Abstract
Peripheral ulcerative keratitis (PUK) is an aggressive, potentially sight-threatening cause for peripheral corneal thinning. It is thought to be the result of immune complex deposition at the limbus, resulting in corneal inflammation and stromal melt. We present a case of a 43-year-old female patient of African origin, presenting with PUK and associated corneal perforation as the primary presentation of HIV infection. An urgent tectonic deep anterior lamellar keratoplasty was performed under general anaesthesia with excellent outcome. The patient was referred to the sexual health clinic and anti-retroviral treatment was initiated. This case is to the best of our knowledge the first report from the UK of PUK with corneal perforation as the primary presentation of HIV infection. As highlighted in this report, infection with HIV may initially be silent; therefore, it is vital to consider HIV infection when dealing with PUK of unknown aetiology.
Keywords: ophthalmology, infectious diseases
Background
Peripheral ulcerative keratitis (PUK) is an aggressive, potentially sight-threatening cause for peripheral corneal thinning. It is thought to be the result of immune complex deposition at the limbus, resulting in corneal inflammation and stromal melt. If left untreated, it can lead to corneal perforation and loss of vision. It is therefore vital that all cases are urgently referred to an Ophthalmologist, or specifically a corneal specialist. PUK may be the presenting feature of a potentially life-threatening systemic disease. Systemic causes may be infectious or non-infectious. PUK may precede the diagnosis of the systemic condition and therefore these cases require urgent investigation. Our case highlights an interesting presentation of infection with HIV in an otherwise asymptomatic patient in apparent good health. It emphasises the importance of careful history, examination and investigation in such cases to ensure optimal, timely management, to allow for a better visual and systemic outcome.
Case presentation
A 43-year-old woman of African origin, presented with a 10-day history of soreness, redness and loss of vision in the right eye. She was in apparent good health with no known systemic conditions. She had previously been seen by her local optician and was noted to have increasing astigmatism. Visual acuity at presentation to our tertiary referral corneal unit was 2/36 in the affected right eye and 6/18 (pinhole 6/12) in the left eye. There was an area of corneal melt infero-temporally in the right eye, with iris protrusion to the wound (figure 1). Blood test investigations, including an auto-immune and infective screen, were performed to help identify a potential cause for the corneal melt. The blood results identified a reduced white cell (3.16×109/L, normal range 4–11×109/L) and neutrophil (1.42×109/L, normal range 1.5–8×109/L) count, with positive IgG antibodies to HIV type 1, suggesting infection with HIV. Unusually, the inferior corneal perforation was the primary presenting feature of her infection. An urgent tectonic deep anterior lamellar keratoplasty (corneal graft surgery where the host Descemet’s membrane and endothelium are maintained, and donor epithelium, basement membrane and stroma are transplanted) was performed the following morning under general anaesthesia.
Figure 1.
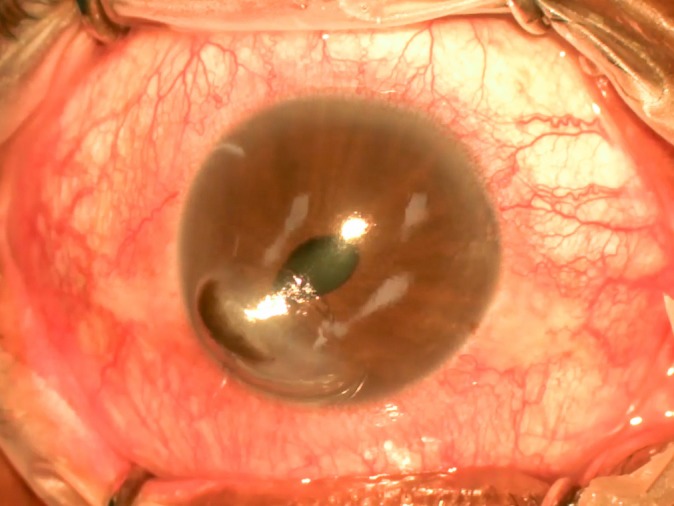
Right eye of a 43-year-old woman of African origin, presenting with a 10-day history of soreness, redness and loss of vision.
