Abstract
The present study examined the potential function and underlying mechanisms of microRNA-125a (miR-125a) in thyroiditis. Mice were subcutaneously administered with 100 µg porcine thyroglobulin weekly for 2 weeks to establish the thyroiditis model. Results of the in vivo study demonstrated that miR-125a serum expression was upregulated in thyroiditis mice compared with the control group. In vitro studies were performed on a mouse macrophage cell line in which a model of thyroiditis was established using 10 ng/ml human interferon-γ. Upregulated miR-125a expression was achieved via mimic transfection. Increased miR-125a expression reduced autophagy and cell proliferation, increased the apoptotic rate and the expression of pro-inflammatory factors tumor necrosis factor-α, interleukin (IL)-1β, IL-6 and IL-18 via downregulation of the phosphoinositide 3-kinase/protein kinase B/mammalian target of rapamycin (PI3K/Akt/mTOR) signaling pathway. PI3K inhibition enhanced the ability of miR-125a to increase the inflammatory response in vitro via regulation of the PI3K/Akt/mTOR signaling pathway. These results suggest miR-125a inhibited autophagy in a model of thyroiditis through the PI3K/Akt/mTOR signaling pathway.
Keywords: microRNA-125a, thyroiditis, inflammation, phosphoinositide 3-kinase/protein kinase B/mechanical target of rampamycin
Introduction
Autoimmune thyroid disease is a common chronic lymphocytic inflammatory disease, which does not exhibit any of the typical symptoms of systemic infection (1), in which thyroid function is progressively reduced, which severely affects the quality of life of patients (2). Hashimoto's thyroiditis (HT) is a common tissue-specific autoimmune thyroid disease. This can be induced by the termination of immune tolerance due to abnormal immune system regulation, as well as an inappropriate autoimmune response against the thyroid (3).
Autophagy is a highly conserved physiological process that involves lysosome-mediated self-digestion and the recycling of intracellular components, including the cell membrane and organelles, particularly mitochondria, cytoskeletal components and protein complexes (4). Autophagy can remove injured or aging biological macromolecules and organelles in cytoplasm, thus maintaining protein turnover and intracellular homeostasis, as well as regulating cell survival, differentiation and development (5). Autophagy is a regulatory stress response that participates in multiple physiological and pathological cell processes, including embryonic development, aging and cancer (5). It is maintained at a basic level in resting cells for the elimination of defective organelles and misfolded proteins, the prevention of excessive protein accumulation and to cope with endoplasmic reticulum stress (6). Additionally, autophagy is an important inflammatory regulator that is associated with inflammasome and cytokine elimination (6). Autophagy maintains cell homeostasis, protecting cells from injury and death (4). Therefore, autophagy is a necessary physiological process for normal cell function and survival.
A study has demonstrated that the phosphoinositide 3-kinase/protein kinase B/mechanistic target of rapamycin (PI3K/Akt/mTOR) signalling pathway can regulate autophagy as well as apoptosis (7). PI3K/Akt controls cell function by regulating the expression of numerous downstream molecules, including Mtor (7). mTOR is a serine/threonine kinase in the phosphatidyl inositol 3′kinase-related kinase family that is associated with the proliferation and growth of non-neuronal cells (8). Neurons are non-proliferative cells, but previous research has indicated that neuron size is associated with mTOR regulation (9). It has also been demonstrated that mTOR activation is required for neuron extension direction, dendritic development and spine shape (8). PI3K/Akt signalling pathway activation regulates mTOR protein expression to result in the inhibition of neuronal apoptosis (9). Phosphorylated Akt can activate mTOR and mTOR inhibits downstream molecule ULK1 complex to negatively regulate autophagy (10).
miRNAs have the potential to regulate the expression of the majority of human genes (11). miRNAs participate in biological processes of autoimmune disease by regulating the development, differentiation, maturation and signal transduction of immune cells (11). Furthermore, they have an important role in maintaining immune cell homeostasis and normal cell function regulation and therefore have the potential to be used in novel disease therapies (12). It has been identified that >100 miRNAs may contribute to autoimmune disease. These miRNAs have the potential to influence the development and function of innate and acquired immune cells (12). Li and Ding (13) recently demonstrated that miR-125a also promoted serum pro-inflammatory cytokine expression in patients with lupus nephritis. In the present study, the function and underlying mechanisms of miR-125a in thyroiditis were examined.
Materials and methods
Mice and cell culture
Female 6-week-old C57BL/6 mice (n=12; 18–20 g) were purchased from Chongqing Medical University (Chongqing, China), housed in a clean-grade animal breeding centre at 20–24°C, humidity of 55–60% and were given free access to food and water in a 12 h alternating dark/light cycle. Mice were divided into the control (n=6) and thyroiditis model (n=6) groups. In the thyroiditis model group, mice were subcutaneously injected with 100 µg/ml porcine thyroglobulin (Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) weekly for 2 weeks. The peripheral blood of mice (100 µl) was subsequently collected into centrifuge tubes containing heparin (Sigma-Aldrich; Merck KGaA) under anaesthesia, and then the mice were sacrificed by decapitation. In control group, mice were subcutaneously injected with normal saline once a week. The use of animals in the present study was reviewed and approved by the Ethics Committee of The Zhongshan District of Chongqing General Hospital (Chongqing, China).
