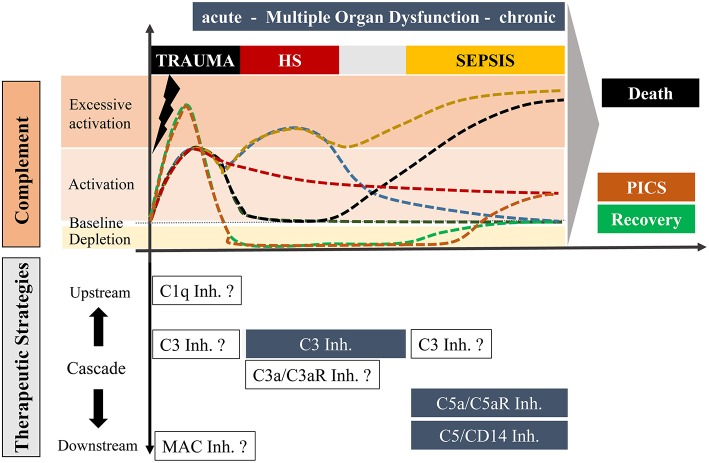
Figure 1.
Overview of potential complement responses after trauma with or without hemorrhagic shock and sepsis leading to either death or recovery or “Persistent Inflammation, Immunosuppression and Catabolism Syndrome” (PICS; with a constitutively active and chronic complement state) and potential complement-targeting strategies, respectively. The upper scaling represents the temporal course of complement activation with possible scenarios. Under optimal conditions, trauma induces an acute complement activation which follows a rapid decline to a physiological state with recovery (dark green). Alternatively, complement activity can also be maintained over a long period which may be associated with PICS (red). In an unfavorable state, the acute complement activation could be followed by secondary complication/s including sepsis leading to a complement hyperactivation and death (black). Trauma with an additional hemorrhagic shock can cause excessive complement activation, which can resolve in a physiological recovery. However, an additional hemorrhagic shock with hyperactivated complement can also result in a life-threatening sepsis phase (yellow). Trauma can further cause an acute complement hyperactivation with a rapid consumption of complement which may finally be resolved in a recovery phase (green) or to complement activation at the later stage leading to chronic inflammation (orange). The downwards orientated scaling includes possible therapeutic strategies of distinct stages of complement after trauma, hemorrhagic shock and sepsis. Blue highlighted boxes include therapeutic options which already revealed beneficial effects in pre-clinical studies. Non-highlighted boxes include possible strategies which need to be investigated in future experimental approaches.