Investigations
The specific blood tests performed included a full blood count (reduced white cell and neutrophil count, as above), urea and electrolytes (normal), liver function tests (reduced albumin; 31 g/L (normal 35–50 g/L)), C-reactive protein (normal), rheumatoid factor (negative), anti-cyclic citrullinated peptide (negative), anti-nuclear antibody (negative), anti-neutrophil cytoplasmic antibody (c and p types) (negative), anti-double stranded DNA antibody (negative), syphilis serology (negative), hepatitis screen (negative), quantiferon (negative) and HIV antibodies (positive).
Outcome and follow-up
The patient was referred to the sexual health clinic and started on anti-retroviral treatment with abacavir/dolutegravir/lamivudine (brand name Triumeq). At the postoperative review 2 weeks after the surgery, the patient had a comfortable and uninflamed eye with no recurrence of their corneal melt. At most recent follow-up 3 months postoperatively, visual acuity was 6/36 unaided with a best corrected visual acuity of 6/12. The right eye remained uninflamed and the graft was healthy and clear (figure 2).
Figure 2.
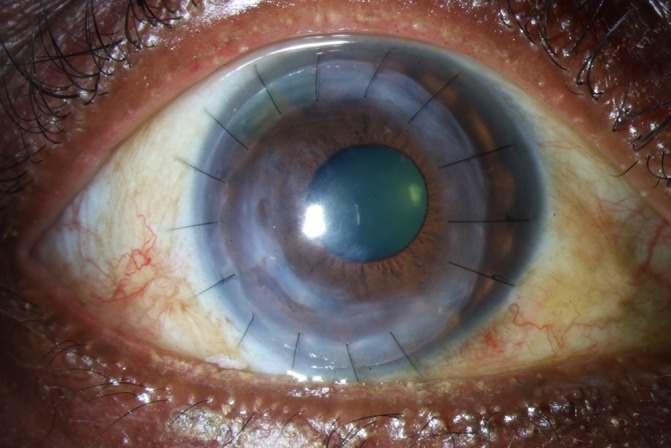
The right eye at 3-month review following tectonic deep anterior lamellar keratoplasty for peripheral ulcerative keratitis.
Discussion
This case highlights an interesting presentation of HIV in an otherwise asymptomatic patient and is the first report from the UK of PUK as the primary presentation of infection with HIV. The differential diagnosis of PUK includes other causes of peripheral corneal thinning. Peripheral corneal thinning is differentiated according to whether the eye is red and injected (inflamed) or white and ‘quiet’ (non-inflamed).1 It may be difficult to differentiate between these, and the opinion of an Ophthalmologist should be sought. Peripheral corneal thinning in an otherwise white eye, with no pain or inflammation, may be due to dellen, pellucid marginal degeneration or Terrien’s marginal degeneration. Dellen represent an area of corneal desiccation adjacent to an elevation on the ocular surface. Treatment includes lubrication. Pellucid marginal degeneration is a corneal ectasia, with irregular astigmatism secondary to inferior corneal thinning. Treatment includes rigid gas permeable contact lenses, collagen cross linking if there is progression or potentially corneal grafting if there is significant visual loss. Terrien’s marginal degeneration typically presents in middle-aged men, with a bilateral superior area of thinning with an intact epithelium. There is lipid at the edge of this thinning with a perilimbal clear zone of cornea.2 It can lead to against-the-rule astigmatism. Treatment involves correcting the refractive error.
Peripheral corneal thinning in an inflamed eye, which is injected, red and painful, may be the result of an infected corneal ulcer, marginal keratitis, PUK or Mooren’s ulcer. An infected corneal ulcer may have an associated hypopyon (pus inside the anterior chamber), a corneal scrape should be performed and topical antibiotics started. Marginal keratitis is a non-infectious inflammatory process as a result of a hypersensitivity reaction to toxins produced by bacteria, usually in association with longstanding staphylococcal blepharitis. The associated thinning and pain is less in these cases than with PUK or Mooren’s ulcer. PUK is an aggressive, potentially sight-threatening condition, with an overlying epithelial defect and progressive loss of corneal stroma.3 Mooren’s ulcer is considered a diagnosis of exclusion. It is an idiopathic form of PUK in which there is intolerable pain and the ulcer typically has an overhanging edge.4 5 In both PUK and Mooren’s, there is limbal involvement. Unlike PUK, there is no associated scleritis in Mooren’s ulcer.3 The features seen in our patient were more consistent with a diagnosis of PUK (figure 1).
