Abstract
Purpose
The objective of our cross-sectional study is to explore the adherence behavior of patients with type 2 diabetes mellitus (T2DM) by examining the association between the various types of adherence. The success of diabetic therapy partly relies on patient motivation, psych-odemographic variables (self-efficacy, health literacy, and health locus of control [HLOC]), and adherence. The aim of our research was to explore the attitudes of T2DM patients toward medication and lifestyle therapy, thus gaining a deeper insight into the role of adherence-determining parameters in disease management.
Patients and methods
The sample for the present study consisted of 113 T2DM inpatients (75 women and 38 men) with a mean age of 60.56 years (SD=12.94, range: 20–85 years) diagnosed with T2DM for an average of 13 years (SD=8.23). Participants completed the Diabetes Adherence Questionnaire conceptualized by the research team in accordance with the mapping of psychological and psychosocial parameters. We examined the associations between variables using Spearman’s rank correlation. Multivariate regression analysis was used to examine predictive variables for adherent behavior. In addition, we attempted to examine factors with a negative effect on adherence using factor analysis.
Results
Based on our results, a high level of medication adherence negatively correlated with lifestyle adherence. Multivariate regression analysis showed that blood glucose monitoring adherence is mostly predicted by social–external HLOC, diabetes self-efficacy, and internal HLOC, while dietary adherence is predicted by the patient’s self-efficacy and duration of the illness. Additionally, understanding and following the diabetes treatment were significantly associated with dietary adherence and high levels of patient self-efficacy, while health literacy was mostly predicted by internal HLOC.
Conclusion
Adherence to medication, diet, glucose monitoring, and physical exercise showed different levels in T2DM patients and were in association with psychodemographic factors.
Keywords: type 2 diabetes mellitus, T2DM, medication adherence, lifestyle adherence, self-efficacy, health literacy, health locus of control
Introduction
According to the WHO, type 2 diabetes mellitus (T2DM) is a chronic disease caused by the body’s ineffective use of insulin.1 Treatment of T2DM requires complex lifestyle therapy in addition to medication.2 This means that people with T2DM must control their blood glucose levels and concurrently keep their body weight and blood pressure at an optimum level, requiring dietary therapy as well as regular physical exercise.3 It is important to highlight that uncontrolled blood glucose levels can increase the risk of microvascular and macrovascular complications. Microvascular complications include retinopathy, nephropathy, and neuropathy, while macrovascular complications affect the large blood vessels and include cardiovascular diseases and strokes.1,4 If the patient is required to take medication to lower blood glucose levels, this can only be effective if the patient also undergoes lifestyle therapy. It is important to note that personalized diabetes therapy is based on patients’ health condition.3
The importance of adherence
The therapy administered to people diagnosed with T2DM is usually designed to meet requirements and needs, with adherence (therapy loyalty) being of key importance.5 Adherence behavior among people with diabetes generally lowers blood glucose levels and shows a higher correlation with self-efficacy, health literacy, and health locus of control (HLOC) of patients than with demographic variables.6,7 The underlying reasons for nonadherence among patients with diabetes should be examined in association with psychosocial factors, and it is also worth considering what led to lower adherence and what form it took.8
In the literature on the subject, the most often cited psychosocial factor for patient adherence is diabetes self-efficacy,9,10 which determines coping behavior of individuals, the amount of effort they are capable of expending, and the amount of time they will face obstacles and adverse experiences.11 More precisely, self-efficacy means that people believe in their own abilities and feel that they have control over events around them.11 According to the research conducted by Indelicato et al in 2017, there is a significant correlation between the glycemic level of patients with diabetes and the level of confidence patients have in their own ability to exercise a positive effect on their own health status.9 Apart from this confidence, another often cited psychosocial factor for adherence is patients’ HLOC belief.12 In internal HLOC, individuals attribute their health to their own actions and they believe that health outcomes are under their control. In contrast, external HLOC beliefs include chance expectations or environmental circumstances and control by powerful others such as physician or family members.13 Further research findings indicate that there is a significant, positive correlation between the self-efficacy of individuals and their internal HLOC on the one hand and medication adherence on the other.10 Additionally, there are studies highlighting the importance of health literacy during diabetes adherence: “Health literacy is the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.”14 Recent studies show a correlation between adherence and health literacy8,15–17 and between patients’ HLOC17,18 and their health belief,19 as adherence is determined by the amount of information they understand and internalize about the illness and the treatment.
There are various reasons for nonadherence behavior in patients with diabetes. Patients’ attitude can be affected by an inappropriate level of health literacy, fear of side effects of medication, or even the complexity of managing medication. Patient–physician communication is an important factor in adherence; there is a significant, positive correlation between physician communication and patient adherence.20–22 Of course, patients must possess appropriate cognitive functions, memory, and ability to understand to follow doctor’s instructions, as well as personality and psychological resources that may contribute to coping with diabetes successfully.19 The importance of these variables and their relation to diabetic therapy and adherence are discussed below in great detail following a review of the types of adherence.
