Abstract
Background
Carotid sinus syndrome (CSS) is an exaggerated response to carotid sinus baroreceptor stimulation, which may result in hypotension, prolonged asystole, and subsequently transient loss of consciousness due to cerebral hypoperfusion. However, this commonly benign syndrome may have lethal consequences under certain circumstances such as scuba diving.
Case summary
We report the case of a trained 73-year-old male diver, who survived an almost fatal diving accident without any neurological deficits due to cardiac arrest under water. After recovery and intensive diagnostics in the local hospital, the origin of cardiac arrest remained unclear. However, after referral to our tertiary care centre CSS could be diagnosed by provoking syncope and asystole with carotid sinus massage (CSM). Consequently, a leadless pacing system was implanted and his medical diving fitness could then be recertified.
Discussion
In conclusion, CSS may be an underdiagnosed cause of loss of consciousness. Thus, screening for CSS by CSM should be included in medical exams in senior athletes and specifically in senior divers.
Keywords: Carotid sinus syndrome, Carotid sinus massage, Cardiac arrest, Leadless pacing system, Diving accident, Case report
Learning points
Carotid sinus syndrome (CSS) may be an underdiagnosed cause of loss of consciousness with potential lethal consequences.
Carotid sinus massage should be included in medical examinations in elderly divers and athletes.
Asystole and syncope in cardio-inhibitory CSS can be prevented by cardiac pacing and a leadless intracardiac pacemaker is effective in CSS patients during scuba diving.
Introduction
Carotid sinus syndrome (CSS) is a quite common syndrome that is mostly benign, but carries a serious risk of syncope and cardiac arrest under special circumstances. It is caused by a hypersensitive carotid sinus, leading to marked bradycardia and/or hypotension and subsequently to reflex mediated syncope.1 An asystole lasting more than 3 s and/or a fall in systolic blood pressure of more than 50 mmHg defines carotid sinus hypersensitivity (CSH). If associated with spontaneous syncope, this abnormal response to carotid sinus massage (CSM) characterizes the diagnosis of CSS. Implantation of a pacemaker has become a recognized treatment of CSS, since pacing in patients with CSS could significantly reduce the number of syncope.2
Carotid sinus syndrome is well known in elderly people, however, details of incidence and manifestations have not been elucidated in sports activities like scuba diving. We report a rare case of CSS in a 73-year-old diver, who survived a cardiac arrest under water due to CSS. After pacemaker implantation, further asystole and syncope could be prevented. Thus, there may be a need for CSS screening in elderly people with potentially unsafe sports activities and prophylactic pacemaker therapy might be considered in individuals with CSH.1
Timeline
| Condition before incident | Excellent physical fitness w/o limitations |
|---|---|
| Time 0 | Cardiac arrest under water in Italy |
| 5 min | Transport to surface and start of CPR/AED |
| 20 min | Return of spontaneous circulation |
| 25 min | Transport to local hospital with helicopter |
| 45 min | Recovery w/o neurological deficit |
| Day 1 | ECG, echocardiography, computed tomography scans and coronary angiography w/o pathological findings |
| 1 week | Referral to our tertiary care centre and diagnosis of carotid sinus syndrome |
| 3 weeks | Implantation of a leadless pacing system (MICRA TCM) |
| 15 weeks | Asymptomatic scuba test dives and recertification of scuba diving fitness |
Case presentation
