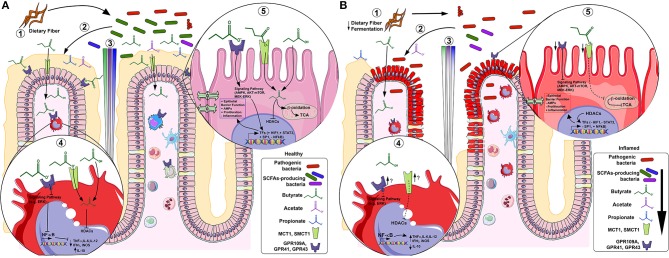
Figure 2.
SCFAs in healthy (A) and inflamed (B) colonic mucosa. In healthy mucosa, (1) bacterial fermentation of dietary fiber (DF) by SCFAs-producing bacteria (e.g., F. prausnitzii), increases luminal content of butyrate (green), propionate (blue) and acetate (purple) (2), forming a gradient along the crypt. In lamina propria (LP) macrophages under acute inflammatory stimulus (4), butyrate inhibits histone deacetylases (HDACs) thus; NF-κB-induced pro-inflammatory mediators (e.g. TNF-α, IL-6, IL-12 and iNOS) expression whereas increases anti-inflammatory mediators (e.g., IL-10). In colonocytes (5), butyrate is β-oxidized to Acetyl-CoA and constitutes the main source of energy by entering the TCA cycle. Alternatively, butyrate initiates signaling pathway activation (or repression) by GPCRs and/or directly inhibits HDACs, thus activating (e.g., HIF-1, STAT3 and SP1) or repressing (e.g., NF-κB) transcription factors (TFs), increasing epithelial barrier function, antimicrobial peptides (AMPs) production, cell proliferation and decreasing inflammation. In inflamed mucosa as IBD, (1) a decreased fermentation of DF by low levels of SCFAs-producing bacteria (e.g., F. prausnitzii) (2), reduces SCFAs luminal content (3). In LP inflammatory macrophages (4), butyrate-GPCRs activation and -HDACs inhibition are downregulated, thus, there is uncontrolled NF-κB-induced pro-inflammatory mediators' expression (e.g. TNF-α, IL-6, IL-12 and iNOS) and decrease of anti-inflammatory mediators (e.g., IL-10), although it appears that the inflammation increasesthe GPCRs and transporters expression. In inflamed colonocytes (5), butyrate uptake and oxidation are decreased and GPCRs and transporters are also downregulated. This contributes to decreased epithelial barrier integrity, AMPs production, cell proliferation and increased inflammation.