Various types of adherence in diabetic therapy
In the present study, we determine medication adherence (adherence-M), glucose monitoring adherence (adherence-GM), dietary adherence (adherence-D), and physical exercise adherence (adherence-PE). It is currently becoming part of efficient and effective treatment to explore and understand the correlations between various types of adherence; it can be considered key to therapy success. Few studies examine the diverse types of adherence among T2DM patients, and most of these studies focus on the adherence-M.2,5,18,23 This is probably due to the fact that this type of adherence is the easiest to examine and quantify, as, in addition to self-reporting, there are various objective measurements at our disposal to follow the drug regimen; furthermore, the majority of doctors place an emphasis on a pharmaceutical solution.4,18,23 However, diabetes requires lifelong professional care, and the key to preparing tertiary prevention regimens is to explore the correlation between additional adherences in depth and to understand them.24
According to Debussche, one of the key factors required for adherence is that patients must be able to make informed decisions on their own, possess good problem-solving skills, be able to manage their disease, and be open to cooperation with health care professionals, as this will enable them to achieve a higher quality of life.25 Adherent attitude toward diet can only be successful if the disease does not directly affect the person’s well-being; that is, the criteria for dietary therapy can be adapted to the lifestyle of the person. Eckert underlined the point that for lifestyle therapies social context and social support play a central role in the strategies the patient develops for coping with the disease, while the success of self-management depends more on the person’s self-efficacy. However, it should be pointed out that self-efficacy develops parallel to successful adaptation and the development of coping strategies; it is not a result of the process. Eckert also stressed that based on studies conducted on adherence-PE, people with T2DM over 63 years of age who exhibit adherence behavior regarding physical exercise incurred lower health care expenditures on antidiabetics and other medication and required medical services less frequently.3 It is important to note that a high level of patient adherence to physical exercise therapy significantly improves blood glucose levels, as the blood supply to muscles improves, thus increasing the body’s glucose utilization.26 Moreover, regular physical exercise helps maintain optimal body weight, boosts life satisfaction, improves lipid profile, and benefits mental health.27 In general, we can say that nonadherence behavior in relation to lifestyle therapy shows a significant inverse correlation with more severe complications in patients and their frequency.24
Adherence to self-monitoring of blood glucose poses a considerable challenge among diabetes patients, firstly, because it imposes restrictions on patient lifestyle, telling them when to eat, and it shows a strong correlation with adherence-D and adherence-PE. Secondly, if it is not appropriately regulated, it can cause frequent low blood glucose levels as well as increase the incidence of complications.28,29 More precisely, since the therapy of patients with T2DM is determined by changes in HbA1c levels, adherence rate for glycemic monitoring is affected significantly by patients’ problem-solving skills as well as by the proper setting of treatment targets.30 In addition to these considerations, adherence to self-monitoring of blood glucose levels is closely associated with lifestyle therapies and can indeed be considered the key lifestyle therapy. This type of adherence is usually associated with a higher level of health literacy, including a sufficient amount of information about the illness. Indeed, how much patients can manage their own diabetes depends first and foremost on their knowledge of the self-monitoring of blood glucose levels.31
Findings from previous studies indicate that it would be important to explore types of adherence one by one as well as to review factors affecting adherence in diabetes patients from perspectives that would shed light on the dynamics and modes of action of correlations. In the following sections, we explore the literature on the relationship of the psychosocial factors to adherence that presumably have a significant effect on the management of diabetes.
The importance of health literacy and its effect on adherence
Fransen et al collected and analyzed empirical studies on health literacy and patient self-management behaviors. They concluded that for diabetic therapy to be successful, it was necessary for patients not only to be motivated, but also to have great self-efficacy as well as high health literacy.32 This is because low health literacy in patients with diabetes may hinder their adherence behavior as they cannot comprehend and organize information effectively, thus potentially causing further difficulties with regard to following doctor’s orders.33 These findings are confirmed by further studies, which have found that patients’ disease knowledge correlates with their perceived self-efficacy.15,34 A low level of health literacy has a negative effect on the health of the patients concerned;16,35 moreover, patients’ disease knowledge has an influence on their therapy adherence rate.31,36,37 Based on a comprehensive meta-analysis and a review, the relationship between health literacy, adherence, and self-efficacy is inconsistent.34,38
The role of the locus-of-control belief in diabetic therapy
With chronic patients, in addition to adherence, the locus-of-control belief can also be crucial for further improvement of health status.39 Internal control has a positive effect on the health behavior of the patient;40 it may influence which health-related behaviors a person will prefer or perform during diabetes therapy.41 However, a lack of internal control may lead to unhealthy dietary choices among people with diabetes.42 These points are also supported by the research conducted by Wallston and Wallston among patients diagnosed with chronic illnesses; they found that with regard to the dimensions of HLOC patients with a high level of both internal and external–social control exhibited a higher level of adherence among the medical staff.57 If we look at it from the diabetes patients’ perspective, it is probable that the high level of internal HLOC in conjunction with other psychosocial resources may improve the adherence behavior of patients toward the therapy.
Self-efficacy and its relationship to lifestyle therapy
As belief in one’s self-efficacy can bring about behavioral changes, it plays an important role among diabetes patients, particularly in managing the therapy.15 Patients with T2DM who have more severe symptoms of depression and anxiety and experience greater stress tend to feel less efficient and committed to diabetic therapy.15,43 It has also previously been observed that lower self-efficacy in diabetes has a negative effect on the control of HbA1c level in patients15,44 and shows a relationship with lower health literacy.43 As noted earlier, therapy for patients with diabetes requires lifestyle changes as well, so how much patients are able to face initial difficulties greatly depends on their level of self-efficacy: patients with low self-efficacy tend to be stopped by the first obstacle and focus on the unfavorable outcome of their illness.45
Objectives
The objective of this study is to explore the adherence behavior of patients with T2DM by examining the associations between the various types of adherence: adherence-M, adherence-GM, adherence-D, and adherence-PE. Moreover, we would also like to test whether health literacy, self-efficacy, and HLOC belief affect therapy adherence. Additionally, we made first steps to explore patient-related barrier factors which hypothetically affect adherence during diabetes therapy.
Patients and methods
Settings and sample
Study participants were patients diagnosed with T2DM receiving treatment at the Diabetes Unit, 1st Department of Internal Medicine, Szent-Györgyi Albert Health Centre, University of Szeged. The patients were in the process of switching from antidiabetics to insulin, or from one type of insulin to another. A diabetologist participated in the development of instruments. Data were collected between February and November 2016 by convenience sampling conducted by an interviewer who asked the participants to evaluate their adherence to diabetic therapy by filling out a questionnaire. The final sample consisted of responses from 113 patients, including 38 men and 75 women. The average age of the participants was 60.56 years (SD=12.9, minimum: 20 years, maximum: 85 years), and the participants were diagnosed with diabetes mellitus for an average of 13 years (SD=8.2). When the data were processed, one patient’s data had to be excluded as the person had been diagnosed with diabetes for 60 years, which was an outlier in our sample.
Study measurements
The psychosocial parameters for adherence were measured using our own questions based on validated questionnaires, which contained certain items on HLOC belief, health belief, and perceived self-efficacy as well as some items on treatment methods and health literacy. In addition, we used an adherence questionnaire conceptualized by the research group to explore the different adherence types and collected participants’ demographic data (Table 1). Our questionnaire measures diverse types of adherence: adherence-M, adherence-GM, adherence-D, and adherence-PE. The section about adherence-M contains statements related to medication prescription and taking medication according to prescription. Adherence-GM, which means a consistent and regular blood glucose level monitoring, was measured with a statement related to prescribed treatment regimens. Lifestyle therapy adherences (adherence-D and adherence-PE) were measured with statements related to medical nutrition therapy and daily physical exercise (Figure S1).
Table 1.