The mouse macrophage cell line RAW264.7 cell was obtained from The Type Culture Collection of the Chinese Academy of Sciences (Shanghai, China) and cultured in Dulbecco's modified Eagle's medium (DMEM; Thermo Fisher Scientific, Inc., Waltham, MA, USA) supplemented with 10% fetal bovine serum (FBS; Thermo Fisher Scientific, Inc.), 100 U/ml penicillin and 100 U/ml streptomycin at 37°C and 5% CO2.
Hematoxylin and eosin (H&E) staining
Following the induction of thyroiditis, thyroid tissue was fixed with 4% paraformaldehyde for 24 h at room temperature. Thyroid tissue was sectioned into 10-µm-thick sections and H&E staining was performed at room temperature for 10 min. Thyroid tissue was examined using a confocal microscope (Nikon Eclipse Ti; Nikon Corporation, Tokyo, Japan) at a magnification of ×100 to confirm the establishment of the model.
Reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
Total RNA was extracted from the mouse peripheral blood using TRIzol reagent (Life Technologies; Thermo Fisher Scientific, Inc.). cDNA was reverse transcribed using the miScript II RT kit (Qiagen China Co., Ltd., Shanghai, China). RT-qPCR was performed in triplicate using the miScript SYBR Green PCR kit (Qiagen China Co., Ltd.) with the StepOnePlus PCR system (Applied Biosystems; Thermo Fisher Scientific, Inc.). Initial denaturation was performed at 95°C for 30 sec, followed by 40 cycles at 95°C for 30 sec, 60°C for 30 sec and 72°C for 30 sec. The primer sequences used were as follows: miRNA-125a: Forward, 5′-CTGAACTAGTGTGTGCGGAAACACTCAGGG-3′ and reverse, 5′-CTGAAAGCTTGGAGTGACAGATCTGTGTCCTC-3′; U6: Forward, 5′-CCGCCCGCCGCCAGGCCCC-3′ and reverse, 5′-ATATGGAACGCTTCACGAATT-3′. The expression of miRNA-125a was quantified using the 2−ΔΔCq method (14,15).
Cell transfection and establishment of an in vitro model of thyroiditis
Cells (5×105) were seeded into 6-well plates, and transfected with 100 ng miR-125a (5′-ACAGGUGAGGUUCUUGGGAGCC-3′) or a combination of miR-125a and a PI3K inhibitor (20 nM LY294002) for 36 h at 37°C using Lipofectamine® 2000 (both Invitrogen; Thermo Fisher Scientific, Inc.) according to the manufacturer's protocol. In control group, cells (5×105) were transfected with 100 ng negative control miRNA (5′-CCCCCCCCCCCCCCCCCCCCC-3′) using Lipofectamine® 2000 according to the manufacturer's protocol. Cells were subsequently seeded into 6 (1×106 cell/well) or 96 (1×103 cell/well) well plates in DMEM and stimulated with human interferon-γ (IFN-γ; 10 ng/ml; Sigma-Aldrich; Merck KGaA) for 12 h at 37°C. RAW264.7 cells were stimulated with IFN-γ to establish the in vitro model of experimental autoimmune inflammation (16).
MTT assay
Cells (1×103/well) were plated in 96-well plates and MTT (5 mg/ml; 20 µl; Thermo Fisher Scientific, Inc.) was added into each well for 4 h at 37°C. Dimethyl sulfoxide (150 µl; Thermo Fisher Scientific, Inc.) was subsequently added into the wells for 20 min at 37°C. Optical density values were measured with an automatic microplate reader (BioTek Instruments, Inc., Winooski, VT, USA) at 492 nm.
Flow cytometry
After 4 h of transfection, cells were plated in 6-well plates (1×106/well) in DMEM with 10% FBS for 48 h at 37°C and subsequently washed with PBS. Cells were resuspended in binding buffer (Nanjing KeyGen Biotech Co., Ltd., Nanjing, China) and stained with annexin-V fluorescein isothiocyanate (5 µl) and propidium iodide (5 µl; KeyGen Biotech Co., Ltd.) for 15 min in the dark at room temperature. Samples were analysed using a Beckman Coulter flow cytometer (Beckman Coulter, Inc., Fullerton, CA, USA) and FlowJo software (version 7.6.1; FlowJo LLC, Ashland, OR, USA).
