Abstract
Substance abuse can have strong negative impacts on surgical outcomes. Therefore, this study assessed the effects of drug abuse in total knee arthroplasty (TKA) patients. Specifically, we identified revision TKA (RTKA): (1) incidence, (2) causes, (3) time to revision, and (4) patient demographics in patients with a history of drug abuse. The Medicare database within the PearlDiver Supercomputer (Warsaw, IN) was queried to identify 2,159,221 TKAs performed between 2005 and 2012. Drug abuse was subdivided into cocaine, cannabis, opioids, sedatives/hypnotics/anxiolytics (SHA), amphetamines, and alcohol abusers. The effect of drug use on the incidence and cause for RTKA, time to revision, as well as patient demographics were correlated using multivariate, analysis of variance, and regression analyses. There was a significant increase in the number of primary TKAs in cocaine (p = 0.011), cannabis (p < 0.001), opioid (p < 0.001), SHA (p < 0.001), amphetamine (p < 0.001), and alcohol (p < 0.001) users. Amphetamine users had the fastest mean time to revision (691 days, standard deviation: 679 days). At 30-, 90-day, and 6-month postoperative, cocaine had the highest proportion of patients requiring RTKA (7, 12, and 20%, respectively), and at 1-year alcohol abusers (38%, p < 0.001). Infection was the most common cause of revision in all drug abuse/dependent cohorts. Age distributions varied significantly by group for primary TKA (p < 0.001). Comorbidity status was similar in all RTKA patients as determined by comparison of the mean Charlson comorbidity index scores (p = 0.091). Based on these results, drug abuse patients are at increased risk for RTKA. These high-risk patients should, therefore, be appropriately risk stratified and receive comprehensive postoperative pain management.
Keywords: knee, illicit, drug, arthroplasty, revision, replacement
Illicit drugs, such as cocaine, cannabis, opioids, sedatives/ hypnotics/anxiolytics (SHA), amphetamines, and alcohol, have been thought to have a strongly negative impact on surgical outcomes. In particular, illicit drug abuse and dependence in joint arthroplasty are thought to increase the rates of postoperative infection and septic complications which can require revision surgery.1–4 Drug abuse in the United States is common, as it has been estimated that approximately 46% of the U.S. population aged 12 years and older have tried an illicit drug in their lifetime.5 In addition, the lifetime prevalence of drug abuse and dependence among U.S. adults is 8 and 3%, respectively.6 In 2015 alone, it was estimated that more than 33,000 deaths were attributable to illicit drugs.7
Recently, the United States has experienced the rise of an opioid epidemic; so much so that the White House has declared the opioid crisis a public health emergency.8 A large part of this problem is the use of opioids for acute or chronic pain by more than 125 million Americans.7 Additionally, for some medical specialties, such as orthopaedics, the use of opioids is almost a necessity for pain control.9 In fact, in a recent study by Kaafarani et al, the group found orthopaedics to be one of the highest opioid prescribing services at the Massachusetts General Hospital.10 Although opioids remain a common medication class for postoperative management, some studies have found that patients with a history of chronic opioid use have worse pain management outcomes following to total hip or total knee arthroplasty (TKA).11,12 However, because of the rising number of opioid users, as well as the continuous increase in orthopaedic procedures, the association between drug use and TKA needs to be more clearly identified.
Illicit drug use and prescription drug abuse are two independent factors that might have consequences resulting in revision TKA (RTKA). Currently, the effects of drug abuse in RTKA have not been adequately studied. Previous studies that have investigated the effect of drug abuse in total joint arthroplasty have primarily focused on the hip, or have only analyzed small sample sizes.2,3 Therefore, the purpose of this study was to determine the effects of drug abuse in TKA patients who eventually needed a revision using a large nationwide database. Specifically, we used the Medicare database from 2005 to 2012 to identify RTKA: (1) incidence, (2) causes, and (3) time to RTKA in patients with a history of abusing cocaine, cannabis, opioids, SHA, amphetamines, and/or alcohol. Drug user patient demographics were also correlated with RTKA.
