Abstract
Background Vascularized bone grafts have become one of the first treatment options for scaphoid nonunions and Kienböck's disease. The aim of this study is to review the current body of the literature regarding the use of four vascularized bone grafts (1,2 ICSRA [1,2 intercompartmental supraretinacular artery] graft, 4+5 ECA [4+5 extracompartmental artery] graft, volar radial graft, and free medial femoral condyle graft) in these pathologies.
Patients and Methods A search on MEDLINE and Google Scholar was performed. Exclusion criteria included language other than English, studies with no full text available, case reports, letters, editorials, and review articles. The primary outcomes included consolidation rate of the grafts and time to union regarding scaphoid nonunion, as well as the clinical outcomes (pain, grip strength, range of motion), revascularization of the lunate, and progression of the disease regarding Kienböck's disease.
Results A total of 37 articles were included in the study enrolling 917 patients. Regarding scaphoid nonunion, the consolidation rate was 86.3% for the 1,2 ICSRA graft, 93.9% for the volar radial bone graft, and 88.8% for the free medial femoral condyle graft. In patients with Kienböck's disease, progression of the disease was observed in 13% of patients, and grip strength and pain were substantially improved whereas range of motion did not demonstrate statistically significant improvement ( p < 0.05).
Conclusion Vascularized bone grafts yield successful outcomes in patients with scaphoid nonunions demonstrating a high union rate. In patients with Kienböck's disease, vascularized grafts lead to revascularization of the lunate in most of the cases with concomitant improvement of the clinical parameters.
Keywords: vascularized bone grafts; 1,2 intercompartmental supraretinacular artery graft; 4+5 extracompartmental artery graft; volar distal radius graft; medial condyle-free graft
Introduction
Vascularized bone grafts were used for the first time 100 years ago when Huntington in the early 1900s used a fibular graft along with its nutritional artery to restore a tibial bone defect. Preservation of the blood supply of the grafts allows primary bone healing; thus, they are consolidated much faster and are more robust compared with nonvascularized grafts. Vascularized bone grafts are either local pedicled grafts attached to their native vasculature or free grafts raised on a particular arteriovenous pedicle, divided and reanastomosed to a vessel at the recipient area. Disadvantages of free grafts include donor area morbidity, need for microsurgical anastomosis, and longer duration of the operation. These problems may be overcome with the use of pedicled local vascularized grafts.
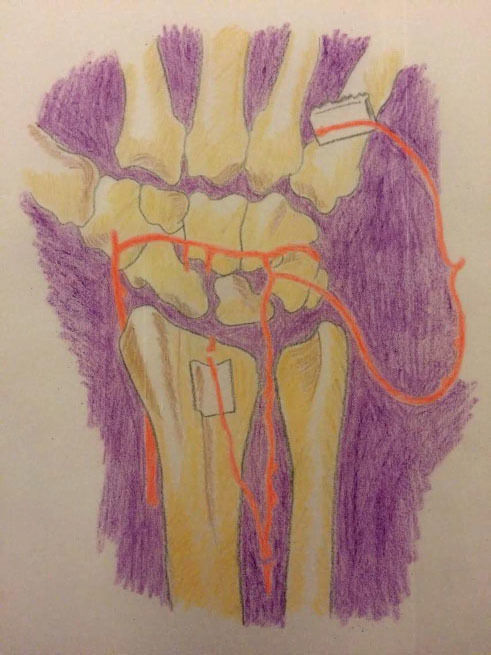
During the past 25 years, vascularized bone grafts have been widely used for the treatment of many carpal pathologies. 1 Literature has shown excellent results regarding the use of these grafts in cases of scaphoid nonunions (with or without proximal pole necrosis) and idiopathic osteonecrosis of lunate (Kienböck's disease). Subsequently they have become one of the first treatment options for these two disorders. The knowledge of the detailed vascular anatomy and of the most commonly used arterial pedicles is necessary ( Fig. 1 ).
Fig. 1.
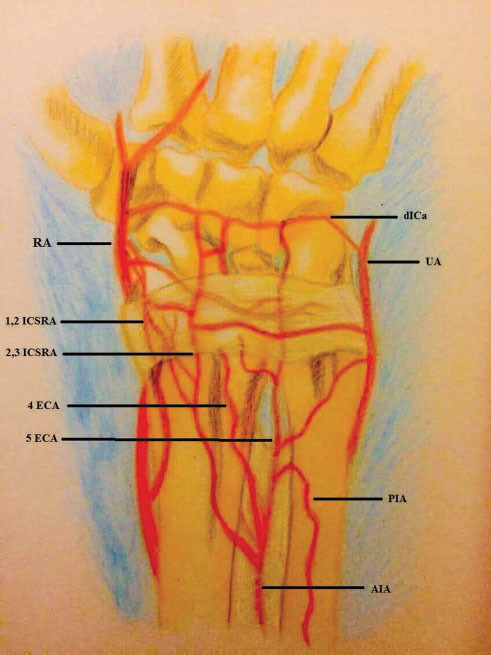
Dorsal vasculature of the carpal area. The four compartmental arteries are demonstrated. 1,2 ICSRA, 1,2 intercompartmental supraret-inacular artery; 2,3 ICSRA, 2,3 intercompartmental supraretinacular artery; 4 ECA, 4 extracompartmental artery; 5 ECA, 5 extracompartmental artery; AIA, anterior interosseous artery; DICA, dorsal inter-carpal artery; PIA, posterior interosseous artery; RA, radial artery; UA, ulnar artery.