Immunocytochemical analysis of autophagy
Cells were washed with PBS, fixed with 4% paraformaldehyde for 15 min at room temperature and permeabilized with 0.1% Triton X-100 for 15 min at room temperature. Cells were subsequently incubated with anti-microtubule-associated protein 1α/1β-light chain 3 (LC3) antibody (cat. no. 3868; 1:1,000; CST Biological Reagents Co., Ltd., Shanghai, China) for 1 h at room temperature, followed by incubation with Alexa Fluor® 488-conjugated goat anti-rabbit antibody (cat. no. 4412; 1:2,000, CST Biological Reagents Co., Ltd.) for 1 h at room temperature. Fluorescence was visualized with a confocal laser-scanning microscope (Zeiss GmbH, Jena, Germany) at a magnification of ×20.
Cytokine assay
Tumor necrosis factor-α (TNF-α; cat. no. EM008-96), interleukin (IL)-1β (cat. no. EM001-96), IL-6 (cat. no. EM004-96) and IL-18 (cat. no. EH047-96) levels were measured in cell supernatant using sandwich ELISA kits (ExCell; Genetimes Technology, Inc., Shanghai, China) according to the manufacturer's protocol.
Western blot analysis
Cells were washed with PBS, harvested and lysed with radioimmunoprecipitation assay buffer (Beyotime Institute of Biotechnology, Haimen, China). Protein content was measured with a bicinchoninic assay following centrifugation at 1,000 × g for 10 min at 4°C. Protein (50 µg) was loaded into each lane, separated using 10% SDS-PAGE and transferred onto polyvinylidene fluoride membranes. The membranes were blocked with 5% skim milk powder for 2 h at 37°C and subsequently incubated overnight at 4°C with primary antibodies against LC3 (cat. no. 4108; 1:1,000), autophagy protein 5 (Atg 5; cat. no. 12994; 1:2,000), PI3K (cat. no. 4249; 1:2,000), phosphorylated (p)-Akt (cat. no. 4060; 1:1,000), p-mTOR (cat. no. 5536; 1:1,000) and GAPDH (cat. no. 5174; 1:5,000; all CST Biological Reagents Co., Ltd.). The membrane was washed in tris-buffered saline with Tween-20 and incubated with horseradish peroxidase-conjugated goat anti-rabbit antibody (cat. no. 7074; 1:5,000; CST Biological Reagents Co., Ltd.). Bands were visualized using an enhanced chemiluminescence plus blotting reagent and Quantity One 1-D 3.0 software (Bio-Rad Laboratories, Inc., Hercules, CA, USA).
Statistical analysis
All data are expressed as the mean ± standard deviation of independent experiments (n=3). Statistical analysis was performed using one-way analysis of variance followed by Tukey's post-hoc test using SPSS software (version 17.0; SPSS, Inc., Chicago, IL, USA). P<0.05 was considered to indicate a statistically significant difference.
Results
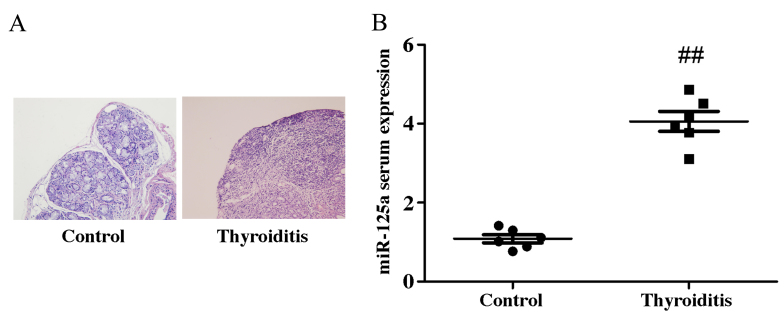
miR-125a serum expression increases in a mouse model of thyroiditis
RT-qPCR was performed to detect miR-125a serum expression. miR-125a expression was significantly upregulated in thyroiditis mice, compared with the control group (Fig. 1). This suggests that miR-125a may be associated with the pathophysiology of thyroiditis.
Figure 1.
miR-125a serum expression in a mouse model of thyroiditis. (A) Hematoxylin and eosin staining and (B) miR-125a serum expression in a mouse model of thyroiditis. Data are expressed as the mean ± standard deviation of independent experiments (n=3). ##P<0.01 vs. control group. miR-125a, microRNA-125a.
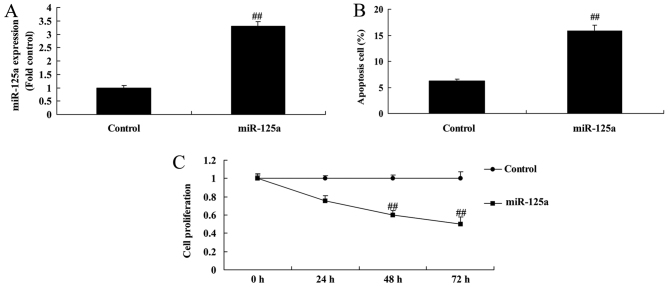
miR-125a upregulation induces apoptosis and reduces cell proliferation in vitro
The effect of miR-125a on cell growth in an in vitro thyroiditis model was examined. miR-125a was significantly upregulated in miRNA-125a mimic transfected cells (Fig. 2A). The upregulation of miRNA-125a significantly increased the apoptotic rate (Fig. 2B) and reduced cell proliferation (Fig. 2C) compared with the control group.