Sociodemographic characteristics of the sample and descriptive statistics for the study variables
| Sociodemographic factors | N=113 |
|---|---|
| Sex | |
| Male, n (%) | 38 (33.6) |
| Female, n (%) | 75 (66.4) |
| Age (years), mean (SD), range | 60.56 (12.9), 20–85 |
| 20–63 years old, n (%) | 62 (54.9) |
| ≥63 years old, n (%) | 51 (45.1) |
| Duration of diabetes (years), mean (SD) | 13 (8.2) |
| Labor market status | |
| Employed, n (%) | 33 (29.2) |
| Retired, n (%) | 80 (70.8) |
| Education level | |
| Low level, n (%) | 60 (53.1) |
| High level, n (%) | 53 (46.9) |
Note: Sociodemographic characteristics of the sample show normal distributions.
The statements regarding adherence inhibitors were formulated specifically for the target group and were consistent with study objectives. The adherence inhibitors included financial difficulties, forgetfulness, lack of time, family problems, disagreement with doctor’s instructions, the ineffectiveness/harmfulness of prescribed medical therapy according to other sources, fear of side effects and long-term effects, lack of clear instructions given by the doctor, lack of clear instructions in the product description of the medication, overly complicated/complex therapy, self-restraint to therapy, and lack of motivation to follow a regimen.
Multidimensional HLOC scale
The scale used for evaluating HLOC in this study was based on the validated questionnaire created by Wallston; however, unlike the original, it contained diabetes-specific statements to assess patients, and also had fewer questions. One statement about internal HLOC belief was “Diabetes basically depends on your own self-strength”, while a statement “In the treatment of diabetes, the social environment (physician, family, friends) is extremely important” was an item present on the strong social–external HLOC subscale. Furthermore, external HLOC belief was measured with statements like “The improvement or decline of health condition related to diabetes is mostly random”. The internal consistency value on the internal HLOC scale proved to be acceptable, while with the social–external and chance external HLOC the small number of items meant that no relevant reliability could be measured.
Health belief scale
According to the literature, one of the most widespread models of health behavior is the health belief model. A primary objective of the model is to predict the factors that determine health behavior, mainly through participation in screening examinations. Health behavior is primarily influenced by perceived danger, which is a combination of the severity of a perceived illness or the consequence of failing to take preventive measures to prevent illness and an estimate of the degree to which a person feels affected by it. Other components of the model are the benefits the behavior can bring as well as the obstacles, costs, and disadvantages of the behavior. In addition to the health-related beliefs factor, the model contains a perceived efficacy variable, as in “You are able to effectively treat your illness and its symptoms, to cope with the illness and to comply with the treatment requirements”. The internal reliability index for the health belief factor on the questionnaire was 0.651, while the internal consistency for self-efficacy amounted to a somewhat lower value due to the small number of items.
Data analysis
Statistical analysis of the data was performed using IBM SPSS for Windows 22 (IBM Corporation, Armonk, NY, USA). The first step was to prepare statistical data, so we detected missing values and screened the outliers. Before selecting the trial, it is important to know whether we can perform a parametric test or not. While processing the data, we checked the distributions of participants’ sociodemographic data and statistics by analyzing their scores (mean ± SD) (Table 1). We checked normality by item, questionnaire, and group to select the relevant statistical hypothesis tests. Since the Kolmogorov–Smirnov hypothesis testing procedure showed that the conditions for normality deviation were not always met, we decided to use nonparametric tests. As we wanted to measure the effect of several independent variables, a multivariate regression analysis was performed. In addition, we decided to use the stepwise method, which is one of the most stringent methods. We paid careful attention to the fact that multivariate regression analysis is extremely sensitive to outliers. In order to get more reliable results, we standardized the variables. With this in mind, we decided to use nonparametric tests. We also agreed that the statistically significant P-value should be <0.05. We examined the associations between variables using Spearman’s rank correlation and used multivariate regression analysis to identify predictive variables for adherent behavior. As mentioned before, the variables were standardized and we used these in all our measurements (Spearman’s rank correlation, multivariate regression analysis). In addition, we attempted to examine factors with a negative effect on adherence using factor analysis.
We performed an exploratory factor analysis for adherence inhibitors to identify items that measure similar phenomena and content. The exploratory factor analysis was performed using the principal component analysis method with oblimin rotation. The applicability of data for factor analysis was tested using Bartlett’s test of sphericity as well as the Kaiser–Meyer–Olkin index. In addition, variables with a factor loading <0.3 were not considered.
Results
The final sample consisted of 113 T2DM inpatients with a mean age of 60.56 years (SD=12.94, range: 20–85 years) and an average diabetes duration of 13 years. On the Diabetes Adherence Questionnaire, 87.6% of the respondents stated that they get all the prescribed medicines, and 80.5% of respondents reported taking medications according to prescriptions. Furthermore, 78.8% of the patients stated being adherent to measuring blood glucose level, while adherence to diet was stated by only 13.3% of respondents. Moreover, only 12.4% of respondents reported adherence to physical exercise. Table 2 shows the different frequencies of responses as not all participants were willing to provide response to each item. In the case of items about psychosocial variables, the majority of responses indicated a high level of adherence (Table 3).
Table 2.
Response rate for the diverse types of adherence
| Type of evaluated adherence | Questions | Percentage of adherent responses |
|---|---|---|
| Medication adherence | Getting all the prescribed medicine | 87.6% |
| Take medication according to the prescription | 80.5% | |
| Glucose monitoring adherence | Measuring blood glucose level | 78.8% |
| Dietary adherence | Medical nutrition therapy | 13.3% |
| Physical exercise adherence | Daily physical exercise | 12.4% |
Notes: The table shows the items of different types of adherence based on the Diabetes Adherence Questionnaire. It is important to note that only values 4 and 5 on the 5-degree Likert-scale were interpreted as adherent responses.
Table 3.
Response rate for perceived self-efficacy, health literacy, and HLOC belief
| Type of evaluated phenomenon | Questions | Percentage of “agree” responses |
|---|---|---|
| Health literacy | You are perfectly informed about your illness and its healing and treatment. | 76.9% |
| You are perfectly able to apply the prescribed treatment for your illness. | 75.2% | |
| Self-efficacy | Following the prescribed treatment regimens for my illness is efficient in treating its symptoms and effectively improve my health status. | 83.2% |
| You are able to effectively treat your illness and its symptoms, to cope with the illness, and to comply with the treatment requirements. | 76.1% | |
| Health locus of control | Diabetes basically depends on your own self-strength. | 84.1% |
| In the treatment of diabetes, the social environment (physician, family, and friends) is extremely important. | 80.5% | |
| The improvement or decline of health condition related to diabetes is mostly random. | 26.6% |
Notes: The table shows the items of self-efficacy, health literacy, and HLOC belief based on the Diabetes Adherence Questionnaire. It is important to note that only values 4 and 5 on the 5-degree Likert-scale were interpreted as adherent responses.