The incidence of scaphoid nonunion when conservative treatment is followed is 5 to 10%. 2 3 4 A critical point regarding the treatment of scaphoid nonunion is whether necrosis of the proximal pole has occurred or not. When the blood supply to the proximal pole has not been disrupted, the recommended treatment option is application of conventional (nonvascularized) bone grafts. Russe et al suggested volar approach and application of a rectangular bone graft, whereas when humpback deformity has been developed wedge bone grafts should be used to restore the native shape of the scaphoid. In cases of nonunions at the proximal pole as well as of nonunions at the waist with proximal pole necrosis vascularized bone grafts are now considered the gold standard. 5 In a recent meta-analysis, the union rate of these grafts in scaphoid nonunions is 84%. 6
In patients with Kienböck's disease, vascularized bone grafts have been used for stages up to IIIa with satisfactory results. A necessary prerequisite for the use of vascularized bone grafts in these patients is the intact cartilaginous shell of the lunate and absence of arthritic changes. 7
There is a wide variety of vascularized bone grafts for the treatment of the two mentioned pathologies ( Table 1 ). Most of these grafts are local pedicled grafts without the need for vascular anastomosis, but free bone grafts from the medial femoral condyle or iliac crest are also used 8 :
Table 1. The most commonly used vascularized bone grafts for the treatment of carpal conditions.
| Carpal pathology | Vascularized bone grafts |
|---|---|
| Abbreviations: 1,2 ICSRA, 1,2 intercompartmental supraretinacular artery; 2,3 ICSRA, 2,3 intercompartmental supraretinacular artery; 4+5 ECA, 4+5 extracompartmental artery. | |
| Scaphoid nonunions | 1) 1,2 ICISRA bone graft 2) Volar bone graft from the distal radius 3) Free bone grafts from the medial femoral condyle or the iliac crest |
| Kienböck's disease | 1) 4+5 ECA bone graft 2) 2,3 ICSRA ή 1,2 ICSRA bone graft 3) 2nd or 3rd metacarpal base bone graft 4) Pisiform bone graft 5) Volar bone grafts from the distal radius 6) Free bone grafts from the medial femoral condyle or iliac crest |
The most commonly used vascularized bone grafts for the treatment of scaphoid nonunions include (1) 1,2 intracompartmental supraretinacular artery (ICSRA) bone grafts, (2) volar bone grafts from the distal radius, and (3) free pedicle bone grafts from the medial femoral condyle or the iliac crest. 9
The main vascularized bone grafts for the treatment of Kienböck's disease include (1) 4+5 extensor compartment artery (ECA) bone graft, (2) second or third metacarpal base bone grafts, (3) 2,3 ICSRA ή 1,2 ICSRA bone grafts, (4) pisiform bone graft, (5) volar bone grafts from the distal radius, and (6) free pedicle bone grafts from the medial femoral condyle. 10 11 12 13 14
The aim of this study is to examine the current body of the literature regarding the use of four vascularized bone grafts (1,2 ICSRA graft, 4+5 ECA graft, volar radial graft, and free medial femoral condyle graft) for the treatment of Kienböck's disease and scaphoid nonunion and assess certain properties and the results of these grafts in patients with these disorders.
Patients and Methods
A search on MEDLINE and Google Scholar for human studies published between 1987 and 2018 was performed using the following search strategy: the following keywords or Mesh-terms were combined with “OR” then by “AND”: “carpal vascularized bone grafts,” “carpal vascularized bone grafts,” “1,2 ICSRA graft,” “4+5 ECA bone graft,” “radial volar bone graft,” and “medial femoral condyle graft.” The references of selected full text articles were also pursued for the inclusion of further articles. A set of inclusion and exclusion criteria methodology was formed.
Articles concerning the management of the two carpal pathologies (scaphoid nonunion, Kienböck's disease) using the four vascularized bone grafts were included. Exclusion criteria included language other than English, studies with no full text available, studies without a clear mention about the postoperative results of the grafts regarding the incorporation rate or the type of the graft, as well as case reports, letters, editorials, and review articles. Abstracts were screened for relevance. Group and study characteristics that were recorded from each study included number of patients, mean age, and sex. The studied outcomes that were extracted from each article and compiled into a database included consolidation rate of the grafts and time to union regarding scaphoid nonunion, as well as the clinical outcomes (pain, grip strength, range of motion [ROM]), the revascularization rate of the lunate and the progression of the disease with regards to Kienböck's disease.
Recorded data were extracted and entered into an excel spreadsheet (Microsoft Office Excel, 2007). Statistical analysis was performed including descriptive statistics, and differences between the groups were calculated using chi-square test for categorical variables (consolidation of the grafts in scaphoid nonunion) and Student's t -test for quantitative variables (pain, grip strength, and ROM of patients with Kienböck's disease). Relative risks (RR) were also calculated. A p ≤ 0.05 was considered to be statistically significant.
Results
Results from the initial electronic search yielded 279 potentially relevant citations. Of these citations, 145 articles were excluded after going through their title and abstract. Total 37 articles met the inclusion criteria and were included in the study ( Fig. 2 ). Nineteen studies about the use of 1,2 ICSRA graft for scaphoid nonunion, 5 studies about the use of 4+5 ECA graft for Kienböck's disease and scaphoid nonunion, 5 about the use of volar distal radial graft for Kienböck's disease and scaphoid nonunion, and 8 about the use of free medial condyle vascularized grafts for Kienböck's disease and scaphoid nonunion met inclusion criteria. Total 917 patients were included in the studies, 825 with scaphoid nonunion and 92 with Kienböck disease.
Fig. 2.
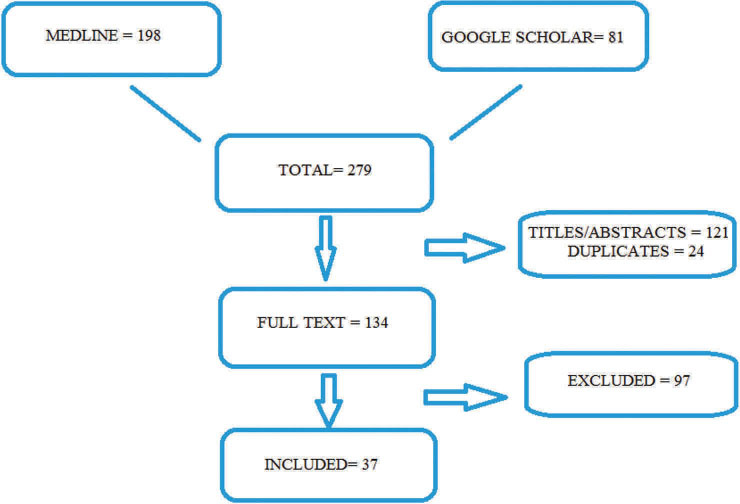
Flowchart displaying the review process.
