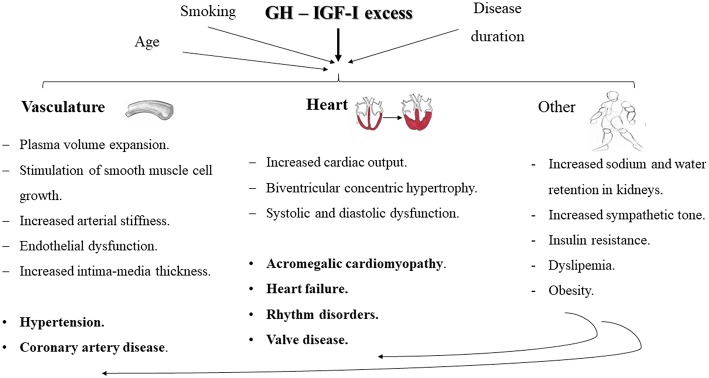
Figure 1.
Schematic representation of the main cardiovascular comorbidities encountered in patients with acromegaly and the key mechanisms involved in their development. Chronic GH hypersecretion and/or IGF-I excess, exacerbated by the influence of other concomitant issues, such as disease duration, age and smoking, may lead to plasma volume expansion, stimulation of smooth muscle cell growth, increased arterial stiffness and endothelial dysfunction and increased intima-media thickness, which may all contribute to the development of hypertension and coronary artery disease. Besides, an increased vascular responsiveness to angiotensin II, sodium and water retention, and an increase in cardiac output, may also contribute to an increased peripheral resistance and exacerbate the development of hypertension. Increased cardiac output, biventricular concentric hypertrophy and systolic and diastolic dysfunction configure the key milestones in the development of acromegalic cardiomyopathy, eventually leading to heart failure. Other typical cardiac alterations in acromegalic patients include rhythm disorders and valve disease. Furthermore, there have been studies suggesting a role of the sympathetic tone in the development of comorbidities in acromegaly. Insulin resistance, obesity and an atherogenic lipid profile may aggravate the progression of cardiovascular alterations.