6.001 | 4.646 | 1.154 | |
| P values | 0.293 | 0.001a | 0.02a | < 0.001a | 0.001a | 0.268 | |
| PCOS-IRL -Lean | 10 | 31 ± 2.6 | 24.8 ± 2.0 | 5.3 ± 0.4 | 9.0 ± 2.6 | 1.9 ± 0.5 | 25.1 ± 2.7 |
asignificant difference
Changes of plasma glucose, insulin, and PRX3 in OGTT
We performed OGTT to understand the changes of plasma glucose, insulin, and PRX3 in PCOS patients. The plasma glucose in PCOS patients was significantly higher than in control patients at 1 h, 2 h, and 3 h (Fig. 1a), while the plasma insulin in PCOS patients was significantly higher than in controls at 0 h, 1 h, and 3 h respectively (Fig. 1b). As illustrated in Fig. 1c, the level of plasma PRX3 in PCOS patients reached its peak at 2 h (2 h vs 0 h: t = 4.421, P < 0.001) and began to fall back at the time point of 3 h (3 h vs 0 h: t = 3.560, P = 0.001). The plasma PRX3 in control subjects was increased at 2 h (2 h vs 0 h: t = 3.270, P = 0.002) and fell back to the level comparable to the baseline at 3 h (3 h vs 0 h: t = 0.570, P = 0.575). There was significant difference of plasma PRX3 between the two groups at the time points of 2 h and 3 h (Fig. 1c).
Fig. 1.
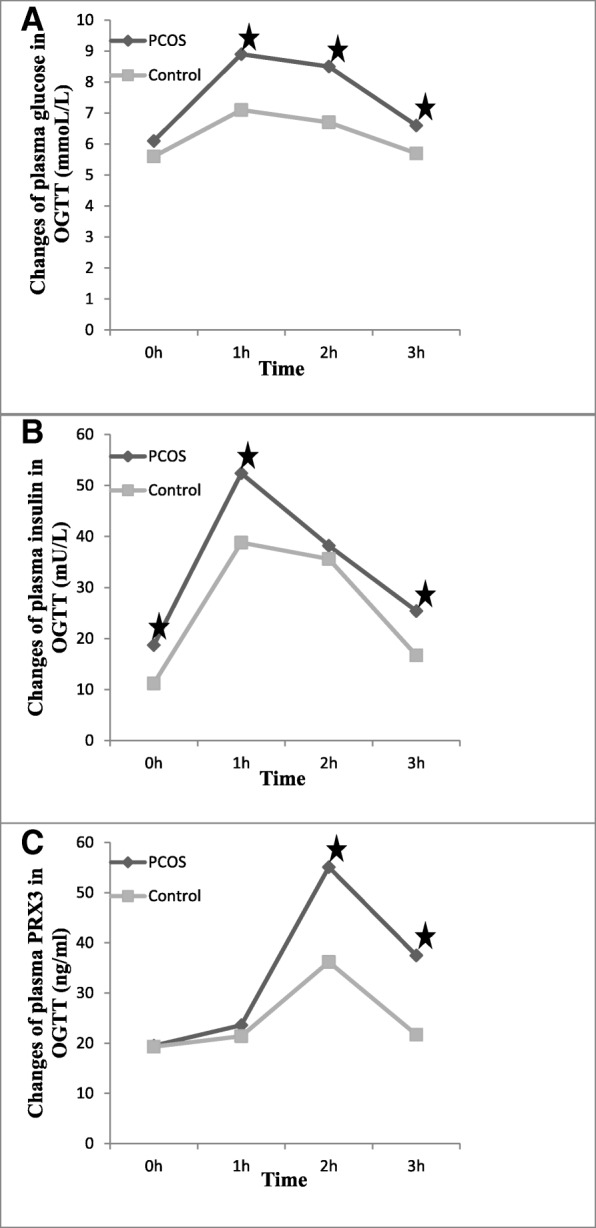
Changes of plasma glucose, insulin, and PRX3 in PCOS patients and controls undergoing OGTT. a Plasma glucose reached its peak at 1 h and began to fall back at 2 h. There was significant difference between PCOS patients and controls respectively at 1 h (t = 2.901, P = 0.006), 2 h (t = 2.578, P = 0.034), and 3 h (t = 2.772, P = 0.045). b The change pattern of plasma insulin was as the same as glucose in both PCOS patients and controls. The plasma insulin in PCOS patients was significantly higher than in controls respectively at 0 h (t = 2.833, P = 0.005), 1 h (t = 3.480, P = 0.002), and 3 h (t = 2.321, P = 0.046). c Plasma PRX3 reached its peak at 2 h (one hour later than the insulin peak) and began to fall back at 3 h. There was significant difference between the two groups at 2 h (t = 2.794, P = 0.012 and 3 h (t = 2.568, P = 0.039) respectively
The association of plasma PRX3 with plasma glucose and insulin
We applied the Spearman correlation analysis to understand the relationship of plasma PRX3 with plasma glucose and insulin. As indicated in Table 4, we did not find significant association of fasting plasma PRX3 with BMI, FPG, FINS, and HOMA-IR in either PCOS patients or control subjects. Interestingly, the plasma PRX3 at 2 h was positively correlated to the insulin level of 1 h in OGTT of PCOS patients (r = 0.451, P = 0.031).
Table 4.
The association of fasting plasma PRX3 with BMI, FPG, FINS, and HOMA-IR