Abbreviation: HLOC, health locus of control.
Examining the association between the various types of adherence
Adherence-M showed a positive, significant correlation with adherence-GM among patients (r=0.322, P<0.001); that is, the patients are more adherent to drug treatment, the more likely they are to follow doctor’s orders on the self-monitoring of glucose levels. However, adherence-M showed a moderate-to-negative correlation with patients’ adherence-D (r=−0.575, P<0.001). This finding suggests that the more patients adhere to taking antidiabetics regularly and properly, the less motivated they feel to adhere to carbohydrate intake and to meet the criteria for a proper diet. Furthermore, we found a moderate, significant, and inverse correlation between adherence-M and adherence-PE (r=−0.496, P<0.001), suggesting that the more patients follow medication orders, the less they will adhere to physical exercise therapy. Adherence-D showed a correlation with adherence-GM (r=0.414, P<0.001) as well as with adherence-PE (r=0.279, P=0.003). Based on these findings, we can say that the evaluated subjects attempted to integrate the diet prescribed for people with diabetes, were more likely to control their blood glucose levels, and found time to follow the prescribed physical exercise regimen (Table 4).
Table 4.
The relationship between various adherence types and Spearman’s rank correlation values
| Group | Adherence-M | Adherence-GM | Adherence-D | Adherence-PE |
|---|---|---|---|---|
| Adherence-M | 0.322* | −0.575** | −0.496** | |
| Adherence-GM | 0.322* | 0.414** | ||
| Adherence-D | −0.575** | 0.414** | 0.279* | |
| Adherence-PE | −0.496** | 0.279* |
Notes:
P<0.05;
P<0.01.
Abbreviations: Adherence-M, medication adherence; Adherence-GM, glucose monitoring adherence; Adherence-D, dietary adherence; Adherence-PE, physical exercise adherence.
Association of lifestyle, glucose monitoring, and medication adherence with psychosocial variables
As emphasized in the “Introduction” section, T2DM requires a complex therapy, in which lifestyle plays a key role, so we thought it is imperative to examine in greater detail the factors that influence adherence-D and adherence-PE. When developing the linear regression model for adherence-D, we found that the model is significant (F (2.81)=8.466, MSE =0.887, P<0.001); its explanatory power for the whole range was 17.3%. The independent variables were the following: duration of diagnosed diabetes, age, education level, self-efficacy, health literacy, internal HLOC belief, social–external HLOC belief, and external HLOC belief. Adherence-D was predicted by patient self-efficacy (β=0.366, t81=3.622, P=0.001) and the duration of diagnosed diabetes (β=0.208, t81=2.062, P=0.042). The data on adherence-PE proved insufficient to set up the linear model due to the disproportionate number of responses given to a particular statement.
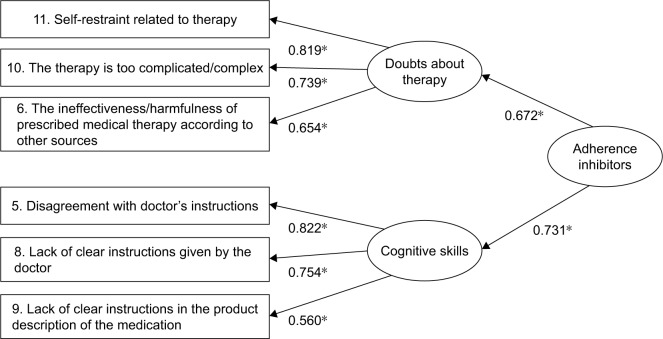
Adherence-GM showed a significant, positive correlation with patients’ internal HLOC belief (r=0.380, P<0.001) as well as the number of antidiabetics taken daily (r=0.211, P=0.049). The linear regression model used proved significant (F (3.78)=10.077, MSE =0.744, P<0.001); its explanatory power for the entire range was 27.9%. The independent variables were the following: duration of diagnosed diabetes, age, education level, self-efficacy, health literacy, internal HLOC belief, social–external HLOC belief, and external HLOC belief. Of the variables measured, social–external HLOC (β=0.312, t78=2.941, P=0.004), perceived self-efficacy (β=0.241, t78=2.484, P=0.015), and internal HLOC were found to be the strongest predictors of adherence-GM (Figure 1).
Figure 1.
Psychosocial variables predicting glucose monitoring adherence indicated with beta values.
Notes: The multivariate regression analysis showed that adherence-GM was mostly predicted by self-efficacy, internal HLOC belief, and social–external HLOC belief. The numbers show beta values or coefficients which show the degree of change in the outcome variable for every one unit of change in the predictor variable. *P<0.05.
Abbreviations: Adherence-GM, glucose monitoring adherence; HLOC, health locus of control.
Results from the factor analysis of adherence inhibitors
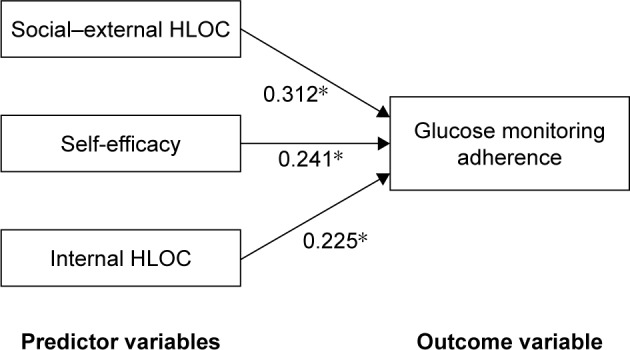
Based on our results, we identified five factors. In accordance with statistical standards, we discuss the “doubts about therapy” and “cognitive skills” factors at length below.
The “doubts about therapy” factor contained items that may have caused adherence inhibition, such as sacrifices, the complexity of therapy, and fear of side effects. The internal consistency of the “doubts about therapy” factor was 0.672, which indicates an acceptable reliability.
The “cognitive skills” factor contained all those variables inhibiting adherence linked to medication instructions provided with the product and agreement with doctor’s orders. The internal consistency of “cognitive skills” turned out to be 0.731, which indicates high reliability (Figure 2).
Figure 2.
The factor structure of adherence inhibitors.
Notes: The path diagram of exploratory factor analysis displays the final model. The numbers show standardized factor loadings, and the items related to the factors “doubts about therapy” and “cognitive skills”. The numbers attached to each item within each rectangular box indicate the item numbers in the adherence inhibitors scale. *P<0.05.
