Figure 4.
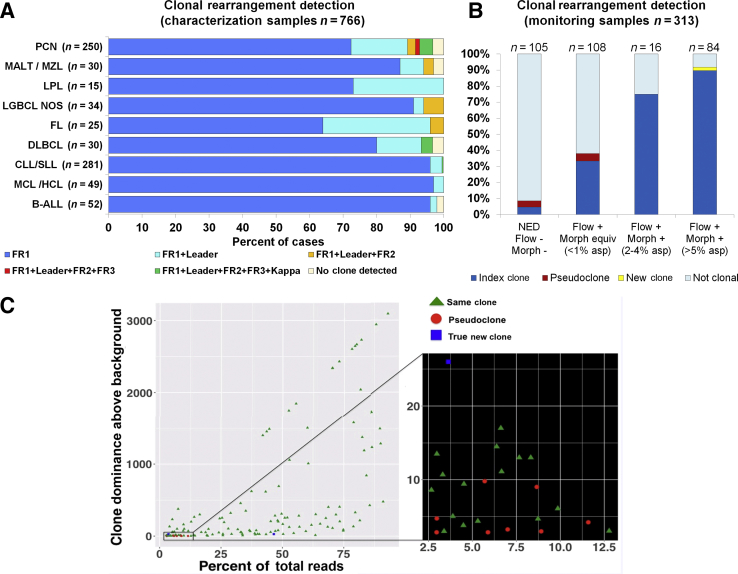
Summary of clonal characterization results in cases during the first year of assay implementation. A: Characterization cohort after implementation. Using a sequential testing approach (FR1 > leader > FR2 + FR3), overall clonality detection was 97%. Most disease categories (95%) can be successfully characterized with FR1 and leader primers only. Disease categories susceptible to somatic hypermutation show a greater number of cases requiring several primer sets for adequate characterization. With the use of κ primers (investigational), the overall detection rate would increase slightly to 98%. See details in Supplemental Table S4. B: Primary clonality assessment using monitoring samples. Samples were stratified into four categories: i) no evidence of disease (NED), ii) disease by flow only, iii) disease by flow and morphology at 2% to 4%, and iv) disease by flow and morphology at ≥5%. A clone was detected in 44% of all cases (9%, 38%, 75%, and 92% in categories 1 to 4, respectively). In 92% of the clonal cases (129/140), the detected clone was identical to the index clone of the original diagnostic sample. Ten cases had a different clone (eight deemed to represent pseudoclones and two new clones). C: The details of clones detected in the monitoring samples: scatter plot shows the relationship between the level of the detected clone (x axis, clone percentage of total reads) and its dominance above the background sequences (y axis). All sequences determined to represent a pseudoclone were detected in the context of a high polyclonal background (dominance of clone over the background, <10×), as seen in the expanded section to the right. All other clones were detected at >10×. Raising the cutoff to >10× for all samples would increase the specificity to 100% at the expense of some sensitivity (sensitivity would decline to 91% based on similar analysis using a receiver operating characteristic curve). This would affect primarily samples with tumor content <2%. n = 766 (A); n = 313 (B). asp, aspirate; B-ALL, B-cell acute lymphoblastic leukemia; CLL, chronic lymphocytic leukemia; DLBCL, diffuse large B-cell lymphoma; equiv, equivalent; FL, follicular lymphoma; HCL, hairy cell leukemia; LGBCL, low-grade B-cell lymphoma; LPL, lymphoplasmacytic lymphoma; MALT, mucosa-associated lymphoid tissue lymphoma; MCL, mantle cell lymphoma; morph, morphology; MZL, marginal zone lymphoma; NOS, not otherwise specified; PCN, plasma cell neoplasm; SLL, small lymphocytic lymphoma.