A well trained 73-year-old man with certified medical fitness for scuba diving participated in a rescue diver course at Lake Garda/Italy. The patient did not take any regular medication and had no history or symptoms of cardio- or cerebrovascular disease. Specifically, he did not suffer from prodromes, chest pain, or palpitations and there was no history of sudden cardiac death or unexplained collapses in his family. During scuba training different rescue techniques, such as salvage of a non-responsive diver from depth to surface, in water resuscitation and regular CPR techniques were trained. Due to the low water temperature, the diver was equipped with an additional ice vest with a neoprene hood that was exceptionally narrow at the neck. At the final dive of the course, he suddenly lost consciousness during the ascent at 6 m depth. The diver was immediately brought to surface and transported to the lakeshore by his dive buddies. At land, 5 min after the incident, CPR according to ERC guidelines (30:2 compression/ventilation ratio) was performed by the dive buddies after checking his vital signs (due to intense CPR training at the whole weekend a high quality CPR could be assumed). An AED was attached and a non-shockable rhythm was documented. After about 10 min, the paramedic team arrived and the first documented rhythm was asystole. Return of spontaneous circulation (ROSC) was achieved after administration of epinephrine and another 5 min of CPR. Further results of the paramedic team such as evidence of aspiration, vital signs, initial ECG after ROSC are unknown. The transport to the regional hospital by helicopter was without any abnormalities according to the medical report. In the ER cardiac examination showed an unremarkable 12-lead ECG (normofrequent sinus rhythm, no AV block or BBB, normal repolarization, no ventricular, or supraventricular extrasystoly), normal vital signs (RR, HR, respiratory rate, and SO2) and echocardiography without abnormalities [normal left ventricular function and right ventricular (RV) function, no signs of structural damage or cardiomyopathy, and minimal MR]. The patient was extubated without neurological deficit. During the following hospital stay ECG, echocardiography, computed tomography scans (to exclude a pulmonary embolism and lung injuries), and even coronary angiography did not show any pathological findings. The patient was subsequently repatriated to our tertiary care centre. The origin or cause of the cardiac arrest remained unclear according to the discharging physicians.
In our centre, the examination of the patient’s history and thorough reconstruction of events during the dive led to the conclusion that the patient passed out under water while turning his head left and upwards, possibly irritating his carotid sinus.
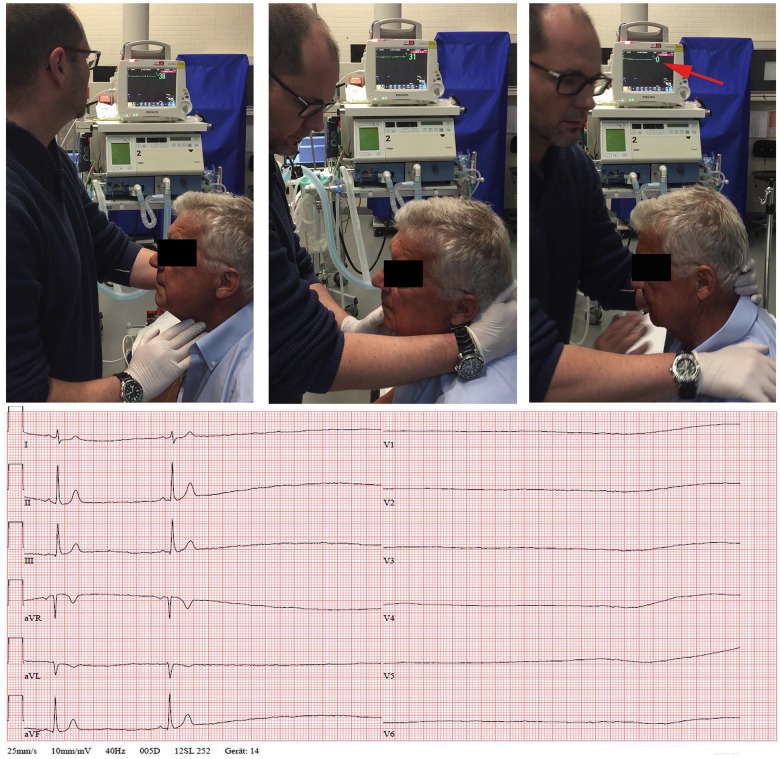
To confirm this hypothesis, CSM with the patient in upright position was performed, while monitoring blood pressure and heart rate. Immediately after massage, sinus arrest for more than 6 s on the monitor (Figure 1) in line with instantaneous syncope was documented. Importantly, blood pressure before and immediately after syncope remained unchanged. Thus, cardio-inhibitory CSH was diagnosed and asystole due to the tight-fitting ice vest was assumed. Based on the diagnostic findings and the results of the CSM, neither electrophysiological studies nor cardiac magnetic resonance imaging where considered necessary. Accordingly, implantation of a pacemaker was recommended. Due to the patient’s intense sports activities (diving, golf, and climbing) and a low expected ventricular pacing rate, a single chamber leadless pacing system was implanted.
