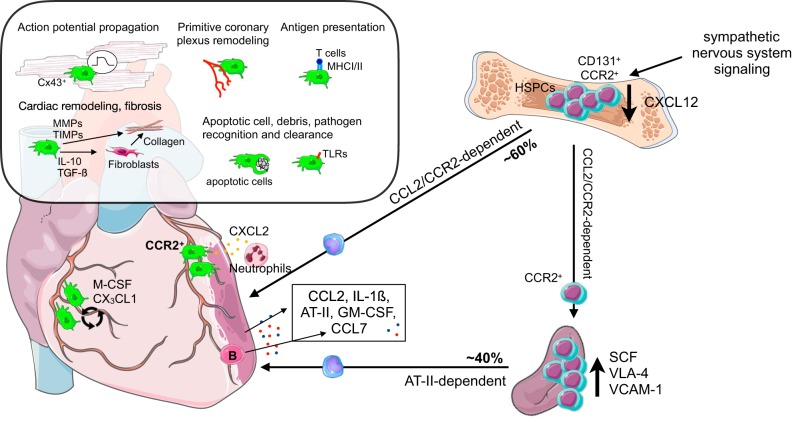
FIGURE 4.
Macrophage origin and function in the steady-state and inflamed heart. Cardiac macrophage ontogeny and function during steady state and inflammation are depicted in the inset. For simplicity, only the role of macrophages is depicted. Macrophage turnover in the heart is governed by macrophage-colony-stimulating factor (M-CSF) and CX3CL1. A variety of soluble factors are increased in circulation after myocardial infarction, listed in the box, which result in monocyte recruitment and further increase hematopoiesis, in addition to autonomic signaling. Proliferation and differentiation of CD131+ and CCR2+ hematopoietic stem and progenitors cells (HSPCs) is increased in the bone marrow. A decrease of retention factors, for example, CXCL12, allows for mobilization of CCR2+ HSPCs to the spleen, where they are retained, for example, via vascular cell adhesion molecule 1 (VCAM-1), and further proliferate and differentiate. Monocyte release from the bone marrow is CCL2/CCR2 dependent, while release from the spleen is angiotensin II dependent. Percentages indicate contribution of bone marrow and spleen to monocytes recruited to the infarct area. CCR2+ macrophages have been indicated to recruit neutrophils, whereas B cells were found to recruit monocytes via CCL7. AT-II, angiotensin II; Cx, connexin; M-CSF, macrophage-colony-stimulating factor; MHC, major histocompatibility complex; MMPs, matrix metalloproteinases; TIMPs, tissue inhibitors of matrix metalloproteinases; TLRs, Toll-like receptors.