Fig. 4.
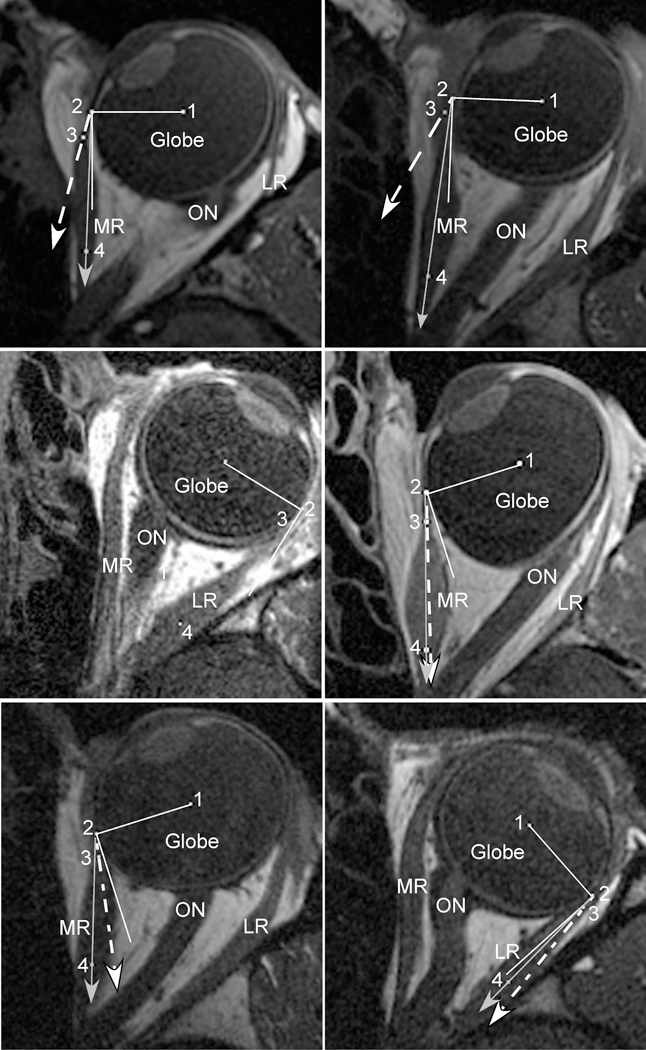
Axial magnetic resonance imaging (MRI) in strabismic subjects maintaining large ipsiversive ductions. In each panel, the solid white line represents a perfect tangent to the globe. The dashed white line with arrow represents the measured angle at tendon insertion. The solid gray line with arrow represents the predicted angle based on the “arc of contact” model. Point (1) marks the globe center, (2) the extraocular muscle insertion (EOM), (3) the middle of the immediate posterior tendon path, and (4) the middle of the posterior EOM belly. Upper Left) Subject with lateral rectus (LR) palsy. Because of the large esotropia created by the palsy, the medial rectus (MR) insertion (2) is near the equator of the globe. In this position, however, the curvilinear MR path and thickened posterior belly creates a much larger loss of tangency than predicted by the “arc of contact” model. Upper Right) Subject who had undergone prior medial rectus (MR) resection. Similarly, after MR resection, the thickened insertion creates a much larger loss of tangency during adduction than predicted by the “arc of contact” model. Center Left) Subject who had undergone prior LR recession. The measured angle at tendon insertion demonstrates perfect tangency with the globe during abduction, identical to the “arc of contact” model. Center Right) Subject who had undergone prior MR recession. The measured angle at tendon insertion is nearly identical to the predicted angle from the “arc of contact” model. The combination of recession and adduction has rotated the insertion (2) posterior to globe center, plus the recessed MR has a thinned tendon and a nearly linear path towards its insertion, creating a near perfect agreement between predicted and measured angles. Lower Left) Subject who had undergone prior MR posterior fixation. Similar to MR recession, the posterior fixation suture has moved the effective MR insertion (2) posterior to globe center during adduction. Because the posterior muscle path deflects inward towards the center of the orbit, however, the measured angle at tendon insertion is closer to globe tangency than predicted. This MRI demonstrates the only scenario where the “arc of contact” model predicted a much greater loss of globe tangency than was actually measured. Lower Right) Subject who had undergone prior LR posterior fixation. The measured angle at tendon insertion was slightly larger than predicted by the “arc of contact” model, but the loss of tangency was much less than observed after MR posterior fixation. LR = Lateral Rectus; MR = Medial Rectus; ON = Optic Nerve