Methods
Data Source
A retrospective review of a comprehensive Medicare database within the PearlDiver Supercomputer application (Warsaw, IN) for TKA and RTKA procedure was performed. The PearlDiver database is a publicly available, Health Insurance Portability and Accountability Act compliant national database compiled from a collection of U.S. Medicare records. This database contains current procedural terminology (CPT) and International Classification of Diseases, Ninth Revision (ICD-9) codes from January 1, 2005, to December 31, 2014.
Patient Selection
Patients who underwent primary TKA were identified by CPT 27447 and ICD-9 81.54. RTKA patients were identified with CPT-27486, CPT-27487, ICD-9 00.80–00.84, and ICD-9 81.55. Causes for revision were identified with ICD-9 codes 996.41, 996.43, 996.44, 996.45, 996.66–67, 998.59, 996.77, 718.46, 718.86, and 716.16 (Appendix A). Drug abuse and dependency was subdivided, based on respective ICD-9 codes (i.e., independent codes for abuse and dependence) into cocaine (ICD-9-D-304.20–22, ICD-9-D-305.60–62), cannabis (ICD-9- D-304.30–32, ICD-9-D-305.20–22), opioids (ICD-9-D-304.00–02, ICD-9-D-305.50–52), SHA (ICD-9-D-304.10–12, ICD-9-D-305.40–42), hallucinogens (ICD-9–304.50–52, ICD- 9-D-305.30–32), amphetamines (ICD-9-D-304.40–42, ICD- 9-D-305.70–72), and alcohol (ICD-9-D-303.90–92, ICD-9-D-305.00–02). For the purpose of this study, patients with defined dependency or abuse, as per ICD-9 code, were analyzed as the same cohort. Our query returned 2,729,006 primary TKAs performed between 2005 and 2014.
Data Analysis
Study end points were annual volume and incidence changes for the above-defined patients undergoing RTKA. These end points were assessed through linear regressions models. Mean values were compared through a one-way analysis of variance (ANOVA) with post hoc evaluations using Bonferroni correction. Chi-square testing was also performed to evaluate distribution of time to revision among groups. Significance was set at an a of 0.05. All tests were performed with SPSS (Version 20, IBM Corporation, Armonk, NY).
Results
Over the 10-year study period, there was a significant increase in the number of primary TKAs performed (p < 0.001), as well as, TKA in cocaine (p = 0.011), cannabis (p < 0.001), opioid (p < 0.001), SHA (p < 0.001), amphetamine (p < 0.001), and alcohol (p < 0.001; fig. 1) users. There was a significant increase in the number of RTKA performed from 2005 to 2014; however, no significant increases in number of RTKA by drug abuse/dependence were observed (Table 1). Nevertheless, 9% (n = 248,098) of patients in the general population underwent RTKA compared with an average of 12.9% of drug and alcohol abusers/dependent patients required RTKA, which was found to be significant (p < 0.001). Post hoc Bonferroni testing demonstrated that cocaine use was associated with a significantly higher revision rate (15.1%), followed by amphetamines (13.7%) and opioids (12.9%, p < 0.001; Table 1).
Fig. 1.
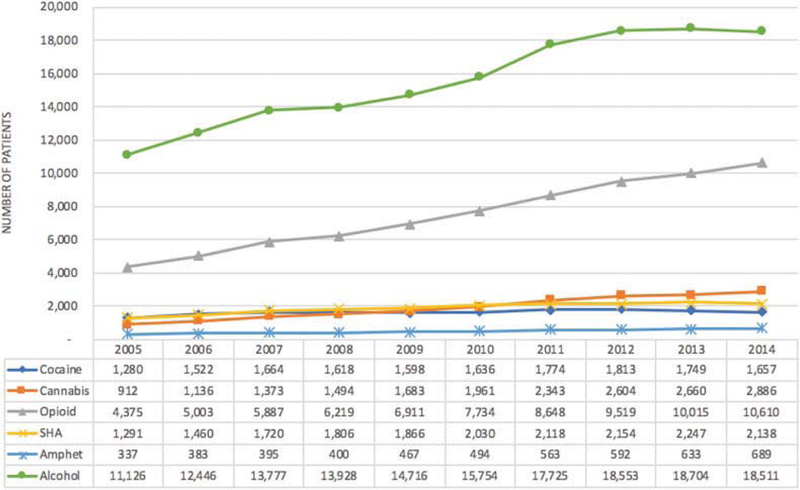
Primary total knee arthroplasty by drug dependence/abuse.