| BMI | FPG | FINS | HOMA-IR | |||||
|---|---|---|---|---|---|---|---|---|
| r values | P values | r values | P values | r values | P values | r values | P values | |
| PCOS | 0.383 | 0.058 | 0.075 | 0.720 | 0.352 | 0.084 | 0.170 | 0.415 |
| Control | −0.268 | 0.169 | −0.056 | 0.778 | 0.207 | 0.292 | −0.094 | 0.634 |
Levels of ROS and oxidized PRXs in mouse islet cell
To confirm the role of PRX3 in the response to insulin releasing, we detected the levels of ROS and oxidized PRXs in mouse islet cells treated with gradient concentrations of glucose. As shown in Fig. 2, oxidized PRXs were increased in a glucose concentration-dependent manner, and the signal for PRX3-SO3H was dramatically enhanced at 2 h of 16.7mM glucose stimulation as compared to 5 .6mM glucose stimulation (Fig. 2a and b). There was no significant difference in ROS production between 5 .6mM glucose stimulation and non-treated cells, while the ROS production in mouse islet cells stimulated with 16.7mM glucose was significantly elevated at 1 h, 2 h, and 3 h respectively (Fig. 2c).
Fig. 2.
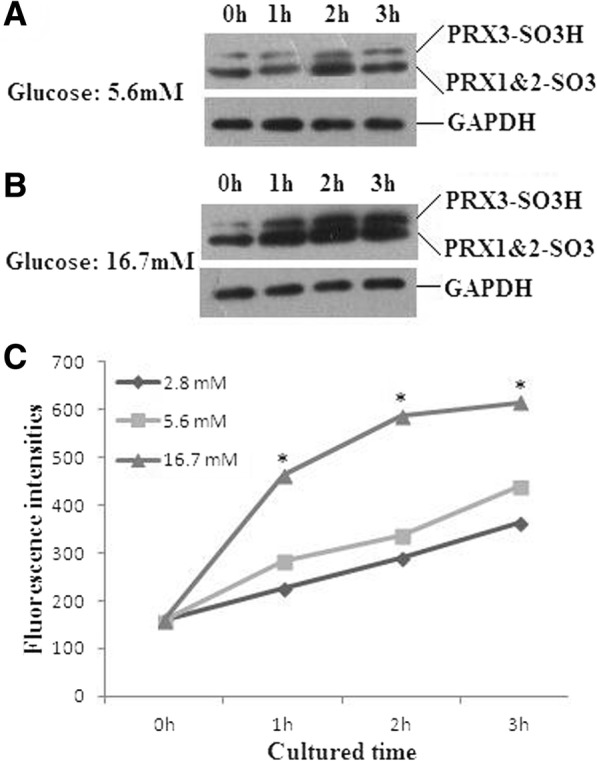
Levels of ROS and oxidized PRXs in mouse islet cells treated with glucose. a and b Oxidized PRXs were increased in a glucose concentration-dependent manner, and the signal for PRX3-SO3H was dramatically enhanced at 2 h of 16.7mM as compared to 5 .6mM glucose stimulation. c ROS production in mouse islet cells stimulated with 16.7mM glucose was significantly elevated at 1 h, 2 h, and 3 h respectively (*1 h: F = 4.641, P < 0.001; 2 h: F = 4.353, P < 0.001; 3 h: F = 3.460, P < 0.001). There was no significant difference in ROS production between 5 .6mM glucose stimulation and non-treated cells
Discussion
In the present study, we examined the plasma level of PRX3 and did not find significant difference between PCOS patients and controls. However, the plasma PRX3 was dramatically increased in the insulin releasing test, especially in PCOS patients. There was a one-hour time lag of peak values between plasma PRX3 and insulin, and the positive correlation of plasma PRX3 with insulin suggests PRX3 to be an indicator of a short sharp release of insulin.
Although the etiology of PCOS has not been well known, IR and/or hyperinsulinemia are considered to play a key role in the pathophysiology of PCOS [18]. High levels of glucose and insulin can cause oxidative stress and have significant negative impacts on the mitochondrial homeostasis of islet beta cells [19, 20], forming a vicious circle in the pathogenesis of PCOS [21–23]. In the present study, we did not notice significant increase of