Figure 3.
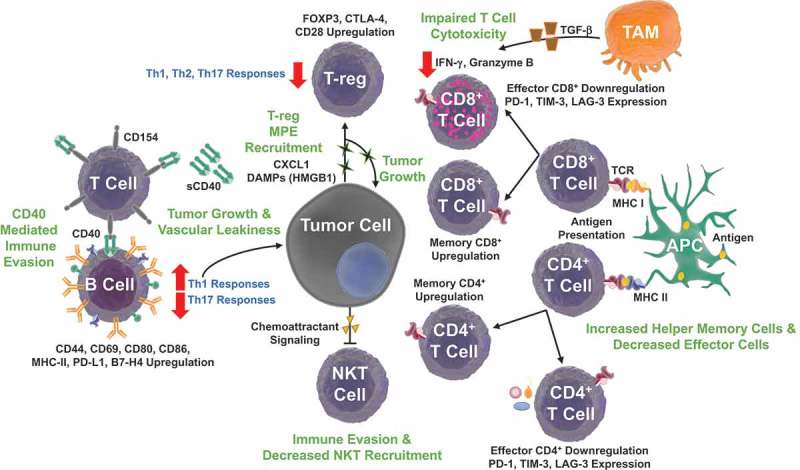
Adaptive immune signaling pathways in malignant pleural effusions. The immunosuppressive MPE environment modulates the ‘adaptome’, B, NKT, αβ T cell and γδ T lymphocyte biology to promote tumor growth and immune evasion. Tumor cells secrete chemokine ligand 1 (CXCL1) and DAMPs, promoting further cell proliferation and T-regulatory (T-reg) cell recruitment. T-regs promote an immunosuppressive environment, inhibiting Th1, Th2, Th9, and Th17 responses. Moreover, T lymphocytes display a high CD4+/CD8+ ratio with an increased percentage of central memory CD4+ T cells and decreased CD8+ effector-memory T cells. T cell programmed cell death protein 1 (PD-1), T cell immunoglobulin and mucin domain 3 (TIM-3), and Lymphocyte-activation gene 3 (LAG-3) immune checkpoint expression inhibit lymphocyte activity. Tumor Associated Macrophage (TAM) transforming growth factor beta (TGF-β) production decreases effector T cell cytotoxicity with reduced production of interferon gamma (IFN-γ) and granzyme B. These changes are accompanied with decreased NKT recruitment to the effusion site. Increased soluble CD40 (sCD40) levels inhibit B cell function by competing for CD154 (CD40 ligand) on T lymphocytes. Despite decreased B cell density, increased expression of CD80, CD86, MHC II, CD44, CD69, and programmed death ligand 1 (PD-L1) promote Th2 responses that can also support MPE formation.