Table 1.
Revision TKA by drug abuse or dependency
| Year | Revision TKA | Cocaine | Cannabis | Opioid | SHA | Amphetamines | Alcohol | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2005 | 22,165 | 8.4% | 209 | 16.3% | 123 | 13.5% | 631 | 14.4% | 163 | 12.6% | 37 | 11.0% | 911 | 8.2% |
| 2006 | 22,096 | 8.4% | 229 | 15.0% | 166 | 14.6% | 795 | 15.9% | 193 | 13.2% | 55 | 14.4% | 1,115 | 9.0% |
| 2007 | 22,961 | 8.6% | 282 | 16.9% | 242 | 17.6% | 954 | 16.2% | 239 | 13.9% | 65 | 16.5% | 1,299 | 9.4% |
| 2008 | 23,334 | 8.7% | 263 | 16.3% | 256 | 17.1% | 1,074 | 17.3% | 287 | 15.9% | 62 | 15.5% | 1,331 | 9.6% |
| 2009 | 23,777 | 8.9% | 279 | 17.5% | 284 | 16.9% | 1,157 | 16.7% | 269 | 14.4% | 82 | 17.6% | 1,409 | 9.6% |
| 2010 | 24,855 | 8.9% | 280 | 17.1% | 322 | 16.4% | 1,247 | 16.1% | 292 | 14.4% | 87 | 17.6% | 1,421 | 9.0% |
| 2011 | 26,632 | 9.9% | 283 | 16.0% | 323 | 13.8% | 1,191 | 13.8% | 280 | 13.2% | 84 | 14.9% | 1,387 | 7.8% |
| 2012 | 27,187 | 9.8% | 256 | 14.1% | 282 | 10.8% | 1,043 | 11.0% | 245 | 11.4% | 74 | 12.5% | 1,338 | 7.2% |
| 2013 | 27,693 | 9.6% | 208 | 11.9% | 250 | 9.4% | 907 | 9.1% | 220 | 9.8% | 68 | 10.7% | 1,100 | 5.9% |
| 2014 | 27,398 | 9.7% | 170 | 10.3% | 188 | 6.5% | 682 | 6.4% | 167 | 7.8% | 63 | 9.1% | 827 | 4.5% |
| Total | 248,098 | 9.1% | 2,459 | 15.1% | 2,436 | 12.8% | 9,681 | 12.9% | 2,355 | 12.5% | 677 | 13.7% | 12,138 | 7.8% |
| p-Value | <0.001 | <0.001 | 0.464 | 0.022 | 0.195 | 0.210 | 0.612 | 0.007 | 0.789 | 0.034 | 0.110 | 0.267 | 0.909 | 0.010 |
Abbreviations: SHA, sedatives/hypnotics/anxiolytics; TKA, total knee arthroplasty.
The mean time to RTKA in the general population was 821 days (standard deviation [SD]: 741 days). Amphetamine users had the fastest mean time to revision (691 days, SD: 679 days); however, there was no significant difference in time to revision across different drug abuse cohorts (ANOVA, p = 0.0978; Table 2). At 30-, 90-day, and 6-month post-operative, cocaine had the highest proportion of patients requiring RTKA (7, 12, and 20%, respectively), and at 1-year alcohol abusers (38%, p < 0.001; Table 3). Infection was the most common cause of revision in all drug abuse/dependent cohorts ( Table 4).
Table 2.
Mean time to revision (in days)
| Time (in days) | Revision TKA | Cocaine | Cannabis | Opioid | SHA | Amphetamines | Alcohol |
|---|---|---|---|---|---|---|---|
| Mean | 821 | 730 | 739 | 804 | 769 | 691 | 756 |
| Standard deviation |
740.9 | 674.5 | 685.5 | 717.2 | 681.2 | 679.3 | 712.0 |
Abbreviations: SHA, sedatives/hypnotics/anxiolytics; TKA, total knee arthroplasty.
Table 3.