1,2 Intracompartmental Supraretinacular Artery Bone Graft
This bone graft, first described by Zaidemberg in 1991, is based on a branch of the radial artery located between the first and second extensor tendon compartment ( Fig. 3 ). 15 This branch called 1,2 ICSRA lies on the extensor retinaculum on the dorsal surface of the distal radius and has a distal and proximal anastomosis with the radial artery ( Fig. 1 ). Subsequently the blood supply for this bone graft comes from the distal anastomosis in a retrograde fashion.
Fig. 3.
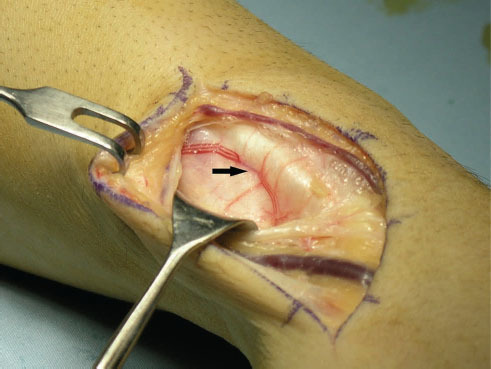
Intraoperative image showing the position of 1,2 ICSRA (black arrow).
Debridement and preparation of the recipient area must be performed first to create a rectangular space into which the graft will be embedded. It must be noted that during harvest of the graft, the distal cut on the radial surface of the radius must be 8 to 15 mm proximal to the radiocarpal joint to include as many perforator branches of the 1,2 ICSRA pedicle, because it has been shown from anatomical studies that these perforators begin at approximately 12 mm proximal to the joint and are approximately 5 in total 9 ( Fig. 4 ). The vascular pedicle along with a surrounding tissue cuff is dissected up to its distal origin from the radial artery and is raised along with the bone graft. The bone graft is placed into the recipient space and is fixed with K-wires or with a screw. 16 17 In cases of humpback deformity, the graft can be placed on the volar side of the scaphoid to restore its native geometry. 18
Fig. 4.
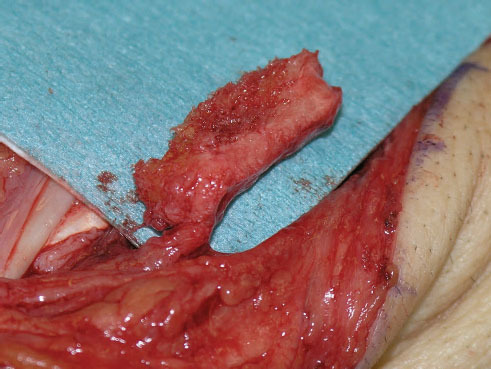
Intraoperative image showing the harvested 1,2 ICSRA bone graft along with its pedicle.
The 1,2 ICSRA bone graft is the most studied vascularized bone graft for the treatment of carpal pathologies. Nineteen articles approximately 1,2 ICSRA for scaphoid nonunion met inclusion criteria and were included in the study. 15 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 In total there were 541 patients with scaphoid nonunion. Avascular necrosis was evident in 242 of them. Consolidation of the graft and union of scaphoid were observed in 467 (86.3%) patients. In patients with avascular necrosis, this rate was 77.9%, whereas when avascular necrosis was not evident, the union rate was 96.2%. This difference was statistically significant ( p < 0.05, RR = 1.23). The mean time to union in all patients was 9.7 weeks after the index operation. However, the results in the literature regarding the consolidation rates of the graft are highly varying. There are certain studies with numerous patients such as that of Waitayawinyu et al in which out of 30 patients with scaphoid nonunion (and additionally proximal pole necrosis), consolidation of the graft occurred in 28 of them. 20 Korompilias et al studied 23 patients with scaphoid nonunion associated with humpback deformity and demonstrated excellent results with a union rate of 100% along with additional correction of the deformity. 26 On the other hand, there are studies in which these rates are much lower. Straw et al in their study reported a union rate of 27%, Chang et al reported a consolidation rate of 70%, whereas this rate was 60% in the study by Boyer's et al. 27 28 29 These authors concluded that possible risk factors for failure were female sex, smoking, previous surgical treatment for scaphoid nonunion, proximal pole necrosis, and humpback deformity.
4+5 Extracompartmental Artery Bone Graft
4+5 ECA bone graft is mainly used for the treatment of Kienböck's disease. It has three favorable properties: the diameter of the vascular pedicle is wide, the pedicle is long, and the bone graft is on the ulnar side of the radius. 11 36 In the past, this bone graft has been used with a pedicle consisted of just the 4 ECA, but nowadays the pedicle consists of both the 4 ECA and 5 ECA (4+5 ECA bone graft) to increase its length ( Fig. 5 ). These arteries are located into the radial part of fourth and fifth extensor tendons compartments respectively and are connected proximally with the dorsal branch of the anterior interosseous artery and distally with the dorsal intercarpal arch. Subsequently the blood supply of this graft comes in a retrograde fashion from the dorsal intercarpal arch through the 4 ECA and 5 ECA, respectively.
Fig. 5.
An illustration depicting the pedicle of the 4+5 ECA bone graft that consists of both the 4 ECA and 5 ECA.
