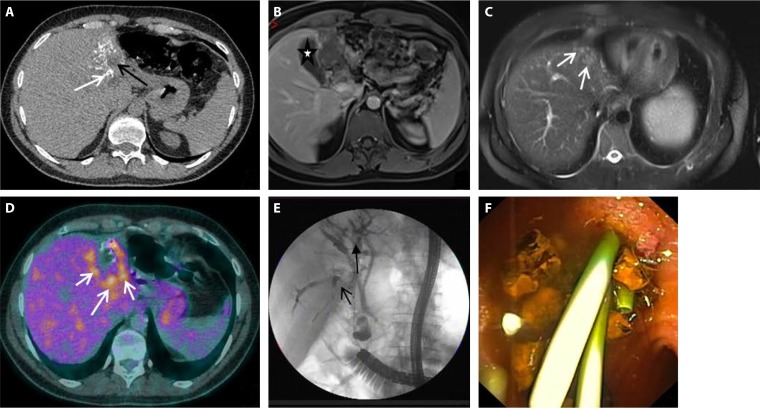
FIG 6.
Complementarity of imaging techniques for the diagnosis and preoperative assessment of alveolar echinococcosis (AE) lesions in a patient with portal vein and bile duct invasion by the parasitic lesions. (A) On computed tomography (CT) scanning, the lesion shows the characteristic heterogeneous aspect of AE, with hyperdense calcifications (white arrow) and hypodense area (central necrosis) (black arrow). (B) Fat-suppressed T1-weighted magnetic resonance (MR) image after gadolinium injection at the portal venous phase shows an atrophy of the left liver and invasion of the left portal vein and of the left intrahepatic biliary tree. The lesion is at the contact of the gallbladder (white star) which is not invaded. (C) T2-weighted MR images show the presence of hyperintense microcysts (white arrows), pathognomonic of AE, but also a solid component (Kodama type II). (D) Fluorodeoxyglucose (FDG) uptake in positron emission tomography (PET) is markedly increased at the periphery of the lesion (white arrows). (E) Assessment of biliary tree involvement and treatment by perendoscopic stenting in a patient with late postoperative biliary complications of AE. Endoscopic retrograde cholangiopancreatography (ERCP) was performed (with a colonoscope because of previous gastrectomy), showing dilation of the extrahepatic and intrahepatic biliary tree with several defects (black arrows) because of biliary stones due to chronic biliary obstruction and bacterial superinfection. (F) Perendoscopic stenting via ERCP. After balloon dilation followed by extensive lavage with isotonic saline and stone extraction, 3 plastic stents (size, 7 and 10 French) are inserted in the stenosis of the bile duct (endoscopic view).