Having obtained all these results, we also checked whether the factors with high internal reliability showed any correlation with the various types of adherence. After performing the statistical analyses, we found that there was a significant negative correlation between the “doubts about therapy” factor and adherence-D (r=−0.368, P=0.001).
Discussion
The objective of our study was to explore the adherence behavior of patients with T2DM, mainly by ascertaining the association between the diverse types of adherence and their determining psychosocial factors. Since previous studies have focused primarily on adherence-M,2,5,21,28 we believe the advantage of our study is that we considered the complexity of variables (the diverse types of adherence and health literacy, self-efficacy, and HLOC belief affecting them) and that we focused mainly on determining the associations between them.
Under examination, we found that there was a moderate, significant, and inverse correlation between adherence-M and lifestyle factors. More specifically, the more patients adhere to taking medication as prescribed, the less likely they were to adhere to dietary therapy and physical exercise. The unexpected finding that higher adherence-M correlates to significantly lower adherence-D and adherence-PE is explained in a number of studies by the fact that in an early phase of the disease patients can avoid hyperglycemia by taking medication that reduces blood glucose.3,16,18 However, this is only a temporary solution, and patients with diabetes must follow a special diet and start doing physical exercise, as the dose–response curve of the medication used cannot offset the blood glucose increase caused by absorption of carbohydrates from food.
In our study, adherence-GM showed a significant, positive correlation with adherence-M and adherence-D. These findings are consistent with observations found in the literature.29,46,47 If adherence-GM is to be considered as one of the main means of diabetic therapy, which can help recognize and prevent hypoglycemia and avert metabolic crises, then it would also be imperative to examine what may cause inappropriate glucose tests in future. The underlying reasons for the study findings can probably be traced back to patients not following dietary instructions closely, as the data collection was supervised by a medical professional. This is confirmed by the fact that since the participating patients were in the process of switching to insulin, it was reasonable to change therapies because the various types of diabetic therapy did not provide them with the metabolic status they wanted to achieve. Overall, if we only attempt to draw conclusions from the perspective of various adherences, we can say that keeping glucose levels within an optimal range takes more than just medication; patients’ carbohydrate intake and dietary habits are also crucial.
Based on our findings, we can say that the degree of adherence-D does not only correlate with adherence-GM, but shows a significant correlation with adherence-PE as well. Thus, if patients can tell the difference between their blood glucose conditions and can regulate their blood glucose levels accordingly, they are more likely to pay attention to what they eat and make sure they lead a healthy lifestyle. We believe the underlying reason for this is that appropriately educated patients are aware of the fact that their body will initiate insulin secretion with some delay after the ingestion of food and that blood glucose levels may shoot up as a result, so adherence to dietary therapy may become crucial. When we look at the association of adherence-D to other types of adherence, we must keep in mind that these processes are also affected by how much patients are able to resolve problematic situations, that is, how resourceful they are, as well as how advanced their diabetes is.
The findings of the study demonstrated the lowest response rate among lifestyle adherences for adherence-PE. A potential reason for this is that it is often unclear even to health care professionals what is meant by physical exercise therapy, as it is not clearly defined.48 Our findings suggest that adherence-PE was in inverse correlation with the degree of adherence-M. In interpreting the findings, it should be noted that we examined results for elderly diabetes patients for the most part. The reason for low adherence-PE may be that long-running medication therapy for the patients in the sample was sufficient to control blood glucose levels, suggesting that they had had decades-long lifestyle habits that could only be changed with sufficient motivation, effort, and determination.7 Having discussed the correlations between the various adherences, let us now focus on an understanding of the effects the presumed psychosocial factors exercise on adherences. In a number of studies, adherence-D shows a positive correlation with patient self-efficacy, internal and external professional HLOC belief, and health literacy.8,15,33,34,39,41,44 Our results are consistent with these findings in confirming that internal HLOC plays an important role in dietary therapy adherence. Where our findings differ from the literature is the effect of external HLOC on the degree of dietary adherence. We attempt to explain the unexpected findings by drawing on an assertion in the literature: in the period of switching from one therapy to another, patients may have felt lower motivation and internal control due to previous failures, an experience which is even greater among the elderly as they may have other comorbidities beyond diabetes that render their everyday life difficult.44,46 Closely related to this is the finding that patients who are exposed to excessive stress and exhaustion generally score lower on health literacy scales.49 However, it seems productive to explore the link between health literacy and beliefs about the harmfulness of treatment.38
In addition to these tests, we also wished to ascertain which psychosocial factors measured would be the best predictors of adherence-D. Our findings showed that there was a 17.3% correlation between adherence-D and the patient’s perceived self-efficacy and the years of diagnosed diabetes. Furthermore, these are the variables that best predict a patient’s adherence. The results can be explained by a fact familiar to us through the literature that self-efficacy is a self-regulation skill which suggests a belief in oneself being able to overcome difficulties and as such can only be achieved through a learning process. This means that patients with diabetes generally do not begin dietary therapy overnight, but face difficulties at the beginning, set their minds to it, and exercise strict self-control.
Adherence-GM shows the most significant, positive correlation with patient health literacy and internal HLOC. Our findings confirmed that adherence-GM among patients with diabetes shows a correlation with internal HLOC as well as the number of antidiabetic pills taken every day. In other words, the better patients are at keeping their HbA1c levels within the normal range, the more likely they are to have HLOC and the more antidiabetics they will take every day.5,8,50 If we explain the findings by saying that the number of pills in this case simply reflects the degree of adherence-M, then it means that HLOC belief is a key to effective medication therapy. However, it is important to note that we also ascribed a key role to health literacy in connection with this type of adherence in our study; however, no significant correlation could be shown between the two variables. Any result that differs from what we expect should be considered carefully, as it may be assumed that the items on health literacy did not test for all the health literacy skills. The latter confirms that the knowledge patients possess about their health is formulated through very complex processes, and this underlines the complexity of the phenomenon.30
In addition to the psychosocial factors affecting adherence-GM, we also set up a linear model to measure which psychological and psychosocial factors most predict a higher degree of patient adherence. Our findings suggest that adherence-GM was 27.9% depending on the personality traits of the patients. More specifically, of the personality factors measured, it was social–external HLOC that predicted adherence-GM, while diabetes self-efficacy was most accurately predicted by internal HLOC. According to Krapek et al,7 adherence increases when blood glucose level is adequately regulated. Furthermore, if we make a comparison based on this finding, we can say that patients with high self-efficacy can affect their health status better, an assertion which is consistent with the theoretical concept that perceived control and a feeling of self-efficacy reduce stress and help cope with the disease.