Four articles approximately 4+5 ECA for Kienböck's disease (stages II, III) and one article for scaphoid nonunion met inclusion criteria and were included in the study. 5 36 37 38 In total there were 54 patients with Kienböck's disease. The mean follow-up in these studies was 45 months (20–70 months). Progression of the disease based on the Lichtman classification was evident in 8 (15%) patients, but the duration of the follow-up period was highly varying in these studies; thus, safe conclusions about the progression of the disease cannot be made. Grip strength was improved from 54% of the normal hand before surgery to 88% after surgery ( p < 0.05). Regarding ROM, an improvement from 66% of normal before surgery to 77% after surgery was shown ( p < 0.05). Although most studies showed significant improvement regarding ROM, this was not evident in the largest study enrolling 26 patients. Pain as assessed by visual analog scale (VAS) score was improved from 6,5 preoperatively to 2,2 postoperatively ( p < 0.05). Revascularization of the graft assessed by conventional X-rays or magnetic resonance imaging (MRI) for showed that revascularization occurred in 71% of the cases. The use of 4+5 ECA graft has also been studied in patients with scaphoid nonunions. In a recent study, the use of this graft resulted in consolidation of the graft in eight out of nine cases with scaphoid nonunion, with an average time to union 9.9 weeks. 25
Volar Bone Grafts from the Distal Radius
Volar bone grafts from the distal radius were first described by Kulhmann et al in 1987. 39 These grafts are based on the volar carpal artery that connects the radial and ulnar artery and is located on the palmar periosteum of the distal radius distally to the edge of the superficial fascia of the pronator quadratus. They can be used for the treatment of both scaphoid nonunions (especially in cases of humpback deformities) and Kienböck's disease. These bone grafts can be used as trapezoid or wedge grafts. The application of a wedge graft in the volar side of the scaphoid is very helpful for the correction of the native scaphoid shape in cases of humpback deformity. The harvest of these grafts is similar to that of the other local radial grafts and can be stabilized in the recipient area with the aid of K-wires or a screw. Literature has shown successful results regarding the use of these volar grafts for scaphoid nonunions and Kienböck's disease. Four articles regarding the use of volar radial bone grafts for scaphoid nonunion and one study for Kienböck's disease met inclusion criteria and were included in the study. 14 39 40 42 In total there were 132 patients with scaphoid nonunion. A clear mention regarding the presence or not of avascular necrosis was given only in two studies. Avascular necrosis was evident in 67 out of 86 cases. Consolidation of the graft and union was achieved in 124 patients (93.9%) patients. The union rate was significantly higher ( p < 0.05) in patients without avascular necrosis (94.7%) compared with those with necrosis (85%) (RR = 1.11). The mean time to union in all patients was 10.1 weeks. Dailiana et al demonstrated union in all nine cases of scaphoid nonunions, though it must be noted that there were not any cases of proximal pole necrosis in this study. 40 In another study with a large number of patients (111 patients with scaphoid nonunions), the union rate for the volar bone grafts was 96% when no other surgery was previously performed, and 89% when another surgery for the treatment of nonunions preceded. 41 Regarding Kienböck's disease, the use of these grafts has been studied in 22 patients with stages II and III disease. The mean duration of postoperative follow-up was up to 6 years. MRI results showed revascularization in 17 patients, whereas there was progression of the disease in two patients. Eighteen patients were completely pain free. Pain remained unchanged in two cases. The ROM and strength increased significantly in all cases ( p < 0.05). 14
Medial Femoral Condyle Free Grafts
The free vascularized bone grafts can be harvested from either the iliac crest or the medial femoral condyle. 43 44 45 46 47 48 During the past years, there is a growing interest for the medial femoral condyle grafts due to their excellent results regarding their consolidation rates and their potential to be shaped in any configuration, thus correcting any humpback deformity in cases of scaphoid nonunions. Another noteworthy characteristic of these grafts is that they can contain a cartilaginous part and subsequently replace the proximal articular part of either the scaphoid or lunate ( Fig. 6 ). This is very helpful in cases of very proximal scaphoid nonunions or in cases where the cartilage of the articular proximal part of the lunate has been breached. In cases of very proximal scaphoid nonunions, the size of the proximal fragment may be too small and this makes the correct interposition and fixation of the local vascularized graft between the proximal and distal fragments technically demanding, and in many cases not feasible. Also, in cases of Kienböck's disease in which the cartilage of the proximal articular part of the lunate is damaged, the osteochondral free grafts are ideal as they can replace the proximal articular surface of the lunate.
Fig. 6.
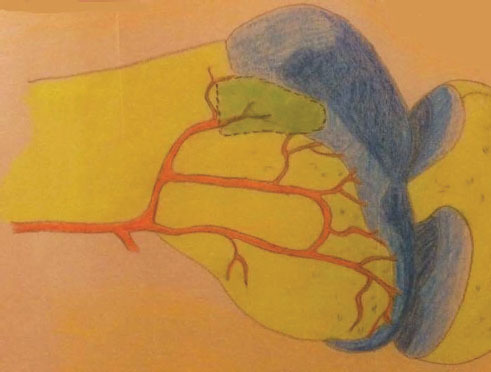
An illustration demonstrating the medial femoral condyle graft (dotted line) that can be harvested as osteoarticular graft containing part of the articular surface of the medial femoral condyle.