Time to revision (%)
| Time | Revision TKA | Cocaine | Cannabis | Opioid | SHA | Amphetamines | Alcohol |
|---|---|---|---|---|---|---|---|
| 30 d | 4–5% | 7% | 6% | 3–4% | 4% | 5–6% | 6–7% |
| 90 d | 8% | 12% | 11% | 8% | 9% | 12% | 12% |
| 6 mo | 16% | 20% | 20% | 17% | 19% | 25% | 20% |
| 1 y | 33% | 36% | 37% | 32% | 34% | 42% | 38% |
| Chi-square | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Abbreviations: SHA, sedatives/hypnotics/anxiolytics; TKA, total knee arthroplasty.
Table 4.
Causes for revision total knee arthroplasty by drug abuse or dependency
| Cause | Rev | Cocaine | Cannabis | Opioid | SHA | Amphetamines | Alcohol | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mechanical loosening |
23,563 | 9.5% | 214 | 8.7% | 259 | 10.6% | 1,065 | 11.0% | 247 | 10.5% | 66 | 9.7% | 1,139 | 9.4% |
| Failure/break | 7,093 | 2.9% | 60 | 2.4% | 69 | 2.8% | 360 | 3.7% | 82 | 3.5% | 19 | 2.8% | 351 | 2.9% |
| Periprosthetic fracture |
3,457 | 1.4% | 29 | 1.2% | 32 | 1.3% | 199 | 2.1% | 51 | 2.2% | 11 | 1.6% | 200 | 1.6% |
| Osteolysis | 1,860 | 0.7% | 15 | 0.6% | 18 | 0.7% | 87 | 0.9% | 18 | 0.8% | <11 | N/A | 78 | 0.6% |
| Infection | 39,385 | 15.9% | 441 | 17.9% | 547 | 22.5% | 2,107 | 21.8% | 462 | 19.6% | 161 | 23.8% | 2,535 | 20.9% |
| Pain-joint replacement |
29,667 | 12.0% | 328 | 13.3% | 363 | 14.9% | 1,502 | 15.5% | 363 | 15.4% | 102 | 15.1% | 1,509 | 12.4% |
| Arthrofibrosis | 7,204 | 2.9% | 87 | 3.5% | 81 | 3.3% | 344 | 3.6% | 70 | 3.0% | 19 | 2.8% | 335 | 2.8% |
| Instability | 3,999 | 1.6% | 49 | 2.0% | 70 | 2.9% | 269 | 2.8% | 72 | 3.1% | 17 | 2.5% | 263 | 2.2% |
| Trauma | 1,224 | 0.5% | 42 | 1.7% | 53 | 2.2% | 144 | 1.5% | 43 | 1.8% | 18 | 2.7% | 141 | 1.2% |
Abbreviation: SHA, sedatives/hypnotics/anxiolytics.
Patient demographics for primary TKA by drug abuse/ dependence type are demonstrated in Table 5. Age distributions varied significantly by group for primary TKA (p < 0.001) chi-squared. The mean Charlson comorbidity index (CCI) for primary TKA in the general population was 4.75 (SD: 1.9). CCI comparison among drug abuse/dependency cohorts, excluding primary TKA in the general population demonstrated significant differences (p < 0.001). Tukey honest significant difference post hoc testing demonstrated that significant difference in CCI for primary TKA were seen between cannabis and opioid (4.33 vs. 4.78, p = 0.0065), cannabis and alcohol (4.33 vs. 4.90, p = 0.0001), and amphetamines and alcohol (4.37 vs. 4.90, p = 0.0147). Comorbidity status was similar in all RTKA patients as determined by comparison of the mean CCI scores (p = 0.091; Table 6).
Table 5.