Figure 1.
ECG rhythm strip during carotid sinus massage leading to asystole and syncope.
Specifically, a MICRA TPS system (Medtronic Inc., Minneapolis, MN, USA) was delivered to the septum of the right ventricle under radiologic guidance using a deflectable catheter via right femoral access. In the first position, excellent pacing parameters and adequate fixation by the four tines was achieved and the system was programmed in a VVI 40 b.p.m. mode.
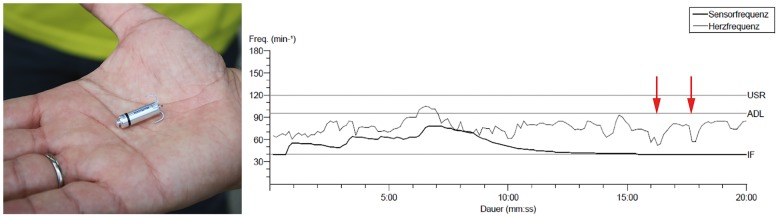
In a follow-up visit 4 weeks after the incident, repeated carotid manipulations could neither provoke asystole nor syncope or other symptoms. Also, blood pressure was normal and not supressed during the test. Twelve weeks after device implantation a test-dive in confined water (24°C, pool 5 m depth) under CPR standby was performed. During the dive, CSM did not provoke any symptoms, whereas drops of the heart rate were documented on pacemaker telemetry (Figure 2). Furthermore, no arrhythmias could be detected during ECG monitoring (Figure 3) in an escorted cold-water scuba dive (8°C, 12 m depth). Finally, regular pacemaker follow-ups showed 1% ventricular pacing without causing any symptoms in the patient. Thus, the patient’s medical fitness for scuba diving was recertified and he did not experience any problems in his further dive or sports activities.
Figure 2.
MICRA VR TPS system (Medtronic Inc.®, USA) telemetry report of heart rate trend during test dive in a swimming pool 3 months after implantation. Base rate of the device was programmed to 40 b.p.m. The light grey line indicates actual heart rate, the black line sensor activation during 20 min of diving. Carotid sinus massages, indicated by the red arrows, resulted in a drop of heart rate. However, the TPS device prevented asystole and heart rate drop below 40 b.p.m.
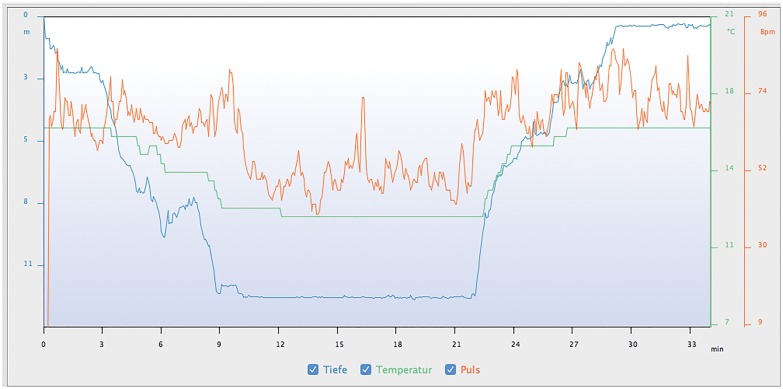
Figure 3.
ECG monitoring after pacemaker implantation during a cold-water dive (12 msw, 12°C). Pronounced by a vagal diving reflex in cold water the heart rate drops with decreasing water temperature (blue—depth, green—temperature, and orange—heart rate).
Discussion
To our knowledge, this is the first reported case of a patient with CSS leading to cardiac arrest under water. Overall outcome of in-water resuscitation remains very poor due to technical difficulties.3,4 In our case, the perfect training of the dive team as well as the following diagnostic workup was the key of success. The pathophysiologic mechanisms of underwater cardiac arrest are multifactorial, but CSS may be an underestimated risk in the elderly diver.