In addition, the relationship between adherence and self-efficacy plays an important role not only in adherence-M, but also in adherence-GM.9,10,15 Indeed, in order to regulate blood glucose levels, it is necessary for patients to experience a sense of effectiveness and be able to make independent decisions that comply with the doctor’s orders with regard to the self-management of diabetes.
Our statements on health literacy, which consist of information on methods of treatment for the disease, showed a correlation with the types of adherence measured. We found that a significant, positive correlation can be seen between adherence-D and items on knowing appropriate methods of the treatment. Furthermore, we found that the diverse types of adherence can be affected by perceived self-efficacy. We can thus assume that those who can maintain their metabolic state and regulate their blood glucose levels tend to follow recommendations on diet and believe that they can manage their illness. In our research project, we also grouped factors that inhibit adherence, and we concluded that the factors that trigger nonadherence include doubts about therapy and the person’s cognitive skills. Since it is difficult to explore factors inhibiting adherence due to the complexity of the phenomenon and it therefore requires additional investigation, the findings should be handled with caution.
The “doubts about therapy” factor refers to adherence inhibitors from the perspective of socioeconomic factors and factors that depend on therapeutic treatment, such as self-restraint in connection with therapy, complexity of therapy, and fear of side effects. Variables inhibiting adherence that fall within this factor are not often discussed in the literature, since it tends to vary from one person to another among those with diabetes as to what they see as sacrifice and what personal fears they have as regards diabetic therapy. However, the complexity of therapy is considered an inhibiting factor that determines the adherence behavior of patients. This finding is consistent with that of Donnan et al18 and Rubin28 that the complexity of diabetic therapy may decrease patient adherence by as much as 10%–20%. This result is in line with those of our investigation into adherence-M and lifestyle therapy.
The “cognitive skills” factor differs from the factors above in that the patient’s health status and attitudes play a more marked role. Disagreeing with doctor’s orders is often accompanied by lower health literacy, a tendency which is linked to patients not clearly grasping what the doctor has told them or not being able to adequately understand medication instructions provided with the product. Furthermore, it should be noted that doctors and health professionals tend to overrate patients’ cognitive skills, adherence, and knowledge about the therapy,17,51,52 thus rendering it more difficult to recognize adherence inhibitors in a timely manner.
A key point in our exploratory research project was that once we had collected adherence inhibitors and analyzed their nature and characteristics, we also examined which of the diverse types of adherence showed a statistically significant correlation. We found that among the adherence inhibitors, “doubts about therapy” demonstrated a significant, inverse correlation with adherence-D, suggesting that of the types of adherence, following dietary recommendations depended greatly on how complex and complicated the diet seems to the patient and how much the dietary therapy fits into the lifestyle the person has led thus far.
To our knowledge, our investigation of adherence inhibitors is among the few that have used quantitative methods. Most studies examining this topic are qualitative.53–55 The literature to date has attempted to explore phenomena affecting adherence behavior mainly along the lines of the doctor–patient relationship and the characteristics of the health care system, even though factors affecting patient adherence also include information on the patient’s health status, patient-dependent factors, and financial considerations.25 As noted above, this study mainly reviews results from elderly patients with diabetes. With this in mind, it is worth considering that a study conducted in 11 European countries with a sample of people aged above 70 years with diabetes found that good communication with the doctor and health care staff was key to adherence behavior. In such situations, it is not only possible for patients to ask their doctors, questions, but also to obtain answers and solutions for the dilemmas they face, thus possibly allaying the fears they may have about the side effects.56
Limitations and future directions
Since this work was an exploratory research where we used the questionnaire compiled by ourselves, it would be advisable to increase the size of the sample and check the validity of our conclusions on a larger patient population. Another limitation is that the sample consisted of inpatients who were undergoing insulin replacement. Hence, it would be worthy to perform this study on T2DM outpatients who are not involved in a therapeutic regime change. A third limitation is that this research is self-explanatory; thus, social compliance may have an effect on the results obtained.
Overall, the current study can be considered innovative among scientific surveys of adherence, as to the best of our knowledge relatively few studies have dealt with correlations between adherences with such heterogeneous syndromes as T2DM. This claim is confirmed by the fact that to date no internationally validated measurement tool has been designed to explore the various types of adherence. Although we relied on the scientific literature in our study to design the models to be used to examine the phenomena, it would be worthwhile to develop these concepts further and investigate them in greater depth in future. This is linked to our aspiration for this study to serve as a starting point for developing future Hungarian standards, to set down a precise description of the psychosocial factors in adherence behavior and to design complex therapy programs that rely both on adherence-M and on dietary therapy and physical exercise therapy.
Conclusion
Thus, the study recommends to measure and understand diverse types of adherence of T2DM patients. The results of the current study also show that there are associations between diverse types of adherence and patients’ psychosocial attributes.
Ethical approval
Ethical approval for the study was obtained from the Human Investigation Review Board at the University of Szeged, Hungary (registration number 5/2016 – SZTE). All the required ethical statements were collected during the research.
Informed consent
Written informed consent in accordance with the Declaration of Helsinki was provided by all the participants of the study.
Supplementary materials
Diabetes Adherence Questionnaire.
Acknowledgments
This research was supported by EU-funded Hungarian grant EFOP-3.6.1-16-2016-00008.