Figure 2.
miR-125a upregulation in an in vitro model of thyroiditis. (A) miR-125 mimic transfection successfully increased miR-125a expression. (B) Percentage of apoptotic cells and (C) rate of cell proliferation in control or miR-125a mimic transfected cells. Data are expressed as the mean ± standard deviation of independent experiments (n=3). ##P<0.01 vs. control group. miR-125a, microRNA-125a.
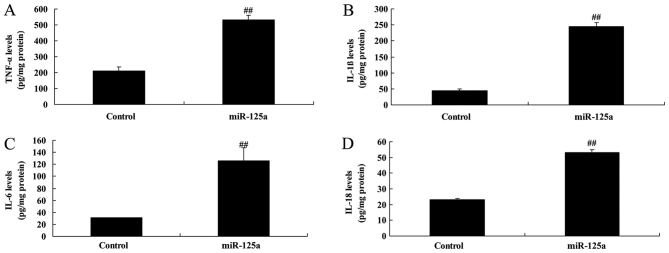
miR-125a upregulation induces the expression of pro-inflammatory factors in vitro
Levels of TNF-α, IL-1β, IL-6 and IL-18 were significantly increased in the in vitro model of thyroiditis when transfected with miR-125a mimics, compared with the control group (Fig. 3), indicating that miR-125a may regulate pro-inflammatory factor expression in thyroiditis.
Figure 3.
miRNA-125a upregulation induced the expression of pro-inflammatory factors (A) TNF-α, (B) IL-1β, (C) IL-6 and (D) IL-18 in an in vitro model of thyroiditis. Data are expressed as the mean ± standard deviation of independent experiments (n=3). ##P<0.01 vs. control group. miR-125a, microRNA-125a; TNF-α, tumor necrosis factor-α; IL, interleukin.
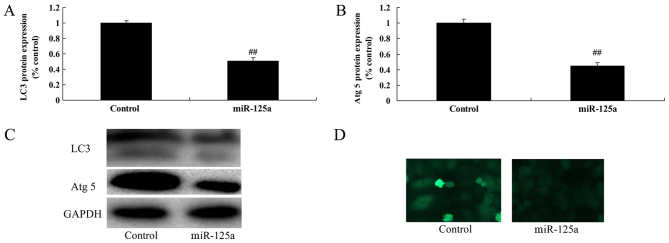
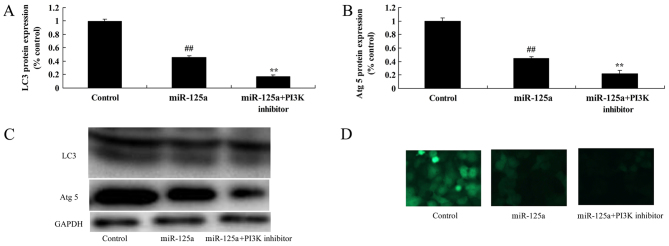
miR-125a upregulation reduces autophagy in vitro
The effect of miR-125a on the expression of autophagy-associated proteins was investigated. The expression of autophagy proteins LC3 and Atg 5 was significantly decreased in the miR-125a mimic transfected group compared with the control (Fig. 4), suggesting that miR-125 may reduce autophagy in thyroiditis.
Figure 4.
miRNA-125a upregulation reduced the relative expression of autophagy proteins (A) LC3 and (B) Atg 5 in an in vitro model of thyroiditis. (C) Western blot analysis of LC3 and Atg 5 expression. (D) LC3 protein expression was visualized by immunocytochemistry with a confocal laser-scanning microscope (magnification, ×40). Data are expressed as the mean ± standard deviation of independent experiments (n=3). ##P<0.01 vs. control group. miR-125a, microRNA-125a; LC3, microtubule-associated protein 1α/1β-light chain 3; Atg 5, autophagy protein 5.
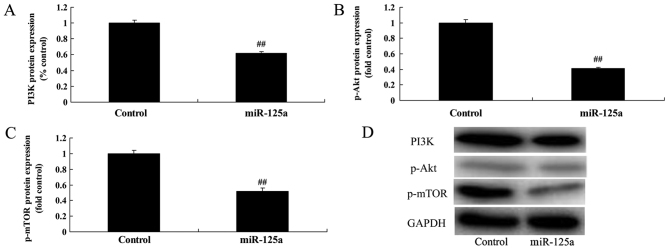
miR-125a suppresses PI3K/Akt/mTOR signalling pathway activation in vitro
miR-125a upregulation significantly suppressed PI3K, p-Akt and p-mTOR levels, compared with the control group (Fig. 5), suggesting that miR-125a suppressed autophagy through inhibition of the PI3K/Akt/mTOR signalling pathway.