fasting plasma PRX3 in PCOS patients. Since the plasma level of PRX3 was increased in the OGTT of both PCOS patients and controls, we suppose that PRX3 responds to the oxidative stress induced by rapid insulin release. Our in vitro detection showed elevated ROS and oxidized PRX3 in glucose treated mouse islet cells, which resembled the changes of plasma PRX3 in the subjects undergoing OGTT and provided strong support for the hypothesis. Another contributory factor for the elevated plasma PRX3 would be the existence of inflammatory state in patients with PCOS. Previous studies demonstrated high levels of inflammatory markers such as C-reactive protein or proinflammatory cytokines such as tumor necrosis factor α and interleukin-6 in peripheral leukocytes of PCOS patients, which contribute in turn to the induction of oxidative stress and IR [24, 25]. Furthermore, acute hyperglycemia stimulated an increase of ROS generation by leukocytes of PCOS patients [26, 27]. The present study showed higher plasma glucose in PCOS patients at 1 h, 2 h, and 3 h of OGTT as compared to control subjects. Increased plasma PRX3 might represent at least partially a response to an augmented oxidative stress of circulating leukocytes.
According to the previous reports, other PRX members including PRX1, PRX2, PRX4, and PRX6 respond actively to glucose and/or insulin-related oxidative stress [28–30]. In the present study using mouse islet cells, the oxidation of PRX3 was quite fewer as compared to that of PRX1 and/or PRX2 under basal conditions. However, oxidized PRX3 was significantly increased after glucose stimulation, along with the increase of oxidized PRX1 and/or PRX2. Another study conducted by Al-Masri et al. showed higher plasma levels of PRX1, PRX2, PRX4, and PRX6 in patients with type 2 diabetes than in control subjects. The plasma PRX1 in well-controlled diabetic patients fell back to the value comparable to that of non-diabetic controls, while PRX2, PRX4, and PRX6 remained to be at high level in both well-controlled and poorly-controlled diabetic patients [28]. These results suggested a cooperative response of PRX members to glucose-induced oxidative stress on the one hand and different responding patterns on the other. It seems that PRX2, PRX4, and PRX6 performed their antioxidant function in a routine manner, while PRX3 would emerge as a ROS scavenger under urgent or severe oxidative stress. In fact, most of the previous studies on the involvement of PRX3 in glucose metabolism/IR were conducted with several stressors or transgenic animals instead of “natural conditions” [13, 14, 27].
