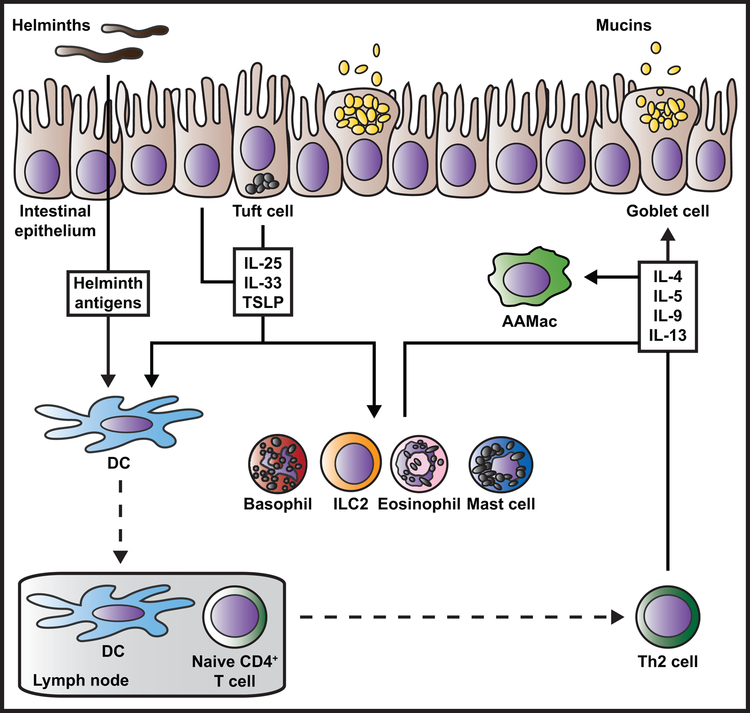
Figure 1. Current paradigm for the regulation of type 2 inflammation during helminth infection.
Damaged, stimulated, or dying intestinal epithelial cells produce cytokines and alarmins such as IL-25, IL-33, and TSLP in response to helminth parasite infection. Tuft cells are a rich source of IL-25. Epithelial cell-derived cytokines act on a variety of innate immune cells including basophils, ILC2s, eosinophils, and mast cells, delivering potent activation, proliferation, recruitment, and/or survival signals. Epithelial cell-derived cytokines also act on DCs that take up and process helminth antigens, grooming these cells to travel to the draining lymph nodes where they present antigen to naïve CD4+ T cells and promote Th2 polarization. In the tissue site, activated innate immune cells and recruited Th2 cells produce large amounts of the type 2 cytokines IL-4, −5, −9, and −13. Different cell types differentially produce these cytokines (not depicted here). Type 2 cytokines amplify innate and adaptive immune cell activation and contribute to wound repair (not depicted here), with IL-4 serving as a key activator of AAMac polarization. IL-4 and IL-13 act back on the damaged epithelium and non-hematopoietic cells to cause goblet cell hyperplasia, tuft cell mobilization, increased intestinal permeability and contractility, and increased epithelial cell turnover that promote worm expulsion.