Figure 5.
miR-125a upregulation suppressed PI3K/Akt/mTOR signalling pathway activation in an in vitro model of thyroiditis. (A) The relative quantification of (A) PI3K (B) p-Akt and (C) p-mTOR protein expressions was calculated from western blot analysis results. (D) Western blot analysis of PI3K, p-Akt and p-mTOR expression. Data are expressed as the mean ± standard deviation of independent experiments (n=3). ##P<0.01 vs. control group. miR-125a, microRNA-125a; PI3K, phosphoinositide 3-kinase; Akt, protein kinase B; mTOR, mechanistic target of rapamycin; p, phosphorylated.
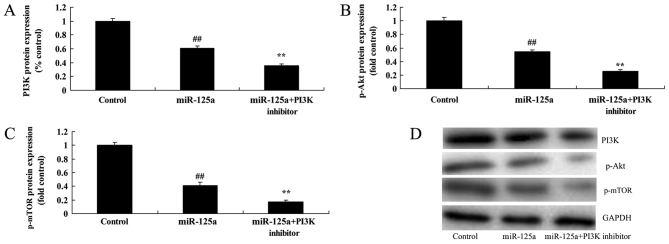
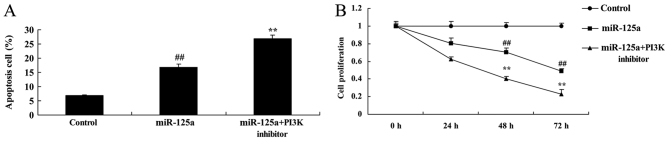
PI3K inhibition enhances the miRNA-125a-mediated suppression of the PI3K/Akt/mTOR signalling pathway, induction of apoptosis and inhibition of cell proliferation in vitro
To examine the role of PI3K in the function of miRNA-125a in thyroiditis, a PI3K inhibitor, 20 nM of LY294002 was used to inhibit the PI3K/Akt/mTOR signalling pathway in the in vitro thyroiditis model. PI3K inhibitor and miRNA-125a mimics significantly reduced PI3K, p-Akt and p-mTOR levels by miRNA-125a, compared with the miRNA-125a mimic alone (Fig. 6). Apoptotic rate was also significantly increased and cell proliferation was further decreased by the PI3K inhibitor and miRNA-125a mimic, compared with the miRNA-125a mimic alone (Fig. 7).
Figure 6.
PI3K inhibition enhanced the ability of miR-125a to suppress PI3K/Akt/mTOR signalling pathway activity in an in vitro model of thyroiditis. Relative quantification of (A) PI3K, (B) p-Akt and (C) p-mTOR levels was calculated from western blot analysis results. (D) Western blot analysis of PI3K, p-Akt and p-mTOR levels. Data are expressed as the mean ± standard deviation of independent experiments (n=3). **P<0.01 vs. miR-125a; ##P<0.01 vs. control group. miR-125a, microRNA-125α; PI3K, phosphoinositide 3-kinase; Akt, protein kinase B; mTOR, mechanistic target of rapamycin; p-, phosphorylated.
Figure 7.
PI3K inhibition enhanced the ability of miR-125a to (A) induce apoptosis and (B) inhibit cell proliferation in an in vitro model of thyroiditis. Data are expressed as the mean ± standard deviation of independent experiments (n=3). **P<0.01 vs. miR-125a; ##P<0.01 vs. control group. miR-125a, microRNA-125a; PI3K, phosphoinositide 3-kinase.
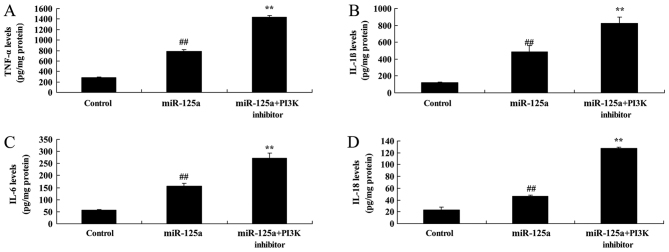
PI3K inhibition enhances the miRNA-125a-mediated increase in pro-inflammatory mediators and decrease in autophagy in vitro
The inhibition of PI3K in combination with the miRNA-125a mimics significantly increased TNF-α, IL-1β, IL-6 and IL-18 expression compared with miRNA-125a mimic alone (Fig. 8). PI3K inhibition also resulted in a further decrease in LC3 and Atg 5 protein expression thyroiditis, compared with miRNA-125a mimic alone (Fig. 9).
Figure 8.