The interest for these grafts led to the conduction of many anatomical studies regarding the vascular anatomy of the medial femoral condyle area. 49 50 These grafts are based on one of two possible arteries at the medial femoral condyle area: the articular branch of the descending genicular artery that originates from the superficial femoral artery or the superior medial genicular artery that originates from the popliteal artery. In most cases, the articular branch of the descending genicular artery is used as it is longer and has a larger diameter compared with the superior medial genicular artery. As mentioned, these grafts can be either cortical-cancellous or osteochondral along with a part of the articular cartilage. 51 52 53
There are many recent studies regarding the use of the medial femoral condyle-free grafts for the treatment of scaphoid nonunion and Kienböck's disease. Seven articles regarding these grafts for scaphoid nonunion met inclusion criteria and were included in the study. In total there were 143 patients with scaphoid nonunion. 44 51 54 55 56 57 58 In the cases included in these studies, the nonunion was too proximal to the bone so that an intercalary bone graft between the proximal and distal bone fragments could not be placed in most cases. Avascular necrosis was evident in 130 of them. Consolidation of the graft and union was achieved in 127 (88.8%) patients. In patients with avascular necrosis, this rate was 86.9%, whereas when avascular necrosis was not evident, the union rate was 92.3%. This difference was not statistically significant ( p < 0.05). The mean time to union was 12 weeks. The first published study regarding the use of a free cortical-cancellous bone graft from the medial femoral condyle was in 2000 by Doi et al who showed excellent union rates in all 10 cases of scaphoid nonunions. 44 Jones et al in a comparative study with patients with scaphoid nonunions with additional proximal pole necrosis showed that these free vascularized bone grafts had superior results regarding consolidation rate compared with the 1,2 ICSRA bone grafts. 59 In another comparative study between the medial femoral grafts and 1,2 ICSRA bone grafts for the treatment of scaphoid nonunions, the results were also superior for the free grafts with 79% union rate for the 1,2 ICSRA bone grafts and 89% for the medial femoral grafts. 55 The results of the osteochondral grafts from the medial femoral condyle have also been published. Bürger et al have published two studies regarding the use of these grafts in patients with proximal pole scaphoid nonunions and with Kienböck's disease. 51 52 The results of these studies were excellent, achieving consolidation of the grafts in 15 out of 16 cases. Regarding the study in which medial femoral condyle used in patients with Kienböck's disease, in 10 out of 16 patients, the stage of the disease remained the same after 19 months, whereas there was improvement in 4 patients and progression of the disease in 2 patients. Revascularization of the graft was evident in 15 patients. Grip strength was substantially improved and reached 86% of the normal hand after surgery. Pain was significantly improved whereas the postoperative ROMs did not significantly change ( p < 0.05). 52
Discussion
The two main indications for the vascularized bone grafts in carpal pathologies are scaphoid nonunions and Kienböck's disease. These grafts are now considered the gold standard for the treatment of scaphoid nonunions, especially in cases with proximal pole necrosis. According to the study results, the consolidation rate was 86.3% for the 1,2 ICSRA graft, 93.9% for the volar radial bone graft, and 88.8% for the free medial femoral condyle graft ( Table 2 ). There was no statistical significant difference between the 1,2 ICSRA and medial femoral condyle graft as well as between the medial femoral condyle and the radial volar graft ( p < 0.05). On the other hand, there was statistical significant difference between the consolidation rate of the 1,2 ICSRA and the radial volar graft ( p < 0.05). Proximal pole necrosis is a critical point concerning the healing of these nonunions, which was also shown in this study. Pooling all patients from all studies regardless of the type of the graft showed that the union rate in cases with avascular necrosis was 81.4% whereas this was 96.4% in cases without necrosis. The difference between the two groups is statistically significant ( p < 0.05, RR = 1.18). In cases in which the 1,2 ICSRA or volar radial graft were used, there was a significant decrease in the union rates when proximal pole necrosis was present, although this was not evident in cases in which medial condyle-free grafts were used. Another significant factor regarding the treatment of scaphoid nonunions is whether humpback deformity has been developed. For the restoration of the scaphoid geometry, either volar bone grafts from the distal radius or free vascularized bone grafts are preferred.
Table 2. Union rates of scaphoid nonunions with the vascularized bone grafts.
| 1,2 ICSRA | Volar radial graft | Medial femoral condyle graft | |
|---|---|---|---|
| Abbreviation: 1,2 ICSRA, 1,2 intercompartmental supraretinacular artery. a There was statistical significant difference between the 1,2 ICSRA and radial volar graft (chi-square = 5.7549, p < 0.05). | |||
| Union | 467 | 124 | 127 |
| Nonunion | 74 | 8 | 16 |
| Total | 541 | 132 | 143 |
| % Union | 86.3 a | 93.9 a | 88.8 |
In patients with Kienböck's disease up to stage IIIA, the results of the vascularized bone grafts regarding the clinical outcomes and the cease of the progression of the disease are satisfactory ( Table 3 ). In total, progression of the disease based on the Lichtman classification was evident in 13% of the cases after the application of these grafts, but the duration of the follow-up period in the included studies was highly varying, so we cannot conclude whether cessation of the disease can be achieved in long term. Grip strength was improved from 52% of the normal hand before surgery to 84% after surgery ( p < 0.05). Regarding ROM, an improvement from 66% of normal before surgery to 77% after surgery was shown ( p < 0.05). Pain as assessed by VAS score was improved from 6,5 preoperatively to 2,2 postoperatively ( p < 0.05). Revascularization of the graft assessed by conventional X-rays or MRI showed that revascularization occurred in 83% of the cases.
Table 3. Results of vascularized bone grafts in Kienböck's disease.
| 4+5 ECA | Volar radial graft | Medial femoral condyle graft | |
|---|---|---|---|
| Abbreviation: 4+5 ECA, 4+5 extracompartmental artery. | |||
| Disease progression (% of cases) | 15 | 9 | 12,5 |
| Revascularization of lunate (% of cases) | 71 | 77 | 93,7 |
| Total cases | 54 | 22 | 16 |
Conclusively, the 1,2 ICSRA bone graft has shown excellent outcomes regarding the consolidation rate in scaphoid nonunions even though many studies were not consistent with these successful results. The 4+5 ECA bone graft is mainly used for the treatment of Kienböck's disease and has three main advantages: its pedicle has a wide diameter and a high length, and additionally the bone graft is harvested from the ulnar side of the radius; thus, it is closer to the lunate. The volar radial bone graft consists of an ideal option in scaphoid nonunions along with humpback deformity. The free vascularized bone grafts from the medial femoral condyle are gaining ground. In recent studies, these grafts have been harvested as osteoarticular grafts containing a part of the articular surface of the medial femoral condyle. This is of great significance as it makes it possible to completely replace the proximal articular part of the scaphoid or lunate. This is a great advantage in difficult cases in which the nonunion is located at the very proximal part of the scaphoid, or the cartilage of the proximal articular part of the lunate is damaged. On the other hand, a vascular anastomosis must be performed during the procedure; thus, the use of free vascularized bone grafts is technically more demanding and time consuming.