Primary TKA demographics by substance abuse or dependency
| Demographic variable |
Rev | Cocaine | Cannabis | Opioid | SHA | Amphetamines | Alcohol |
|---|---|---|---|---|---|---|---|
| Age | |||||||
| Unknown | 33,809 | 245 | 175 | 803 | 198 | 56 | 1,952 |
| < 65 | 240,896 | 5,502 | 6,983 | 18,604 | 5,081 | 1,799 | 19,988 |
| 65–69 | 691,166 | 572 | 1,327 | 8,090 | 2,118 | 338 | 21,562 |
| 70–74 | 627,124 | 242 | 652 | 6,838 | 1,802 | 208 | 22,389 |
| 75–79 | 513,325 | 74 | 231 | 4,433 | 1,162 | 115 | 17,042 |
| 80–84 | 303,594 | 18 | 99 | 2,357 | 593 | 50 | 9,402 |
| > 85 | 117,677 | (1) | 43 | 981 | 219 | 23 | 3,596 |
| Gender | |||||||
| Female | 1,513,683 | 3,114 | 4,349 | 22,282 | 6,387 | 1,390 | 25,616 |
| Male | 846,550 | 2,864 | 4,070 | 9,703 | 2,303 | 839 | 41,263 |
| Unknown | 33,809 | 245 | 175 | 803 | 198 | 56 | 1,953 |
| Comorbidity burden | |||||||
| CCI (SD) | 4.75 (1.9) | 4.57 (2.61) | 4.33 (2.37) | 4.78 (2.46) | 4.68 (2.34) | 4.37 (2.39) | 4.90 (2.27) |
Abbreviations: CCI, Charlson comorbidity index; SD, standard deviation; SHA, sedatives/hypnotics/anxiolytics; TKA, total knee arthroplasty.
Table 6.
Revision TKA demographics by substance abuse or dependency
| Demographic variable |
Rev | Cocaine | Cannabis | Opioid | SHA | Amphetamines | Alcohol |
|---|---|---|---|---|---|---|---|
| Age | |||||||
| Unknown | 2,549 | 35 | 22 | 134 | 28 | <11 | 191 |
| < 65 | 38,730 | 741 | 844 | 2,605 | 667 | 224 | 2,248 |
| 65–69 | 52,202 | 49 | 82 | 779 | 182 | 34 | 1,315 |
| 70–74 | 49,589 | <11 | 27 | 548 | 121 | <11 | 1,162 |
| 75–79 | 42,732 | <11 | 13 | 277 | 56 | <11 | 762 |
| 80–84 | 27,865 | <11 | <11 | 113 | 20 | 0 | 336 |
| > 85 | 14,151 | <11 | <11 | 29 | <11 | 0 | 85 |
| Gender | |||||||
| Female | 131,756 | 396 | 481 | 2,395 | 649 | 144 | 1,708 |
| Male | 83,991 | 373 | 435 | 1,205 | 243 | 110 | 2,801 |
| Unknown | 2,549 | 35 | 22 | 134 | 28 | <11 | 191 |
| Comorbidity burden | |||||||
| CCI (SD) | 5.24 (2.36) | 4.44 (2.65) | 4.23 (2.38) | 4.35 (2.31) | 4.42 (2.42) | 4.29 (2.43) | 4.58 (2.33) |
Abbreviations: CCI, Charlson comorbidity index; SD, standard deviation; SHA, sedatives/hypnotics/anxiolytics; TKA, total knee arthroplasty.
Discussion
Although there are a few prior studies investigating the effects of substance abuse on joint arthroplasty, these studies do not address specific illicit drugs.1,2,4 Thus, the purpose of this study was to determine the effects of individual illicit drug abuse on RTKA incidence, causes, and time to revision, as well as correlate drug user patient demographics with RTKA using a Medicare patient population database. The results of this study show that illicit drug use, in general, increases the risk for revision and on average, and all illicit drug abuse lead to earlier revision.
This study is not without limitations. The PearlDiver database is reliant upon accurate CPT or ICD codes, which creates the potential for a reporting bias. Additionally, we do not have information on the implant used, prosthesis fixation method, patient bone quality, and data regarding which component failed. Furthermore, patient demographics as well as time and amount of drug use could not be determined. Also, we were not able to differentiate illicit opioid abuse versus prescription opioid abuse. Therefore, the opioid abuse patients analyzed in this article encompass all patients with cause for RTKA identified to be opioids based on ICD-9 codes 304.00–02 and 305.50–52 as a single cohort. Nevertheless, this study analyzes more than 2 million TKA cases from a large national patient population database. Additionally, this study investigated the specific drugs abused and the causes of RTKA in subgroups that have not been previously adequately studied in the literature.