Conclusions
In conclusion, the present results have provided evidence that PRX3 plays an essential role in the response to oxidative stress induced by rapid increase of glucose and insulin. Detection of plasma PRX3 would be useful for the evaluation of IR in PCOS patients.
Acknowledgements
Not applicable.
Funding
This study was funded by the Key Research and Development Program of Shandong Province (grant number 2018GSF118190).
Availability of data and materials
All data generated or analysed during this study are included in this published article and are available from the corresponding author on reasonable request.
Abbreviations
- BMI
Body mass index
- DCFH-DA
2′,7′-dichlorofluorescin diacetate
- ELISA
Enzyme-linked immunosorbent assay
- FINS
Fasting insulin
- FPG
Fasting plasma glucose
- H2O2
Hydrogen peroxide
- HOMA-IR
Homeostasis model assessment of IR
- IR
Insulin resistance
- KRBB
Krebs-Ringer bicarbonate buffer
- OGTT
Oral glucose tolerance test
- PCOS
Polycystic ovarian syndrome
- PRX
Peroxiredoxin
- ROS
Reactive oxygen species
Authors’ contributions
LHL collected blood samples and detected plasma glucose/insulin. LTT performed Western Blot analysis. YAQ performed statistical analysis. LJ and LX performed cell culture and ELISA. LL analyzed and interpreted the patient data, and was a major contributor in writing the manuscript. KT gave critical comments to the research. All authors read and approved the final manuscript.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Binzhou Medical University. The reference number is 2017–037 and the date of approval is 2017-9-26. Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Lianqin Li, Email: lilq2005@126.com.
Tomonori Kaifu, Email: kaifu@tohoku-mpu.ac.jp.
References
- 1.Azziz R, Woods KS, Reyna R, Key TJ, Knochenhauer ES, Yildiz BO. The prevalence and features of the polycystic ovary syndrome in an unselected population. J Clin Endocrinol Metab. 2004;89:2745–2749. doi: 10.1210/jc.2003-032046. [DOI] [PubMed] [Google Scholar]
- 2.Franks S. Polycystic ovary syndrome: a changing perspective. Clin Endocrinol. 1989;31:87–120. doi: 10.1111/j.1365-2265.1989.tb00457.x. [DOI] [PubMed] [Google Scholar]
- 3.Azziz R, Carmina E, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Futterweit W, Janssen OE, Legro RS, Norman RJ, Taylor AE, Witchel SF. Task force on the phenotype of the polycystic ovary syndrome of the androgen excess and PCOS society.: the androgen excess and PCOS society criteria for the polycystic ovary syndrome: the complete task force report. Fertil Steril. 2009;91:456–488. doi: 10.1016/j.fertnstert.2008.06.035. [DOI] [PubMed] [Google Scholar]
- 4.Murri M, Luque-Ramirez M, Insenser M, Ojeda-Ojeda M, Escobar-Morreale HF. Circulating markers of oxidative stress and polycystic ovary syndrome (PCOS): a systematic review and meta-analysis. Hum Reprod Update. 2013;19:268–288. doi: 10.1093/humupd/dms059. [DOI] [PubMed] [Google Scholar]
- 5.Hyderali BN, Mala K. Oxidative stress and cardiovascular complications in polycystic ovarian syndrome. Eur J Obstet Gynecol Reprod Biol. 2015;191:15–22. doi: 10.1016/j.ejogrb.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Boutzios G, Livadas S, Piperi C, Vitoratos N, Adamopoulos C, Hassiakos D, Iavazzo C, Diamanti-Kandarakis E. Polycystic ovary syndrome offspring display increased oxidative stress markers comparable to gestational diabetes offspring. Fertil Steril. 2013;99:943–950. doi: 10.1016/j.fertnstert.2012.10.050. [DOI] [PubMed] [Google Scholar]