Footnotes
Author contributions
Andrea Klinovszky performed statistical analysis and interpretation of data, and drafted and wrote the manuscript. István Márton Kiss contributed to study design, data collection, and construction of study measurements. Orsolya Papp-Zipernovszky supervised the work, performed critical revision, and provided scientific advice. Csaba Lengyel served as the diabetologist, contributed to sample composition and discussion, and provided scientific advice. Norbert Buzás planned and supervised the work, participated in construction of study measurements, drafted and wrote the manuscript, and performed critical revision. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.World Health Organization [webpage on the Internet] Global report on diabetes. Geneva: 2016. [Accessed November 18, 2018]. Available from: https://www.who.int/diabetes/global-report/en/ [Google Scholar]
- 2.de Vries ST, Keers JC, Visser R, et al. Medication beliefs, treatment complexity, and non-adherence to different drug classes in patients with type 2 diabetes. J Psychosom Res. 2014;76(2):134–138. doi: 10.1016/j.jpsychores.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 3.Eckert K. Impact of physical activity and bodyweight on health-related quality of life in people with type 2 diabetes. DMSO. 2012;5(1):303–311. doi: 10.2147/DMSO.S34835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Diabetes Association Introduction: Standards of Medical Care in Diabetes – 2018. [Accessed November 29, 2018];Diabetes Care. 2018 41(Suppl 1):S1–S156. doi: 10.2337/dc18-Sint01. Available from: http://care.diabetesjournals.org/content/diacare/suppl/2017/12/08/41.Supplement_1.DC1/DC_41_S1_Combined.pdf. [DOI] [PubMed] [Google Scholar]
- 5.Clifford S, Perez-Nieves M, Skalicky AM, Reaney M, Coyne KS. A systematic literature review of methodologies used to assess medication adherence in patients with diabetes. Curr Med Res Opin. 2014;30(6):1071–1085. doi: 10.1185/03007995.2014.884491. [DOI] [PubMed] [Google Scholar]
- 6.Dimatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychology. 2004;23(2):207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- 7.Krapek K, King K, Warren SS, et al. Medication adherence and associated hemoglobin A1c in type 2 diabetes. Ann Pharmacother. 2004;38(9):1357–1362. doi: 10.1345/aph.1D612. [DOI] [PubMed] [Google Scholar]
- 8.Adam J, Folds L. Depression, self-efficacy, and adherence in patients with type 2 diabetes. The Journal for Nurse Practitioners. 2014;10(9):646–652. [Google Scholar]
- 9.Indelicato L, Dauriz M, Santi L, et al. Psychological distress, self-efficacy and glycemic control in type 2 diabetes. Nutr Metab Cardiovasc Dis. 2017;27(4):300–306. doi: 10.1016/j.numecd.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 10.Náfrádi L, Nakamoto K, Schulz PJ. Is patient empowerment the key to promote adherence? A systematic review of the relationship between self-efficacy, health locus of control and medication adherence. PLoS One. 2017;12(10):e0186458. doi: 10.1371/journal.pone.0186458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 12.Pourhoseinzadeh M, Gheibizadeh M, Moradikalboland M. The relationship between health locus of control and health behaviors in emergency medicine personnel. Int J Community Based Nurs Midwifery. 2017;5(4):397–407. [PMC free article] [PubMed] [Google Scholar]
- 13.Chen S, Lin HS. Relationships among health locus of control, psychosocial status and glycemic control in type 2 diabetes adults. J Nurse Care. 2014;3(3):1–6. [Google Scholar]
- 14.Rudd Re, Anderson W, Oppenheimer S, et al. Health literacy: an update of medical and public health. Annual Review of Adult Learning and Literacy. 2007;7(2):175–197. [Google Scholar]
- 15.Osborn CY, Cavanaugh K, Wallston KA, Rothman RL. Self-efficacy links health literacy and numeracy to glycemic control. J Health Commun. 2010;15(Suppl 2):146–158. doi: 10.1080/10810730.2010.499980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ivanisic M. Testing health literacy in Osijek hospital patients using the validated Croatian version of newest vital sign (NVS) health literacy instrument. PLoS One. 2018;13(2):1–14. doi: 10.1371/journal.pone.0193079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826–834. doi: 10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Donnan PT, Macdonald TM, Morris AD. Adherence to prescribed oral hypoglycaemic medication in a population of patients with type 2 diabetes: a retrospective cohort study. Diabet Med. 2002;19(4):279–284. doi: 10.1046/j.1464-5491.2002.00689.x. [DOI] [PubMed] [Google Scholar]
- 19.Anderson B, Ho J, Brackett J, Finkelstein D, Laffel L. Parental involvement in diabetes management tasks: relationships to blood glucose monitoring adherence and metabolic control in young adolescents with insulin-dependent diabetes mellitus. J Pediatr. 1997;130(2):257–265. doi: 10.1016/s0022-3476(97)70352-4. [DOI] [PubMed] [Google Scholar]
- 20.Krass I, Schieback P, Dhippayom T. Adherence to diabetes medication: a systematic review. Diabet Med. 2015;32(6):725–737. doi: 10.1111/dme.12651. [DOI] [PubMed] [Google Scholar]
- 21.Balkrishnan R. Predictors of medication adherence in the elderly. Clin Ther. 1998;20(4):764–771. doi: 10.1016/s0149-2918(98)80139-2. [DOI] [PubMed] [Google Scholar]
- 22.Guénette L, Lauzier S, Guillaumie L, et al. Patients’ beliefs about adherence to oral antidiabetic treatment: a qualitative study. Patient Prefer Adherence. 2015;9(1):413–420. doi: 10.2147/PPA.S78628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lam WY, Fresco P. Medication adherence measures: an overview. Biomed Res Int. 2015;2015(5 supplement):217047, 1–12. doi: 10.1155/2015/217047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.García-Pérez LE, Álvarez M, Dilla T, Gil-Guillén V, Orozco-Beltrán D. Adherence to therapies in patients with type 2 diabetes. Diabetes Ther. 2013;4(2):175–194. doi: 10.1007/s13300-013-0034-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Debussche X. Is adherence a relevant issue in the self-management education of diabetes? a mixed narrative review. DMSO. 2014;29(7):357–367. doi: 10.2147/DMSO.S36369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnson MD, Anderson JR, Walker A, Wilcox A, Lewis VL, Robbins DC. Common dyadic coping is indirectly related to dietary and exercise adherence via patient and partner diabetes efficacy. J Fam Psychol. 2013;27(5):722–730. doi: 10.1037/a0034006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Madden K. Evidence for the benefit of exercise therapy in patients with type 2 diabetes. DMSO. 2013;6(1):233–239. doi: 10.2147/DMSO.S32951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rubin RR. Adherence to pharmacologic therapy in patients with type 2 diabetes mellitus. Am J Med. 2005;118(5):27–34. doi: 10.1016/j.amjmed.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 29.Sun P, Lian J. Treatment adherence in newly diagnosed type 2 diabetes: patient characteristics and long-term impact of adherence on inpatient care utilization. Postgrad Med. 2016;128(4):338–345. doi: 10.1080/00325481.2016.1151326. [DOI] [PubMed] [Google Scholar]