PI3K inhibition enhanced the ability of miR-125a to increase the expression of pro-inflammatory mediators (A) TNF-α, (B) IL-1β, (C) IL-6 and (D) IL-18 in an in vitro model of thyroiditis. Data are expressed as the mean ± standard deviation of independent experiments (n=3). **P<0.01 vs. miR-125a; ##P<0.01 vs. control group. PI3K, phosphoinositide 3-kinase; miR-125a, microRNA-125a; TNF-α, tumor necrosis factor-α; IL, interleukin.
Figure 9.
PI3K inhibition enhanced the ability of miR-125a to inhibit autophagy in an in vitro model of thyroiditis. The relative quantification of (A) LC3 and (B) Atg 5 protein expression was calculated from western blot analysis results. (C) Western blot analysis of LC3 and Atg 5 expression. (D) LC3 protein expression was visualized by immunocytochemistry with a confocal laser-scanning microscope (magnification, ×40). Data are expressed as the mean ± standard deviation of independent experiments (n=3). **P<0.01 vs. miR-125a; ##P<0.01 vs. control group. miR-125a, microRNA-125a; PI3K, phosphoinositide 3-kinase; LC3, microtubule-associated protein 1α/1β-light chain 3; Atg 5, autophagy protein 5.
Discussion
HT, also referred to as chronic lymphocytic thyroiditis, is a T-cell-mediated organ specific autoimmune disease (17). It is the most common type of thyroiditis and typically develops in middle-aged women, with the population morbidity at 2% (18). The present study revealed that miR-125a serum expression was upregulated in a mouse model of thyroiditis compared with the control group. However, only 12 mice were used in the current study and larger cohorts should be used in future research to validate this result. In the current study, RAW264.7 cells stimulated with IFN-γ were used to establish the in vitro model of experimental autoimmune inflammation, however they were not uses as a model of experimental autoimmune thyroiditis as that hypothesis was not adequately supported by previous studies. Other experiment models will be used in a further study.
It has previously been indicated that lymphocytic inflammatory disorder is a major source of ROS (17). Excessive ROS production is associated with allergic dermatitis, continuous inflammation, lupus erythematosus and multiple dermatitis (19). Autophagy defects have been identified in many diseases and are associated with an increased susceptibility to autoimmune and inflammatory disease development (20). HT is an autoimmune inflammatory disease and autophagy has an important role in its pathogenesis (20). The present study demonstrated that miR-125a upregulation reduced the expression of autophagy proteins LC3 and Atg in vitro.
Kim et al (21) recently reported that miR-125a inhibits autophagy activation during mycobacterial infection. The development of HT is closely associated with a signalling network of cytokines, neurotransmitters and other endocrine hormones in the thyroid (22). This signalling network can regulate the differentiation and growth function of thyroid cells in an autocrine and paracrine manner. Inflammatory cytokines associated with this disease include monocyte chemoattractant protein 1 and TNF-α (23). The present study identified that the upregulation of miR-125a induced the expression of inflammatory factors IL-18, IL-6, IL-1β and TNF-α in vitro. Li et al (13) recently demonstrated that miR-125a also promotes serum pro-inflammatory cytokine expression in patients with lupus nephritis.
Akt is a serine/threonine kinase that regulates cell function by phosphorylating various enzymes, kinases and transcription factors following its activation (24). For example, activated Akt can phosphorylate B cell lymphoma-1 and caspases to inhibit apoptosis and act on the class O forkhead box transcription factors member and nuclear factor-κB to regulate cell survival (25). The PI3K/Akt signalling pathway is a molecular pathway that is required for cell survival and has important roles in apoptosis and tumor genesis (25). Its regulatory effect on downstream autophagy-related molecules, including mTOR, has been extensively recognized (9). The results of the present study revealed that miR-125a upregulation suppressed PI3K/Akt/mTOR signalling pathway activation in vitro.
It is well established that necrosis can induce the inflammatory response, the release of toxic cytokines and peripheral cell injury (7). By contrast, apoptosis is a process of programmed cell death that does not induce an inflammatory response and is therefore neuroprotective (10). Research has confirmed that autophagy is regulated by the PI3K/Akt signalling pathway following neuronal mechanical injury. The PI3K/Akt/mTOR pathway has a critical role in the growth, proliferation and survival of cells (10). However, some research has demonstrated that this pathway can induce cell death, particularly necrosis. PI3K/Akt/mTOR pathway activation can inhibit autophagy, which may lead to an increase in necrotic cells and a decrease in neuronal apoptosis and overall cellular activity (9). The present study indicated that the inhibition of PI3K enhanced the ability of miRNA-125a to increase the inflammatory response in macrophages via the PI3K/Akt/mTOR signalling pathway. Tang et al (26) identified that miR-125a also inhibits the invasive ability of hepatocellular carcinoma cells via regulation of the PI3K/Akt/mTOR signalling pathway.