- 7.Cox AG, Winterbourn CC, Hampton MB. Mitochondrial peroxiredoxin involvement in antioxidant defence and redox signaling. Biochem J. 2009;425:313–325. doi: 10.1042/BJ20091541. [DOI] [PubMed] [Google Scholar]
- 8.Wonsey DR, Zeller KI, Dang CV. The c-Myc target gene PRDX3 is required for mitochondrial homeostasis and neoplastic transformation. Proc Natl Acad Sci U S A. 2002;99:6649–6654. doi: 10.1073/pnas.102523299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li L, Shoji W, Oshima H, Obinata M, Fukumoto M, Kanno N. Crucial role of peroxiredoxin III in placental antioxidant defense of mice. FEBS Lett. 2008;582:2431–2434. doi: 10.1016/j.febslet.2008.05.050. [DOI] [PubMed] [Google Scholar]
- 10.Li L, Shoji W, Takano H, Nishimura N, Aoki Y, Takahashi R, Goto S, Kaifu T, Takai T, Obinata M. Increased susceptibility of peroxiredoxin III knockout mice to oxidative stress. Biochem Biophys Res Commun. 2007;355:715–721. doi: 10.1016/j.bbrc.2007.02.022. [DOI] [PubMed] [Google Scholar]
- 11.Li L, Zhang YG, Chen CL. Anti-apoptotic role of peroxiredoxin III in cervical cancer cells. FEBS Open Bio. 2013;3:51–54. doi: 10.1016/j.fob.2012.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huh JY, Kim Y, Jeong J, Park J, Kim I, Huh KH, Kim YS, Woo HA, Rhee SG, Lee KJ, Ha H. Peroxiredoxin 3 is a key molecule regulating adipocyte oxidative stress, mitochondrial biogenesis, and adipokine expression. Antioxid Redox Signal. 2012;16:229–243. doi: 10.1089/ars.2010.3766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen L, Na R, Gu M, Salmon AB, Liu Y, Liang H, Qi W, Van Remmen H, Richardson A, Ran Q. Reduction of mitochondrial H2O2 by overexpressing peroxiredoxin 3 improves glucose tolerance in mice. Aging Cell. 2008;7:866–878. doi: 10.1111/j.1474-9726.2008.00432.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wolf G, Aumann N, Michalska M, Bast A, Sonnemann J, Beck JF, Lendeckel U, Newsholme P, Walther R. Peroxiredoxin III protects pancreatic β cells from apoptosis. J Endocrinol. 2010;207:163–175. doi: 10.1677/JOE-09-0455. [DOI] [PubMed] [Google Scholar]
- 15.Hiroi M, Nagahara Y, Miyauchi R, Misaki Y, Goda T, Kasezawa N, Sasaki S, Yamakawa-Kobayashi K. The combination of genetic variations in the PRDX3 gene and dietary fat intake contribute to obesity risk. Obesity (Silver Spring) 2011;19:882–887. doi: 10.1038/oby.2010.275. [DOI] [PubMed] [Google Scholar]
- 16.Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS) Hum Reprod. 2004;19:41–47. doi: 10.1093/humrep/deh098. [DOI] [PubMed] [Google Scholar]
- 17.Report of a WHO Consultation. Obesity: preventing and managing the global epidemic. WHO Tech Rep Ser. 2000;894:1–253. [PubMed]
- 18.Svendsen PF, Nilas L, Nørgaard K, Jensen JE, Madsbad S. Obesity, body composition and metabolic disturbances in polycystic ovary syndrome. Hum Reprod. 2008;23:2113–2121. doi: 10.1093/humrep/den211. [DOI] [PubMed] [Google Scholar]
- 19.Ceriello A, dello Russo P, Amstad P, Cerutti P. High glucose induces antioxidant enzymes in human endothelial cells in culture. Evidence linking hyperglycemia and oxidative stress. Diabetes. 1996;45:471–477. doi: 10.2337/diab.45.4.471. [DOI] [PubMed] [Google Scholar]