Funding Statement
Funding None.
Footnotes
Conflict of Interest None declared.
References
- 1.Steinmann S P, Bishop A T. A vascularized bone graft for repair of scaphoid nonunion. Hand Clin. 2001;17(04):647–653. [PubMed] [Google Scholar]
- 2.Ford D J, Khoury G, el-Hadidi S, Lunn P G, Burke F D. The Herbert screw for fractures of the scaphoid. A review of results and technical difficulties. J Bone Joint Surg Br. 1987;69(01):124–127. doi: 10.1302/0301-620X.69B1.3818717. [DOI] [PubMed] [Google Scholar]
- 3.Lindström G, Nyström A. Natural history of scaphoid nonunion, with special reference to “asymptomatic” cases. J Hand Surg [Br] 1992;17(06):697–700. doi: 10.1016/0266-7681(92)90204-f. [DOI] [PubMed] [Google Scholar]
- 4.Rajagopalan B M, Squire D S, Samuels L O. Results of Herbert-screw fixation with bone-grafting for the treatment of nonunion of the scaphoid. J Bone Joint Surg Am. 1999;81(01):48–52. doi: 10.2106/00004623-199901000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Miller M D, Thompson S, Hart J. Philadelphia, PA: Elsevier; 2012. Review of Orthopaedics. [Google Scholar]
- 6.Alluri R K, Yin C, Iorio M L, Leland H, Mack W J, Patel K. A critical appraisal of vascularized bone grafting for scaphoid non union. J Wrist Surg. 2017;6(03):251–257. doi: 10.1055/s-0036-1597575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rizzo M, Moran S L. Vascularized bone grafts and their applications in the treatment of carpal pathology. Semin Plast Surg. 2008;22(03):213–227. doi: 10.1055/s-2008-1081404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trumble T. Philadelphia, PA: Mosby; 2006. Core Knowledge in Orthopaedics: Hand, Elbow, and Shoulder. [Google Scholar]
- 9.Jones D B, Jr, Rhee P C, Shin A Y. Vascularized bone grafts for scaphoid nonunions. J Hand Surg Am. 2012;37(05):1090–1094. doi: 10.1016/j.jhsa.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Lutsky K, Beredjiklian P K. Kienböck disease. J Hand Surg Am. 2012;37(09):1942–1952. doi: 10.1016/j.jhsa.2012.06.029. [DOI] [PubMed] [Google Scholar]
- 11.Elhassan B T, Shin A Y. Vascularized bone grafting for treatment of Kienböck's disease. J Hand Surg Am. 2009;34(01):146–154. doi: 10.1016/j.jhsa.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 12.Simmons S P, Tobias B, Lichtman D M. Lunate revascularization with artery implantation and bone grafting. J Hand Surg Am. 2009;34(01):155–160. doi: 10.1016/j.jhsa.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 13.Fujiwara H, Oda R, Morisaki S, Ikoma K, Kubo T. Long-term results of vascularized bone graft for stage III Kienböck disease. J Hand Surg Am. 2013;38(05):904–908. doi: 10.1016/j.jhsa.2013.02.010. [DOI] [PubMed] [Google Scholar]
- 14.Mathoulin C, Wahegaonkar A L. Revascularization of the lunate by a volar vascularized bone graft and an osteotomy of the radius in treatment of the Kienböck's disease. Microsurgery. 2009;29(05):373–378. doi: 10.1002/micr.20657. [DOI] [PubMed] [Google Scholar]
- 15.Zaidemberg C, Siebert J W, Angrigiani C. A new vascularized bone graft for scaphoid nonunion. J Hand Surg Am. 1991;16(03):474–478. doi: 10.1016/0363-5023(91)90017-6. [DOI] [PubMed] [Google Scholar]
- 16.Pacelli L, Pederson W. Vascularized bone grafting for scaphoid nonunions. J Hand Surg Am. 2003;13(01):21–26. [Google Scholar]
- 17.Gray R, Shin A. Vascularized bone grafting of scaphoid non-unions. Arthrosc Tech. 2010;18(03):155–162. [Google Scholar]
- 18.Henry M. Collapsed scaphoid non-union with dorsal intercalated segment instability and avascular necrosis treated by vascularised wedge-shaped bone graft and fixation. J Hand Surg Eur Vol. 2007;32(02):148–154. doi: 10.1016/J.JHSB.2006.11.018. [DOI] [PubMed] [Google Scholar]
- 19.Dehghani M, Soltanmohamadi M, Tahririan M A, Moezi M, Daneshpajouhnejad P, Zarezadeh A. Management of scaphoid nonunion with avascular necrosis using 1,2 intercompartmental supraretinacular arterial bone graft. Adv Biomed Res. 2014;3(01):185. doi: 10.4103/2277-9175.140094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Waitayawinyu T, McCallister W V, Katolik L I, Schlenker J D, Trumble T E. Outcome after vascularized bone grafting of scaphoid nonunions with avascular necrosis. J Hand Surg Am. 2009;34(03):387–394. doi: 10.1016/j.jhsa.2008.11.023. [DOI] [PubMed] [Google Scholar]
- 21.Hirche C, Heffinger C, Xiong L et al. The 1,2-intercompartmental supraretinacular artery vascularized bone graft for scaphoid nonunion: management and clinical outcome. J Hand Surg Am. 2014;39(03):423–429. doi: 10.1016/j.jhsa.2013.10.028. [DOI] [PubMed] [Google Scholar]
- 22.Malizos K N, Dailiana Z H, Kirou M, Vragalas V, Xenakis T A, Soucacos P N. Longstanding nonunions of scaphoid fractures with bone loss: successful reconstruction with vascularized bone grafts. J Hand Surg [Br] 2001;26(04):330–334. doi: 10.1054/jhsb.2001.0570. [DOI] [PubMed] [Google Scholar]