Similar to our study, other studies have found analogous results. Dufour et al13 performed a retrospective study analyzing the prevalence of diagnosed opioid abuse in commercial versus Medicare patient populations. The group found an increased 6-month prevalence of diagnosed opioid abuse in the Medicare patient population from 3.17 to 6.35 per 1,000 patients, during January 1, 2008, to June 30, 2010, while for commercial patients, the increase was only from 0.84 to 1.15 during the same time period. Bozic et al14 performed a study analyzing the Medicare patient population and risk factors for early RTKA. The group found that drug abusers had a higher risk for early revision when compared with nondrug abusers (hazard ratio [HR], 2.08; 95% confidence interval, 1.17–3.72 compared with an overall HR, 1.14).
Another study performed by Zywiel et al11 comparing 49 patients with a mean age of 56 years (range, 37–78) who underwent TKA after 6 or more weeks of chronic opioid use for pain control and to a matched cohort of nonopioid users. The group found Knee Society scores (KSSs) to be significantly lower in opioid abusers at final follow-up (mean, 3 years; range, 2–7 years). Opioid abusers had a mean KSS of 79 points (range, 45–100 points), while nonopioid patients had a mean of 92 points (range, 59–100 points). Additionally, opioid abusers underwent a significantly higher number of surgical procedures to help resolve unexplained knee stiffness or pain than nonopioid users (11 vs. 0, p < 0.001). The study also found that chronic opioid use prior to TKA contributed to a 16% revision rate, consistent with the results of our study.
Based on the results of ours and the above studies, there is clearly a strong correlation between drug abuse and adverse primary TKA outcomes, potentially resulting in RTKA. Based on these results, therefore, a more targeted approach should be made when managing pain in orthopaedic patients. Specifically, patients and physicians need to keep in mind that it has been well documented in the literature that patients have poorer pain outcomes and are more likely to be opioid/drug dependent postoperatively if treated with opioids preoperatively.11,15 Additionally, as noted in this study, certain drugs, such as alcohol, opioids, and cannabis, can put patients at higher risk for TKA complications. Recent literature has suggested the use of nonopioid management techniques, such as intraoperative local infiltration analge- sia16 or peripheral nerve blocks.17 However, specifically for drug abuse patients, these newer potential treatment options should be coupled with risk stratification, as well as a more holistic and life-style altering approach to pain management.18–20
Conclusion
The prevalence of drug abuse patients, particularly Medicare patients, is of substantial concern, and will remain a concern until marked changes are made to the way these patients managed. Therefore, studies such as this are critical in identifying specific incidences and prevalences, specific illicit drugs abused, and patient demographics, to target and improve patient care. Although alcohol and opioids are the most abused substances, cocaine abuse holds the highest risk for revision. However, those who abuse cannabis are more likely to need an RTKA sooner than those who use other substances, particularly in the 30- and 90-day postoperative day intervals. Infection remains one of the most common causes of revision post- TKA regardless of the substance abused. The results of this study help highlight the strong correlation between drug abuse and RTKA. Based on these results, therefore, drug abuse patients should therefore be appropriately risk stratified and receive comprehensive postoperative pain management.
Footnotes
Conflict of Interest
M.R.: Stryker, Orthosensor; T.Y.L.: Smith & Nephew, Stryker; M.A.M.: AAOS, Abbott, Cymedica, DJ Orthopaedics, Johnson & Johnson, Journal of Arthroplasty, Journal of Knee Surgery, Mallinckrodt Pharmaceuticals, Microport, National Institutes of Health (NIAMS & NICHD), Ongoing Care Solutions, Orthopedics, Orthosensor, Pacira, Peerwell, Performance Dynamics Inc., Sage, Stryker, Surgical Technologies International, Kolon TissueGene. The remaining authors report no conflict of interest.