The exact pathogenesis of PUK remains unclear. Both humoral-mediated and cell-mediated immune processes have been implicated,3 leading to immune complex deposition at the limbus. This results in corneal inflammation leading to the characteristic stromal melt of PUK.6 Rheumatoid arthritis is the most common cause of PUK. The mortality rate in untreated rheumatoid arthritis patients with PUK is reported to be 50% over a 10-year period.7 Therefore, it is vital that such cases are identified and appropriately managed in a multi-disciplinary manner. Other non-infectious causes include, granulomatosis with polyangiitis, systemic lupus erythematous, relapsing polychondritis, polyarteritis nodosa, microscopica polyangiitis and Churg-Strauss syndrome. Infectious causes may include herpes zoster, tuberculosis, syphilis, Lyme disease, gonorrhoea, hepatitis and as was the case with our patient, HIV. Careful history and systemic review should be taken. Blood investigations include full blood count, urea and electrolytes, liver function test, glucose, c-reactive protein, erythrocyte sedimentation rate, vasculitis screen (including rheumatoid factor, anti-CCP, anti-nuclear antibody, anti-neutrophil cytoplasmic antibody (c and p types), anti-double stranded DNA antibody). Infectious screening may include syphilis serology, lyme serology, hepatitis screen and HIV antibodies. Urinalysis, blood pressure and chest X-ray may also be useful.
Our patient was in apparent good health. No risk factors for HIV infection were identified from the patient’s medical or social history. Two case reports from India have reported PUK to occur as the primary presentation of HIV infection.8 9 HIV vasculopathy may result in an immune complex-mediated process,10 which if occurring at the corneal limbus, may result in PUK. Interestingly, Mooren’s ulcer has been reported to occur in a case of treatment-related immune reconstitution inflammatory syndrome associated with the initiation of HIV treatment.11 Our case is to the best of our knowledge the first report from the UK of PUK with corneal perforation as the primary presentation of HIV infection.
In all cases of PUK, same day referral to a corneal specialist is indicated. Multi-disciplinary management should involve the patient’s physician and Rheumatologist if there is a non-infectious systemic cause. Treatment includes ocular and systemic therapy and surgery is potentially required in advanced cases. Ocular treatment options include preservative free lubricants, punctual occlusion and prophylactic topical antibiotics (such as preservative free topical levofloxacin 0.5% four times daily) to prevent any secondary infection. Topical corticosteroids inhibit new collagen production and may increase the progression of keratolysis and perforation in PUK. The general consensus is that the use of topical corticosteroids topically should be avoided in PUK.3 Systemic management depends on the underlying diagnosis, thus it is vital that infectious causes are first excluded. Non-infectious causes of PUK require systemic immunosuppression. This is typically with 3 days of pulsed intravenous methylprednisolone at a dose of 500–1000 mg per day, or high dose oral prednisolone (60 mg/day), followed by a tapering course of oral prednisolone based on the clinical response. Systemic immunosuppression with a second line agent should be considered, as discussed further in a review article.12 If however, an infectious cause is identified, as with our patient, immunosuppressive treatment should be avoided, and the underlying infection treated. The two reported cases of PUK as the first presentation of HIV infection,8 9 did not have corneal perforation and were successfully managed non-surgically. In cases such as ours that present with corneal perforation, surgical management is required. Options include; therapeutic bandage contact lenses and cyanoacrylate glue as a temporising measure, conjunctival flaps, amniotic membrane grafts, or if there is a large perforation with significant iris protrusion, repositioning of the iris and a tectonic corneal graft may be required (figure 2).