- 23.Liang K, Ke Z, Chen L, Nie M, Cheng Y, Deng Z. Scaphoid nonunion reconstructed with vascularized bone-grafting pedicled on 1,2 intercompartmental supraretinacular artery and external fixation. Eur Rev Med Pharmacol Sci. 2013;17(11):1447–1454. [PubMed] [Google Scholar]
- 24.Ribak S, Medina C E, Mattar R, Jr, Ulson H J, Ulson H J, Etchebehere M. Treatment of scaphoid nonunion with vascularised and nonvascularised dorsal bone grafting from the distal radius. Int Orthop. 2010;34(05):683–688. doi: 10.1007/s00264-009-0862-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Özalp T, Öz Ç, Kale G, Erkan S. Scaphoid nonunion treated with vascularised bone graft from dorsal radius. Injury. 2015;46 02:S47–S52. doi: 10.1016/j.injury.2015.05.032. [DOI] [PubMed] [Google Scholar]
- 26.Korompilias A V, Lykissas M G, Kostas-Agnantis I P, Gkiatas I, Beris A E. An alternative graft fixation technique for scaphoid nonunions treated with vascular bone grafting. J Hand Surg Am. 2014;39(07):1308–1312. doi: 10.1016/j.jhsa.2014.04.021. [DOI] [PubMed] [Google Scholar]
- 27.Boyer M I, von Schroeder H P, Axelrod T S. Scaphoid nonunion with avascular necrosis of the proximal pole. Treatment with a vascularized bone graft from the dorsum of the distal radius. J Hand Surg [Br] 1998;23(05):686–690. doi: 10.1016/s0266-7681(98)80029-6. [DOI] [PubMed] [Google Scholar]
- 28.Straw R G, Davis T R, Dias J J. Scaphoid nonunion: treatment with a pedicled vascularized bone graft based on the 1,2 inter-compartmental supraretinacular branch of the radial artery. J Hand Surg [Br] 2002;27(05):413. doi: 10.1054/jhsb.2002.0808. [DOI] [PubMed] [Google Scholar]
- 29.Chang M A, Bishop A T, Moran S L, Shin A Y. The outcomes and complications of 1,2-intercompartmental supraretinacular artery pedicled vascularized bone grafting of scaphoid nonunions. J Hand Surg Am. 2006;31(03):387–396. doi: 10.1016/j.jhsa.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 30.Steinmann S P, Bishop A T, Berger R A. Use of the 1,2 intercompartmental supraretinacular artery as a vascularized pedicle bone graft for difficult scaphoid nonunion. J Hand Surg Am. 2002;27(03):391–401. doi: 10.1053/jhsu.2002.32077. [DOI] [PubMed] [Google Scholar]
- 31.Kapoor A K, Thompson N W, Rafiq I, Hayton M J, Stillwell J, Trail I A. Vascularised bone grafting in the management of scaphoid non-union—a review of 34 cases. J Hand Surg Eur Vol. 2008;33(05):628–631. doi: 10.1177/1753193408092038. [DOI] [PubMed] [Google Scholar]
- 32.Ong H S, Tan G, Chew W Y. Treatment of scaphoid non-union with 1,2 intercompartmental supraretinacular artery (1,2 ICSRA) vascularised graft. Singapore Med J. 2011;52(09):658–661. [PubMed] [Google Scholar]
- 33.Caporrino F A, Dos Santos JB, Penteado F T, de Moraes V Y, Belloti J C, Faloppa F. Dorsal vascularized grafting for scaphoid nonunion: a comparison of two surgical techniques. J Orthop Trauma. 2014;28(03):e44–e48. doi: 10.1097/BOT.0b013e3182a4a91a. [DOI] [PubMed] [Google Scholar]
- 34.Lim T K, Kim H K, Koh K H, Lee H I, Woo S J, Park M J. Treatment of avascular proximal pole scaphoid nonunions with vascularized distal radius bone grafting. J Hand Surg Am. 2013;38(10):1906–1912. doi: 10.1016/j.jhsa.2013.07.025. [DOI] [PubMed] [Google Scholar]
- 35.Malizos K N, Dailiana Z, Varitimidis S, Koutalos A. Management of scaphoid nonunions with vascularized bone grafts from the distal radius: mid- to long-term follow-up. Eur J Orthop Surg Traumatol. 2017;27(01):33–39. doi: 10.1007/s00590-016-1867-7. [DOI] [PubMed] [Google Scholar]
- 36.Moran S L, Cooney W P, Berger R A, Bishop A T, Shin A Y. The use of the 4 + 5 extensor compartmental vascularized bone graft for the treatment of Kienböck's disease. J Hand Surg Am. 2005;30(01):50–58. doi: 10.1016/j.jhsa.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 37.Nakagawa M, Omokawa S, Kira T, Kawamura K, Tanaka Y. Vascularized bone grafts from the dorsal wrist for the treatment of Kienböck disease. J Wrist Surg. 2016;5(02):98–104. doi: 10.1055/s-0036-1582427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Park I J, Kim H M, Lee J Y et al. Treatment of Kienböck's disease using a fourth extensor compartmental artery as a vascularized pedicle bone graft. J Plast Reconstr Aesthet Surg. 2016;69(10):1403–1410. doi: 10.1016/j.bjps.2016.07.013. [DOI] [PubMed] [Google Scholar]
- 39.Kuhlmann J N, Mimoun M, Boabighi A, Baux S. Vascularized bone graft pedicled on the volar carpal artery for non-union of the scaphoid. J Hand Surg [Br] 1987;12(02):203–210. doi: 10.1016/0266-7681_87_90014-3. [DOI] [PubMed] [Google Scholar]
- 40.Dailiana Z H, Malizos K N, Zachos V, Varitimidis S E, Hantes M, Karantanas A. Vascularized bone grafts from the palmar radius for the treatment of waist nonunions of the scaphoid. J Hand Surg Am. 2006;31(03):397–404. doi: 10.1016/j.jhsa.2005.09.021. [DOI] [PubMed] [Google Scholar]