References
- 1.Gordon RJ, Lowy FD. Bacterial infections in drug users. N Engl J Med 2005;353(18):1945–1954 [DOI] [PubMed] [Google Scholar]
- 2.Wieser K, Zingg PO, Betz M, Neubauer G, Dora C. Total hip replacement in patients with history of illicit injecting drug use. Arch Orthop Trauma Surg 2012;132(07):1037–1044 [DOI] [PubMed] [Google Scholar]
- 3.Lehman CR, Ries MD, Paiement GD, Davidson AB. Infection after total joint arthroplasty in patients with human immunodeficiency virus or intravenous drug use. J Arthroplasty 2001;16(03):330–335 [DOI] [PubMed] [Google Scholar]
- 4.Best MJ, Buller LT, Klika AK, Barsoum WK. Outcomes following primary total hip or knee arthroplasty in substance misusers. J Arthroplasty 2015;30(07):1137–1141 [DOI] [PubMed] [Google Scholar]
- 5.Schulden JD, Thomas YF, Compton WM. Substance abuse in the United States: findings from recent epidemiologic studies. Curr Psychiatry Rep 2009;11(05):353–359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry 2007;64(05):566–576 [DOI] [PubMed] [Google Scholar]
- 7.Skolnick P The opioid epidemic: crisis and solutions. Annu Rev Pharmacol Toxicol 2018;58:143–159 [DOI] [PubMed] [Google Scholar]
- 8.Hargan ED. Determiniation That a Public Health Emergency Exists. Available at: https://www.hhs.gov/sites/default/files/opioidPHE-Declaration-no-sig.pdf. Accessed August 26, 2018
- 9.Goesling J, Moser SE, Zaidi B, et al. Trends and predictors of opioid use after total knee and total hip arthroplasty. Pain 2016;157(06): 1259–1265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaafarani HM, Weil E, Wakeman S, Ring D. The opioid epidemic and new legislation in Massachusetts: time for a culture change in surgery? Ann Surg 2017;265(04):731–733 [DOI] [PubMed] [Google Scholar]
- 11.Zywiel MG, Stroh DA, Lee SY, Bonutti PM, Mont MA. Chronic opioid use prior to total knee arthroplasty. J Bone Joint Surg Am 2011;93(21):1988–1993 [DOI] [PubMed] [Google Scholar]
- 12.Pivec R, Issa K, Naziri Q, Kapadia BH, Bonutti PM, Mont MA. Opioid use prior to total hip arthroplasty leads to worse clinical out-comes. Int Orthop 2014;38(06):1159–1165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dufour R, Joshi AV, Pasquale MK, et al. The prevalence of diagnosed opioid abuse in commercial and Medicare managed care populations. Pain Pract 2014;14(03):E106–E115 [DOI] [PubMed] [Google Scholar]
- 14.Bozic KJ, Lau E, Ong K, et al. Risk factors for early revision after primary TKA in Medicare patients. Clin Orthop Relat Res 2014; 472(01):232–237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bedard NA, DeMik DE, Dowdle SB, Callaghan JJ. Trends and risk factors for prolonged opioid use after unicompartmental knee arthroplasty. Bone Joint J 2018;100-B(1, suppl A):62–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mont MA, Beaver WB, Dysart SH, Barrington JW, Del Gaizo DJ. Local infiltration analgesia with liposomal bupivacaine improves pain scores and reduces opioid use after total knee arthroplasty: results of a randomized controlled trial. J Arthroplasty 2018;33 (01):90–96 [DOI] [PubMed] [Google Scholar]
- 17.Elmallah RK, Cherian JJ, Pierce TP, Jauregui JJ, Harwin SF, Mont MA. New and common perioperative pain management techniques in total knee arthroplasty. J Knee Surg 2016;29(02):169–178 [DOI] [PubMed] [Google Scholar]
- 18.Oliver J, Coggins C, Compton P, et al. ; American Society for Pain Management Nursing. American Society for Pain Management Nursing position statement: pain management in patients with substance use disorders. J Addict Nurs 2012; 23(03):210–222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ballantyne JC. Opioids for the treatment of chronic pain: mistakes made, lessons learned, and future directions. Anesth Analg 2017; 125(05):1769–1778 [DOI] [PubMed] [Google Scholar]
- 20.Prater CD, Zylstra RG, Miller KE. Successful pain management for the recovering addicted patient. Prim Care Companion J Clin Psychiatry 2002;4(04):125–131 [DOI] [PMC free article] [PubMed] [Google Scholar]