- 20.Bell RC, Carlson JC, Storr KC, Herbert K, Sivak J. High-fructose feeding of streptozotocin-diabetic rats is associated with increased cataract formation and increased oxidative stress in the kidney. Br J Nutr. 2000;84:575–582. [PubMed] [Google Scholar]
- 21.Victor VM, Rovira-Llopis S, Bañuls C, Diaz-Morales N, Martinez de Marañon A, Rios-Navarro C, Alvarez A, Gomez M, Rocha M, Hernández-Mijares A. Insulin resistance in PCOS patients enhances oxidative stress and leukocyte adhesion: role of myeloperoxidase. PLoS One. 2016;11:e0151960. doi: 10.1371/journal.pone.0151960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen L, Xu WM, Zhang D. Association of abdominal obesity, insulin resistance, and oxidative stress in adipose tissue in women with polycystic ovary syndrome. Fertil Steril. 2014;102:1167–1174. doi: 10.1016/j.fertnstert.2014.06.027. [DOI] [PubMed] [Google Scholar]
- 23.Enli Y, Fenkci SM, Fenkci V, Oztekin O. Serum fetuin-a levels, insulin resistance and oxidative stress in women with polycystic ovary syndrome. Gynecol Endocrinol. 2013;29:1036–1039. doi: 10.3109/09513590.2013.829442. [DOI] [PubMed] [Google Scholar]
- 24.Victor VM, Rocha M, Bañuls C, Sanchez-Serrano M, Sola E, Gomez M, Hernandez-Mijares A. Mitochondrial complex I impairment in leukocytes from polycystic ovary syndrome patients with insulin resistance. J Clin Endocrinol Metab. 2009;94:3505–3512. doi: 10.1210/jc.2009-0466. [DOI] [PubMed] [Google Scholar]
- 25.Victor VM, Rocha M, Bañuls C, Alvarez A, de Pablo C, Sanchez-Serrano M, Gomez M, Hernandez-Mijares A. Induction of oxidative stress and human leukocyte/endothelial cell interactions in polycystic ovary syndrome patients with insulin resistance. J Clin Endocrinol Metab. 2011;96:3115–3122. doi: 10.1210/jc.2011-0651. [DOI] [PubMed] [Google Scholar]
- 26.González F, Rote NS, Minium J, Kirwan JP. Reactive oxygen species-induced oxidative stress in the development of insulin resistance and hyperandrogenism in polycystic ovary syndrome. J Clin Endocrinol Metab. 2006;91:336–340. doi: 10.1210/jc.2005-1696. [DOI] [PubMed] [Google Scholar]
- 27.Arkat S, Umbarkar P, Singh S, Sitasawad SL. Mitochondrial Peroxiredoxin-3 protects against hyperglycemia induced myocardial damage in diabetic cardiomyopathy. Free Radic Biol Med. 2016;97:489–500. doi: 10.1016/j.freeradbiomed.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 28.Al-Masri AA, El Eter E, Tayel S, Zamil H. Differential associations of circulating peroxiredoxins levels with indicators of glycemic control in type 2 diabetes mellitus. Eur Rev Med Pharmacol Sci. 2014;18:710–716. [PubMed] [Google Scholar]
- 29.Pacifici F, Arriga R, Sorice GP, Capuani B, Scioli MG, Pastore D, Donadel G, Bellia A, Caratelli S, Coppola A, Ferrelli F, Federici M, Sconocchia G, Tesauro M, Sbraccia P, Della-Morte D, Giaccari A, Orlandi A, Lauro D. Peroxiredoxin 6, a novel player in the pathogenesis of diabetes. Diabetes. 2014;63:3210–3220. doi: 10.2337/db14-0144. [DOI] [PubMed] [Google Scholar]
- 30.Gateva A, Assyov Y, Velikova T, Kamenov Z. Increased peroxiredoxin 4 levels in patients with prediabetes compared to normal glucose tolerance subjects. Clin Endocrinol. 2016;85:551–555. doi: 10.1111/cen.13135. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article and are available from the corresponding author on reasonable request.