- 41.Gras M, Mathoulin C. Vascularized bone graft pedicled on the volar carpal artery from the volar distal radius as primary procedure for scaphoid non-union. Orthop Traumatol Surg Res. 2011;97(08):800–806. doi: 10.1016/j.otsr.2011.08.008. [DOI] [PubMed] [Google Scholar]
- 42.Dodds S D, Halim A. Scaphoid plate fixation and volar carpal artery vascularized bone graft for recalcitrant scaphoid nonunions. J Hand Surg Am. 2016;41(07):e191–e198. doi: 10.1016/j.jhsa.2016.04.021. [DOI] [PubMed] [Google Scholar]
- 43.Gabl M, Reinhart C, Lutz M et al. Vascularized bone graft from the iliac crest for the treatment of nonunion of the proximal part of the scaphoid with an avascular fragment. J Bone Joint Surg Am. 1999;81(10):1414–1428. doi: 10.2106/00004623-199910000-00006. [DOI] [PubMed] [Google Scholar]
- 44.Doi K, Oda T, Soo-Heong T, Nanda V. Free vascularized bone graft for nonunion of the scaphoid. J Hand Surg Am. 2000;25(03):507–519. doi: 10.1053/jhsu.2000.5993. [DOI] [PubMed] [Google Scholar]
- 45.Jones D B, Jr, Shin A Y. Medial femoral condyle vascularized bone grafts for scaphoid nonunions. Chir Main. 2010;29 01:S93–S103. doi: 10.1016/j.main.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 46.Gabl M, Lutz M, Reinhart C et al. Stage 3 Kienböck's disease: reconstruction of the fractured lunate using a free vascularized iliac bone graft and external fixation. J Hand Surg [Br] 2002;27(04):369–373. doi: 10.1054/jhsb.2002.0766. [DOI] [PubMed] [Google Scholar]
- 47.Harpf C, Gabl M, Reinhart C et al. Small free vascularized iliac crest bone grafts in reconstruction of the scaphoid bone: a retrospective study in 60 cases. Plast Reconstr Surg. 2001;108(03):664–674. doi: 10.1097/00006534-200109010-00010. [DOI] [PubMed] [Google Scholar]
- 48.Sakai K, Doi K, Kawai S. Free vascularized thin corticoperiosteal graft. Plast Reconstr Surg. 1991;87(02):290–298. doi: 10.1097/00006534-199102000-00011. [DOI] [PubMed] [Google Scholar]
- 49.Yamamoto H, Jones D B, Jr, Moran S L, Bishop A T, Shin A Y. The arterial anatomy of the medial femoral condyle and its clinical implications. J Hand Surg Eur Vol. 2010;35(07):569–574. doi: 10.1177/1753193410364484. [DOI] [PubMed] [Google Scholar]
- 50.Hugon S, Koninckx A, Barbier O. Vascularized osteochondral graft from the medial femoral trochlea: anatomical study and clinical perspectives. Surg Radiol Anat. 2010;32(09):817–825. doi: 10.1007/s00276-010-0629-1. [DOI] [PubMed] [Google Scholar]
- 51.Bürger H K, Windhofer C, Gaggl A J, Higgins J P. Vascularized medial femoral trochlea osteocartilaginous flap reconstruction of proximal pole scaphoid nonunions. J Hand Surg Am. 2013;38(04):690–700. doi: 10.1016/j.jhsa.2013.01.036. [DOI] [PubMed] [Google Scholar]
- 52.Bürger H K, Windhofer C, Gaggl A J, Higgins J P. Vascularized medial femoral trochlea osteochondral flap reconstruction of advanced Kienböck disease. J Hand Surg Am. 2014;39(07):1313–1322. doi: 10.1016/j.jhsa.2014.03.040. [DOI] [PubMed] [Google Scholar]
- 53.Higgins J P, Bürger H K. Osteochondral flaps from the distal femur: expanding applications, harvest sites, and indications. J Reconstr Microsurg. 2014;30(07):483–490. doi: 10.1055/s-0034-1372484. [DOI] [PubMed] [Google Scholar]
- 54.Jones D B, Jr, Moran S L, Bishop A T, Shin A Y. Free-vascularized medial femoral condyle bone transfer in the treatment of scaphoid nonunions. Plast Reconstr Surg. 2010;125(04):1176–1184. doi: 10.1097/PRS.0b013e3181d1808c. [DOI] [PubMed] [Google Scholar]
- 55.Aibinder W R, Wagner E R, Bishop A T, Shin A Y. Bone grafting for scaphoid non unions: is free vascularized bone grafting superior for scaphoid nonunions? Hand (N Y) 2017;1:1.558944717736397E15. doi: 10.1177/1558944717736397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kumta S, Warrier S, Jain L, Ummal R, Menezes M, Purohit S. Medial femoral condyle vascularised corticoperiosteal graft: a suitable choice for scaphoid non-union. Indian J Plast Surg. 2017;50(02):138–147. doi: 10.4103/ijps.IJPS_62_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Choudry U H, Bakri K, Moran S L, Karacor Z, Shin A Y. The vascularized medial femoral condyle periosteal bone flap for the treatment of recalcitrant bony nonunions. Ann Plast Surg. 2008;60(02):174–180. doi: 10.1097/SAP.0b013e318056d6b5. [DOI] [PubMed] [Google Scholar]
- 58.Elgammal A, Lukas B. Vascularized medial femoral condyle graft for management of scaphoid non-union. J Hand Surg Eur Vol. 2015;40(08):848–854. doi: 10.1177/1753193414561900. [DOI] [PubMed] [Google Scholar]
- 59.Jones D B, Jr, Bürger H, Bishop A T, Shin A Y. Treatment of scaphoid waist nonunions with an avascular proximal pole and carpal collapse. A comparison of two vascularized bone grafts. J Bone Joint Surg Am. 2008;90(12):2616–2625. doi: 10.2106/JBJS.G.01503. [DOI] [PubMed] [Google Scholar]