In conclusion, miR-125a increased inflammation and inhibited autophagy in an in vitro model of thyroiditis through regulation of the PI3K/Akt/mTOR signalling pathway. Further investigation is required to fully elucidate the mechanisms involved in autoimmune thyroiditis. The present study provides evidence for a potential mechanism involved in autoimmune thyroiditis pathophysiology.
Acknowledgements
This study was supported by Medical Science and Technology Innovation Project of Chongqing General Hospital (grant no. 2017MSXM02).
Funding
No funding was received.
Availability of data and materials
The analyzed data sets generated during the study are available from the corresponding author on reasonable request.
Authors' contributions
DC, XH, SL, HD, HG, RH and BZ performed the experiments and wrote the manuscript. DC designed the experiment and performed the data analysis.
Ethics approval and consent to participate
The use of animals in the present study was reviewed and approved by the Ethics Committee of The Zhongshan District of Chongqing General Hospital (Chongqing, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Byun JI, Lee ST, Jung KH, Sunwoo JS, Moon J, Lim JA, Lee DY, Shin YW, Kim TJ, Lee KJ, et al. Effect of immunotherapy on seizure outcome in patients with autoimmune encephalitis: A prospective observational registry study. PLoS One. 2016;11:e0146455. doi: 10.1371/journal.pone.0146455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Winther KH, Watt T, Bjørner JB, Cramon P, Feldt-Rasmussen U, Gluud C, Gram J, Groenvold M, Hegedüs L, Knudsen N, et al. The chronic autoimmune thyroiditis quality of life selenium trial (CATALYST): Study protocol for a randomized controlled trial. Trials. 2014;15:115. doi: 10.1186/1745-6215-15-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nazarpour S, Ramezani Tehrani F, Simbar M, Tohidi M, Alavi Majd H, Azizi F. Effects of levothyroxine treatment on pregnancy outcomes in pregnant women with autoimmune thyroid disease. Eur J Endocrinol. 2017;176:253–265. doi: 10.1530/EJE-16-0548. [DOI] [PubMed] [Google Scholar]
- 4.Kim HM, Kim ES, Koo JS. Expression of autophagy-related proteins in different types of thyroid cancer. Int J Mol Sci. 2017;18:E540. doi: 10.3390/ijms18030540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh BK, Sinha RA, Ohba K, Yen PM. Role of thyroid hormone in hepatic gene regulation, chromatin remodeling, and autophagy. Mol Cell Endocrinol. 2017;458:160–168. doi: 10.1016/j.mce.2017.02.018. [DOI] [PubMed] [Google Scholar]
- 6.Lin CI, Whang EE, Donner DB, Du J, Lorch J, He F, Jiang X, Price BD, Moore FD, Jr, Ruan DT. Autophagy induction with RAD001 enhances chemosensitivity and radiosensitivity through Met inhibition in papillary thyroid cancer. Mol Cancer Res. 2010;8:1217–1226. doi: 10.1158/1541-7786.MCR-10-0162. [DOI] [PubMed] [Google Scholar]
- 7.Kim SH, Kang JG, Kim CS, Ihm SH, Choi MG, Yoo HJ, Lee SJ. Synergistic cytotoxicity of BIIB021 with triptolide through suppression of PI3K/Akt/mTOR and NF-κB signal pathways in thyroid carcinoma cells. Biomed Pharmacother. 2016;83:22–32. doi: 10.1016/j.biopha.2016.06.014. [DOI] [PubMed] [Google Scholar]
- 8.Pringle DR, Vasko VV, Yu L, Manchanda PK, Lee AA, Zhang X, Kirschner JM, Parlow AF, Saji M, Jarjoura D, et al. Follicular thyroid cancers demonstrate dual activation of PKA and mTOR as modeled by thyroid-specific deletion of Prkarla and Pten in mice. J Clin Endocrinol Metab. 2014;99:E804–E812. doi: 10.1210/jc.2013-3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Souza EC, Ferreira AC, Carvalho DP. The mTOR protein as a target in thyroid cancer. Expert Opin Ther Targets. 2011;15:1099–1112. doi: 10.1517/14728222.2011.594044. [DOI] [PubMed] [Google Scholar]
- 10.Petrulea MS, Plantinga TS, Smit JW, Georgescu CE, Netea-Maier RT. PI3K/Akt/mTOR: A promising therapeutic target for non-medullary thyroid carcinoma. Cancer Treat Rev. 2015;41:707–713. doi: 10.1016/j.ctrv.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 11.Prabahar A, Natarajan J. MicroRNA mediated network motifs in autoimmune diseases and its crosstalk between genes, functions and pathways. J Immunol Methods. 2017;440:19–26. doi: 10.1016/j.jim.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 12.Otsu H, Watanabe M, Inoue N, Masutani R, Iwatani Y. Intraindividual variation of microRNA expression levels in plasma and peripheral blood mononuclear cells and the associations of these levels with the pathogenesis of autoimmune thyroid diseases. Clin Chem Lab Med. 2017;55:626–635. doi: 10.1515/cclm-2016-0449. [DOI] [PubMed] [Google Scholar]