- 30.Patton SR. Adherence to glycemic monitoring in diabetes. J Diabetes Sci Technol. 2015;9(3):668–675. doi: 10.1177/1932296814567709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gherman A, Schnur J, Montgomery G, et al. How are adherent people more likely to think? A meta-analysis of health beliefs and diabetes self-care. Diabetes Educ. 2011;37(3):392–408. doi: 10.1177/0145721711403012. [DOI] [PubMed] [Google Scholar]
- 32.Fransen MP, von Wagner C, Essink-Bot ML. Diabetes self-management in patients with low health literacy: ordering findings from literature in a health literacy framework. Patient Educ Couns. 2012;88(1):44–53. doi: 10.1016/j.pec.2011.11.015. [DOI] [PubMed] [Google Scholar]
- 33.Powell CK, Hill EG, Clancy DE. The relationship between health literacy and diabetes knowledge and readiness to take health actions. Diabetes Educ. 2007;33(1):144–151. doi: 10.1177/0145721706297452. [DOI] [PubMed] [Google Scholar]
- 34.Baker DW, Parker RM, Williams MV, et al. The health care experience of patients with Low Literacy. Arch Fam Med. 1996;5(6):329–334. doi: 10.1001/archfami.5.6.329. [DOI] [PubMed] [Google Scholar]
- 35.Ubavic S, Krajnovic D, Marinkovic V. Analysis of health literacy instruments which could be used on a primary healthcare level. Arh Farm. 2015;65(1):72–87. [Google Scholar]
- 36.Cavanaugh KL. Health literacy in diabetes care: explanation, evidence and equipment. Diabetes Manag. 2011;1(2):191–199. doi: 10.2217/dmt.11.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Delamater AM. Improving patient adherence. Clinical Diabetes. 2006;24(2):71–77. [Google Scholar]
- 38.Al Sayah F, Majumdar SR, Williams B, Robertson S, Johnson JA. Health literacy and health outcomes in diabetes: a systematic review. J Gen Intern Med. 2013;28(3):444–452. doi: 10.1007/s11606-012-2241-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kneckt MC, Syrjälä AM, Knuuttila ML, Syrjälä AH. Locus of control beliefs predicting oral and diabetes health behavior and health status. Acta Odontol Scand. 1999;57(3):127–131. doi: 10.1080/000163599428841. [DOI] [PubMed] [Google Scholar]
- 40.Rafael B, Konkolÿ Thege B, Kovács P, et al. Szorongás, depresszió, egészségkontrollhit és az egészség-magatartással való kapcsolatuk ischaemiás szívbetegek körében [Anxiety, depression, health-related control beliefs, and their association with health behaviour in patients with ischemic heart disease] Orv Hetil. 2015;156(20):813–822. doi: 10.1556/650.2015.30158. [DOI] [PubMed] [Google Scholar]
- 41.Petricek G, Vuletić Mavrinac G, Vrcić-Keglevic M. Health locus of control assessment in diabetes mellitus type 2 patients. Acta Med Croatica. 2009;63(2):135–143. Croatian. [PubMed] [Google Scholar]
- 42.Wardle J, Steptoe A. Socioeconomic differences in attitudes and beliefs about healthy lifestyles. J Epidemiol Community Health. 2003;57(6):440–443. doi: 10.1136/jech.57.6.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Robertson SM, Amspoker AB, Cully JA, Ross EL, Naik AD. Affective symptoms and change in diabetes self-efficacy and glycaemic control. Diabet Med. 2013;30(5):e189–e196. doi: 10.1111/dme.12146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Knappe S, Pinquart M. Tracing criteria of successful aging? Health locus of control and well-being in older patients with internal diseases. Psychol Health Med. 2009;14(2):201–212. doi: 10.1080/13548500802385717. [DOI] [PubMed] [Google Scholar]
- 45.Katon WJ, Lin EH, von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611–2620. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rothman RL, Malone R, Bryant B, et al. The spoken knowledge in low Literacy in diabetes scale: a diabetes knowledge scale for vulnerable patients. Diabetes Educ. 2005;31(2):215–224. doi: 10.1177/0145721705275002. [DOI] [PubMed] [Google Scholar]
- 47.Strychar I, Elisha B, Schmitz N. Type 2 diabetes self-management: role of diet self-efficacy. Can J Diabetes. 2012;36(6):337–344. [Google Scholar]
- 48.Shea SC. Improving Medication Adherence: How to Talk with Patients About Their Medications. 1st ed. Philadelphia: Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 49.Mertig RG. Nurses’ Guide to Teaching Diabetes Self-Management. 2nd ed. New York: Springer; 2012. [Google Scholar]
- 50.Schinckus L, Dangoisse F, van den Broucke S, Mikolajczak M. When knowing is not enough: Emotional distress and depression reduce the positive effects of health literacy on diabetes self-management. Patient Educ Couns. 2018;101(2):324–330. doi: 10.1016/j.pec.2017.08.006. [DOI] [PubMed] [Google Scholar]
- 51.Quill TE, Brody H. Physician recommendations and patient autonomy: finding a balance between physician power and patient choice. Ann Intern Med. 1996;125(9):763–769. doi: 10.7326/0003-4819-125-9-199611010-00010. [DOI] [PubMed] [Google Scholar]
- 52.Mccabe R, Healey PGT. Miscommunication in doctor-patient communication. Top Cogn Sci. 2018;10(2):409–424. doi: 10.1111/tops.12337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Simmons D, Weblemoe T, Voyle J, et al. Personal barriers to diabetes care: lessons from a multi-ethnic community in New Zealand. Diabet Med. 1998;15(11):958–964. doi: 10.1002/(SICI)1096-9136(1998110)15:11<958::AID-DIA687>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 54.Alberti H, Boudriga N, Nabli M. Primary care management of diabetes in a low/middle income country: a multi-method, qualitative study of barriers and facilitators to care. BMC Fam Pract. 2007;8(1):1–7. doi: 10.1186/1471-2296-8-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rushforth B, Mccrorie C, Glidewell L, Midgley E, Foy R. Barriers to effective management of type 2 diabetes in primary care: qualitative systematic review. Br J Gen Pract. 2016;66(643):e114–e127. doi: 10.3399/bjgp16X683509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bastiaens H, van Royen P, Pavlic DR, Raposo V, Baker R. Older people’s preferences for involvement in their own care: a qualitative study in primary health care in 11 European countries. Patient Educ Couns. 2007;68(1):33–42. doi: 10.1016/j.pec.2007.03.025. [DOI] [PubMed] [Google Scholar]
- 57.Wallston KA, Wallston BS. Who is responsible for your health? The construct of Health Locus of Control. In: Sanders GS, Suls J, editors. Social Psychology of Health and Illness. New Jersey: Lawrence Erlbaum Associates; 1982. pp. 65–95. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Diabetes Adherence Questionnaire.