Carotid sinus hypersensitivity is an exaggerated response to carotid sinus baroreceptor stimulation, which may result in decreased heart rate, prolonged asystole, and/or hypotension. If this reflex reproducibly leads to transient loss of consciousness due to cerebral hypoperfusion, the diagnosis of CSS is confirmed.1 The incidence of CSS varies widely in literature between 1% and 60%,5 however, the rate of positive responses to CSM increases with age, ranging from 4% in patients <40 years up to 41% in patients >80 years.6 The response can be pronounced by a vagal diving reflex in cold water, as seen in the ECG tracings even after pacemaker implantation (Figures 2 and 3). Moreover, CSS may be a risk factor for a potentially life threatening loss of consciousness in other sports activities like swimming, aviation, or climbing. Too tight suits (especially in the area of the neck) or strong head rotations with effort can cause headache, physical, and psychological unease up to life-threatening cardiological pathologies under these circumstances (Figure 4).
Figure 4.
Compressed area of the neck due to the latex seal. Tight latex seal of a dry suit (right) or thick neoprene ice vest (left) can stimulate the carotid sinus.
The current ESC guidelines for diagnosis and management of syncope recommend CSM in patients with a history of syncope of unknown origin >40 years of age (Class I) and advocate pacemaker implantation (Class IIa), if cardio-inhibitory CSS is confirmed.1 However, recommendations for pre-participation screening of athletes do not specifically address CSS screening or sports eligibility of senior athletes.7,8 Given the high prevalence and the potential lethal consequences of CSH, inclusion of CSM in physical examination protocols of medical fitness tests for scuba divers and athletes with specific sports activities should be considered especially in elderly individuals. Furthermore, prophylactic pacemaker implantation even before the occurrence of syncope may be appropriate in these individuals, if CSM leads to prolonged asystole.
Pacing can be a therapeutic option preventing critical bradycardia as well as loss of consciousness, even in divers. Cardiac arrest and subsequent resuscitation as described in the current case could have been prevented by thorough clinical testing, diagnosis of CSS, and prophylactic implantation of a pacemaker.9 However, in our case a conventional pacemaker system was not the first choice for several reasons. First, the patient was not pacemaker-dependent in sinus rhythm and a low amount of RV pacing was anticipated. Second, a conventional pacemaker with a subcutaneous generator can be damaged by excessive pressure changes. Thus, available pacemaker generators are usually not approved for scuba diving or rated to a maximum of 3–4 atmospheres (ATA) or 20–30 m depth. Third, lead dislocation or damage might be a problem with extensive arm movements in several sports activities like climbing, golf, tennis, etc. and this risk can even be higher with a close-fitting harness together with the heavy scuba dive gear. Accordingly, a leadless pacer was implanted directly to the right ventricle, since this system carries a lower risk of complications and might be less sensitive to pressure changes than conventional pacemakers due to its cylindrical shape and smaller volume.
The implanted MICRA TPS pacemaker system (Medtronic Inc.®, USA) is not officially certified for scuba diving and further studies are required to prove its safety under hyperbaric conditions. So far, the International Standards Organization (ISO) has not approved a standardized pressure test for implantable pulse generators that are exposed to hyperbaric oxygen therapy or scuba diving. However, one manufacturer evaluated device performance upon exposure to elevated atmospheric pressures. During laboratory testing, all devices in a statistically significant sample continued to function as designed when exposed to pressures up to 5.0 ATA.10
In conclusion, this is the first observation that a leadless pacer is working properly under water and is able to prevent recurrent syncope in a scuba diver. However, further technical testing of the TPS system is warranted.
Conclusions
Carotid sinus syndrome may be an underdiagnosed cause of loss of consciousness with potential lethal consequences. Thus, screening for CSS by CSM should be included in medical exams, especially in senior athletes and divers. Asystole and loss of consciousness in cardio-inhibitory CSS can be prevented by pacemaker implantation. Although scientific evidence for diving in patients with leadless pacemakers are scarce, adequate operation of the system is shown in this case report.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1. Brignole M, Moya A, de Lange FJ, Deharo JC, Elliott PM, Fanciulli A, Fedorowski A, Furlan R, Kenny RA, Martín A, Probst V, Reed MJ, Rice CP, Sutton R, Ungar A, van Dijk JG. ESC guidelines for the diagnosis and management of syncope. Eur Heart J 2018;39:1883–1948. [DOI] [PubMed] [Google Scholar]
- 2. Brignole M. Carotid sinus syndrome. An article from the e-journal of the ESC Council for Cardiology Practice. Vol. 6, N° 30–07 Apr 2008.