- 13.Li H, Ding G. Elevated serum inflammatory cytokines in lupus nephritis patients, in association with promoted hsa-miR-125a. Clin Lab. 2016;62:631–638. doi: 10.7754/Clin.Lab.2015.150812. [DOI] [PubMed] [Google Scholar]
- 14.Hu H, Hu S, Xu S, Gao Y, Zeng F, Shui H. miR-29b regulates Ang II-induced EMT of rat renal tubular epithelial cells via targeting PI3K/AKT signaling pathway. Int J Mol Med. 2018;42:453–460. doi: 10.3892/ijmm.2018.3579. [DOI] [PubMed] [Google Scholar]
- 15.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 16.Xia N, Chen G, Liu M, Ye X, Pan Y, Ge J, Mao Y, Wang H, Wang J, Xie S. Anti-inflammatory effects of luteolin on experimental autoimmune thyroiditis in mice. Exp Ther Med. 2016;12:4049–4054. doi: 10.3892/etm.2016.3854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buschur E, Sarma AV, Pietropaolo M, Dunn RL, Braffett BH, Cleary PA, Cowie C, Larkin ME, Wessells H, Nathan DM, et al. Self-reported autoimmune disease by sex in the diabetes control and complications trial/epidemiology of diabetes interventions and complications (DCCT/EDIC) study. Diabetes Care. 2014;37:e28–29. doi: 10.2337/dc13-1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Höfling DB, Chavantes MC, Juliano AG, Cerri GG, Knobel M, Yoshimura EM, Chammas MC. Low-level laser in the treatment of patients with hypothyroidism induced by chronic autoimmune thyroiditis: A randomized, placebo-controlled clinical trial. Lasers Med Sci. 2013;28:743–753. doi: 10.1007/s10103-012-1129-9. [DOI] [PubMed] [Google Scholar]
- 19.Lee J, Yi S, Kang YE, Chang JY, Kim JT, Sul HJ, Kim JO, Kim JM, Kim J, Porcelli AM, et al. Defective ciliogenesis in thyroid hürthle cell tumors is associated with increased autophagy. Oncotarget. 2016;7:79117–79130. doi: 10.18632/oncotarget.12997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu C, Wu F, Mao C, Wang X, Zheng T, Bu L, Mou X, Zhou Y, Yuan G, Wang S, Xiao Y. Excess iodine promotes apoptosis of thyroid follicular epithelial cells by inducing autophagy suppression and is associated with Hashimoto thyroiditis disease. J Autoimmun. 2016;75:50–57. doi: 10.1016/j.jaut.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 21.Kim JK, Yuk JM, Kim SY, Kim TS, Jin HS, Yang CS, Jo EK. MicroRNA-125a inhibits autophagy activation and antimicrobial responses during mycobacterial infection. J Immunol. 2015;194:5355–5365. doi: 10.4049/jimmunol.1402557. [DOI] [PubMed] [Google Scholar]
- 22.Raad H, Eskalli Z, Corvilain B, Miot F, De Deken X. Thyroid hydrogen peroxide production is enhanced by the Th2 cytokines, IL-4 and IL-13, through increased expression of the dual oxidase 2 and its maturation factor DUOXA2. Free Radic Biol Med. 2013;56:216–225. doi: 10.1016/j.freeradbiomed.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 23.Koc A, Batar B, Celik O, Onaran I, Tasan E, Sultuybek GK. Polymorphism of the NFKB1 affects the serum inflammatory levels of IL-6 in Hashimoto thyroiditis in a Turkish population. Immunobiology. 2014;219:531–536. doi: 10.1016/j.imbio.2014.03.009. [DOI] [PubMed] [Google Scholar]
- 24.Xian H, Wang F, Teng W, Yang D, Zhang M. Thyroid hormone induce a p53-dependent DNA damage through PI3K/Akt activation in sperm. Gene. 2017;615:1–7. doi: 10.1016/j.gene.2017.03.014. [DOI] [PubMed] [Google Scholar]
- 25.Zhu P, Liao LY, Zhao TT, Mo XM, Chen GG, Liu ZM. GPER/ERK&AKT/NF-κB pathway is involved in cadmium-induced proliferation, invasion and migration of GPER-positive thyroid cancer cells. Mol Cell Endocrinol. 2017;442:68–80. doi: 10.1016/j.mce.2016.12.007. [DOI] [PubMed] [Google Scholar]
- 26.Tang H, Li RP, Liang P, Zhou YL, Wang GW. miR-125a inhibits the migration and invasion of liver cancer cells via suppression of the PI3K/AKT/mTOR signaling pathway. Oncol Lett. 2015;10:681–686. doi: 10.3892/ol.2015.3264. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The analyzed data sets generated during the study are available from the corresponding author on reasonable request.