This case is to the best of our knowledge the first report from the UK of PUK with corneal perforation as the primary presentation of HIV infection. As demonstrated by our patient, this infection may be silent; therefore, it is vital to consider HIV when dealing with PUK of unknown aetiology.
Learning points.
Peripheral corneal thinning associated with scleritis and stromal melt are the features of peripheral ulcerative keratitis (PUK). Such cases require urgent same day review by an ophthalmologist.
PUK may be the presenting feature of a potentially life-threatening systemic disease. Systemic causes may be infectious or non-infectious. PUK may precede the diagnosis of the systemic condition and therefore it is vital that these cases are urgently investigated.
As demonstrated by our patient, infection with HIV may be initially silent; therefore, it is vital to consider HIV when dealing with PUK of unknown aetiology.
Footnotes
Contributors: All authors contributed to this article. ST - Wrote and edited the manuscript. DG - Assisted with editing. DT - Assisted with editing. KD - Assisted with editing, performed surgery for the patient.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1.Mondino BJ. Inflammatory diseases of the peripheral cornea. Ophthalmology 1988;95:463–72. 10.1016/S0161-6420(88)33164-7 [DOI] [PubMed] [Google Scholar]
- 2.Keenan JD, Mandel MR, Margolis TP. Peripheral ulcerative keratitis associated with vasculitis manifesting asymmetrically as fuchs superficial marginal keratitis and terrien marginal degeneration. Cornea 2011;30:825–7. 10.1097/ICO.0b013e3182000c94 [DOI] [PubMed] [Google Scholar]
- 3.Yagci A. Update on peripheral ulcerative keratitis. Clin Ophthalmol 2012;6:747–54. 10.2147/OPTH.S24947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Srinivasan M, Zegans ME, Zelefsky JR, et al. . Clinical characteristics of Mooren’s ulcer in South India. Br J Ophthalmol 2007;91:570–5. 10.1136/bjo.2006.105452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seino JY, Anderson SF. Mooren’s Ulcer. Optom Vis Sci 1998:783–90. [DOI] [PubMed] [Google Scholar]
- 6.Dana MR, Qian Y, Hamrah P. Twenty-five-year panorama of corneal immunology: emerging concepts in the immunopathogenesis of microbial keratitis, peripheral ulcerative keratitis, and corneal transplant rejection. Cornea 2000;19:625–43. [DOI] [PubMed] [Google Scholar]
- 7.Foster CS, Forstot SL, Wilson LA. Mortality rate in rheumatoid arthritis patients developing necrotizing scleritis or peripheral ulcerative keratitis. Effects of systemic immunosuppression. Ophthalmology 1984;91:1253–63. 10.1016/S0161-6420(84)34160-4 [DOI] [PubMed] [Google Scholar]
- 8.Soni ND, Ingole AB, Murade SM. An unusual case of peripheral ulcerative keratitis as a presenting feature in an otherwise healthy patient with undiagnosed human immunodeficiency virus infection and low CD4 counts. Indian J Ophthalmol 2013;61:138–9. 10.4103/0301-4738.109391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gharai S, Venkatesh P, Tandon R, et al. . Peripheral ulcerative keratitis and central retinal vein occlusion as the initial manifestation of HIV infection. Ocul Immunol Inflamm 2007;15:407–9. 10.1080/09273940701572404 [DOI] [PubMed] [Google Scholar]
- 10.Chetty R. Vasculitides associated with HIV infection. J Clin Pathol 2001;54:275–8. 10.1136/jcp.54.4.275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Du Toit SH, Smit DP. Mooren’s ulcer of the cornea after immune reconstitution. AIDS 2014;28:139–40. 10.1097/QAD.0000000000000044 [DOI] [PubMed] [Google Scholar]
- 12.Jabs DA, Rosenbaum JT, Foster CS, et al. . Guidelines for the use of immunosuppressive drugs in patients with ocular inflammatory disorders: recommendations of an expert panel. Am J Ophthalmol 2000;130:492–513. 10.1016/S0002-9394(00)00659-0 [DOI] [PubMed] [Google Scholar]