- 3. Winkler BE, Hartig F, DuCanto J, Koch A, Georgieff M, Lungwitz YP, Muth C-M.. Helicopter-based in-water resuscitation with chest compressions: a pilot study. Emerg Med J 2015;32:553–558. [DOI] [PubMed] [Google Scholar]
- 4. DuCanto J, Lungwitz Y, Koch A, Kähler W, Gessell L, Simanonok J, Roewer N, Kranke P, Winkler BE.. Mechanical ventilation and resuscitation under water: Exploring one of the last undiscovered environments—a pilot study. Resuscitation 2015;93:40–45. [DOI] [PubMed] [Google Scholar]
- 5. Disertori M, Brignole M, Menozzi C, Raviele A, Rizzon P, Santini M, Proclemer A, Tomasi C, Rossillo A, Taddei F, Scivales A, Migliorini R, De Santo T. Management of syncope referred for emergency to general hospitals. Europace 2003;5:283–291. [DOI] [PubMed] [Google Scholar]
- 6. Puggioni E, Guiducci V, Brignole M, Menozzi C, Oddone D, Donateo P, Croci F, Solano A, Lolli G, Tomasi C, Bottoni N.. Results and complications of the carotid sinus massage performed according to the “Methods of Symptoms”. Am J Cardiol 2002;89:599–601. [DOI] [PubMed] [Google Scholar]
- 7. Mont L, Pelliccia A, Sharma S, Biffi A, Borjesson M, Brugada Terradellas J, Carré F, Guasch E, Heidbuchel H, La Gerche A, Lampert R, McKenna W, Papadakis M, Priori SG, Scanavacca M, Thompson P, Sticherling C, Viskin S, Wilson M, Corrado D, Lip GYH, Gorenek B, Blomström Lundqvist C, Merkely B, Hindricks G, Hernández-Madrid A, Lane D, Boriani G, Narasimhan C, Marquez MF, Haines D, Mackall J, Manuel Marques-Vidal P, Corra U, Halle M, Tiberi M, Niebauer J, Piepoli M.. Pre-participation cardiovascular evaluation for athletic participants to prevent sudden death: Position paper from the EHRA and the EACPR, branches of the ESC. Endorsed by APHRS, HRS, and SOLAECE. Eur J Prev Cardiol 2017;24:41–69. [DOI] [PubMed] [Google Scholar]
- 8. Pelliccia A, Fagard R, Bjørnstad HH, Anastassakis A, Arbustini E, Assanelli D, Biffi A, Borjesson M, Carrè F, Corrado D, Delise P, Dorwarth U, Hirth A, Heidbuchel H, Hoffmann E, Mellwig KP, Panhuyzen-Goedkoop N, Pisani A, Solberg EE, van-Buuren F, Vanhees L, Blomstrom-Lundqvist C, Deligiannis A, Dugmore D, Glikson M, Hoff PI, Hoffmann A, Hoffmann E, Horstkotte D, Nordrehaug JE, Oudhof J, McKenna WJ, Penco M, Priori S, Reybrouck T, Senden J, Spataro A, Thiene G. Recommendations for competitive sports participation in athletes with cardiovascular disease: a consensus document from the study group of sports cardiology of the working group of cardiac rehabilitation and exercise physiology and the working group of myocardial and pericardial diseases of the European Society of Cardiology. Eur Heart J 2005;26:1422–1445. [DOI] [PubMed] [Google Scholar]
- 9. Claesson JE, Kristensson BE, Edvardsson N, Währborg P.. Less syncope and milder symptoms in patients treated with pacing for induced cardioinhibitory carotid sinus syndrome: a randomized study. Europace 2007;9:932–936. [DOI] [PubMed] [Google Scholar]
- 10. Boston Scientific. Elevated Pressure (HBOT/SCUBA) and Implanted Medical Devices. Boston Scientific; 2015. www.bostonscientific.com [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.